Atelectasis: Difference between revisions
Areeba Raja (talk | contribs) No edit summary |
mNo edit summary |
||
| (9 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor''' - [[User:Hing Long Yip|Hing Long Yip]] | '''Original Editor''' - [[User:Hing Long Yip|Hing Long Yip]] | ||
| Line 10: | Line 7: | ||
== Introduction == | == Introduction == | ||
[[File:Atelectasis Normal vs Affected Airway.jpeg|right|frameless|400x400px]] | [[File:Atelectasis Normal vs Affected Airway.jpeg|right|frameless|400x400px]] | ||
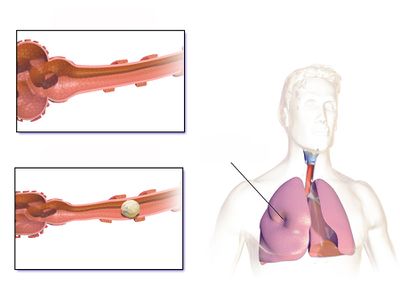
Atelectasis is a condition in which | Atelectasis is a condition in which there is collapse of [[Lung Anatomy|lung]] tissue ([https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3929318/ parenchyma]) with loss of volume. The word "parenchyma" signifies the functional units, the alveoli, of the lungs. Atelectasis describes involvement of relatively smaller units (of alveoli). When larger units of lung parenchyma is involved it is called "collapse" (or collapsed lung), which is essentially just a larger atelectasis. Atelectasis does not involve the airways. | ||
The loss of volume leads to an impaired gaseous exchange between CO2 and O2. It is a reversible condition and usually occurs secondary to an underlying pathology.<ref name=":2">Peroni DG, Boner AL. [https://pubmed.ncbi.nlm.nih.gov/12531090/ Atelectasis: mechanisms, diagnosis and management]. Paediatr Respir Rev. 2000;1:274-8.</ref><ref name=":4">Grott K, Dunlap JD. [https://www.ncbi.nlm.nih.gov/books/NBK545316/#!po=10.0000 Atelectasis]. StatPearls [Internet]. 2020 Aug 10.Available from: https://www.ncbi.nlm.nih.gov/books/NBK545316/#!po=10.0000 (accessed 18.4.2021)</ref> | |||
| Line 17: | Line 17: | ||
* Atelectasis does not preferentially affect either sex. | * Atelectasis does not preferentially affect either sex. | ||
* Incidence doesn't increase in patient with increased age, [[COPD (Chronic Obstructive Pulmonary Disease)|COPD]] or [[asthma]]. | * Incidence doesn't increase in patient with increased age, [[COPD (Chronic Obstructive Pulmonary Disease)|COPD]] or [[asthma]]. | ||
* The incidence of atelectasis in patients who have recently undergone general anesthesia is as high as 90% | * The incidence of atelectasis in patients who have recently undergone general anesthesia is as high as 90%<ref>Hedenstierna G, Tokics L, Reinius H, Rothen HU, Östberg E, Öhrvik J. Higher age and obesity limit atelectasis formation during anaesthesia: an analysis of computed tomography data in 243 subjects. British journal of anaesthesia. [https://www.sciencedirect.com/science/article/pii/S0007091219309304 2020 Mar 1;124(3):336-44.]</ref>, with up to 20 - 25% of normal lung noted to be either poorly aerated or atelectatic on CT during anesthesia<ref>Reber A, Engberg G, Sporre B, Kviele L, Rothen HU, Wegenius G, Nylund U, Hedenstierna G. Volumetric analysis of aeration in the lungs during general anaesthesia. British journal of anaesthesia. 1996 Jun [https://academic.oup.com/bja/article/76/6/760/346151 1;76(6):760-6.]</ref> | ||
* It is commonly observed as a complication in [[Post-Operative Pulmonary Complication|post-operative]] patients whose breathing mechanism is impacted by the procedure, [[Pain Mechanisms|pain]], and prolonged resting. | * It is commonly observed as a complication in [[Post-Operative Pulmonary Complication|post-operative]] patients whose breathing mechanism is impacted by the procedure, [[Pain Mechanisms|pain]], and prolonged resting. | ||
* Atelectasis is less commonly seen in patients with conditions like [[COPD (Chronic Obstructive Pulmonary Disease)|COPD]], [[bronchiectasis]], and [[Cystic Fibrosis|cystic fibrosis]]. | * Atelectasis is less commonly seen in patients with conditions like [[COPD (Chronic Obstructive Pulmonary Disease)|COPD]], [[bronchiectasis]], and [[Cystic Fibrosis|cystic fibrosis]]. | ||
* Cephalad displacement of the diaphragm in [[Obesity|Obese]] and/or pregnant patients is more likely to cause atelectasis.<ref name=":4" /> | * Cephalad displacement of the diaphragm in [[Obesity|Obese]] and/or pregnant patients is more likely to cause atelectasis.<ref name=":4" />Atelectasis was found to increase with an increase in BMI for both normal and overweight patients<ref>Hedenstierna G, Tokics L, Reinius H, Rothen HU, Östberg E, Öhrvik J. Higher age and obesity limit atelectasis formation during anaesthesia: an analysis of computed tomography data in 243 subjects. British journal of anaesthesia : [https://www.sciencedirect.com/science/article/pii/S0007091219309304 BJA. 2020;124(3):336–44.] </ref>. | ||
== Classification == | == Classification == | ||
It can be classified as follows<ref name=":5">Stark P. [http://publishingimages.s3.amazonaws.com/eZineImages/PracticePerfect/715/Atelectasis-Types-and-pathogenesis-in-adults-UpToDate.pdf Atelectasis: Types and pathogenesis in adults] [Internet]. 2020. </ref> | It can be classified as follows<ref name=":5">Stark P. [http://publishingimages.s3.amazonaws.com/eZineImages/PracticePerfect/715/Atelectasis-Types-and-pathogenesis-in-adults-UpToDate.pdf Atelectasis: Types and pathogenesis in adults] [Internet]. 2020. </ref> | ||
# pathophysiological mechanism (e.g., compressive atelectasis, absorption atelectasis, surfactant impairment atelectasis) | |||
# the amount of lung involved (e.g., lobar, segmental, or subsegmental atelectasis) | |||
# the location (i.e., specific lobe or segment location). | |||
=== | === Pathophysiology === | ||
Following table comprises the classification of atelectasis based on pathophysiologic mechanism<ref name=":2" /><ref name=":4" /><ref name=":5" /><ref>Raman TS, Mathew S, Garcha PS. [https://pubmed.ncbi.nlm.nih.gov/10216624/ Atelectasis in children.] Indian pediatrics. 1998 May;35(5):429-35.</ref><ref>Culiner MM. [https://pubmed.ncbi.nlm.nih.gov/5947916/ The right middle lobe syndrome, a non-obstructive complex.] Diseases of the Chest. 1966; 50(1):57-66.</ref><ref>Sutnick AI, Soloff LA. [https://pubmed.ncbi.nlm.nih.gov/14104855/ Atelectasis with pneumonia: a pathophysiologic study.] Annals of internal medicine. 1964;60:39-46.</ref><ref>Magnusson L, Spahn DR. "[https://pubmed.ncbi.nlm.nih.gov/12821566/ New concepts of atelectasis during general anaesthesia.]" BR J Anaesth. 2003;91.1: 61-72.</ref><ref>Woodring J H, & Reed JC . [https://pubmed.ncbi.nlm.nih.gov/8820021/ Types and mechanisms of pulmonary atelectasis]. J Thorac Imag 1996;11:92-108''.''</ref><ref>Nazir A Lone, MD, MBBS, MPH, FACP, FCCP. [https://emedicine.medscape.com/article/1001160-clinical#showall Pulmonary Atelectasis Clinical Presentation: History, Physical, Causes] [Internet]. Medscape.com. Medscape; 2020 [cited 2021 Nov 19]. </ref><ref>Duggan M, Kavanagh Brian P, Warltier David C. [https://watermark.silverchair.com/0000542-200504000-00021.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAvkwggL1BgkqhkiG9w0BBwagggLmMIIC4gIBADCCAtsGCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQM1M0kQp1WSf9k3E1pAgEQgIICrLMn-sN1G756LQkSnJ_jRLF23z5xUtHzyRTvKKqa6S2JY74yR68UsnLh8BNiq5XazGaZmYCwX6jMqwhqGyXljP8w9iRmCqNG3VAPCNodaTv3AZ5C3WwjFWriShxwo2TGcwzS-OZ3peld3sILyDNKQbB_6uqtsYSKhOFpvx9EPgG030EMF5Dy3_frh4odd-wqYniZRDycQTGWXI2fafXX6b3bnOyxguU6PHdRpk2vz6278whwwmYxqVo9qHmM0N1xCMiU4ug-ZSvqbKDzLX-ogkLQnglLya866_RflkevOGtSMVTyTKY7DH15zsIUQwHI2idz3hV1r8C64XLsgV8QmoRJ7XAZ8RLGtjmfHEBq07iieihFK2y22aUH4JMzbk1ocI-xI0k5yFDJylttJ2xZK-AzaZlgdUENRb1z_Oeb-ZwCH2dhdZmbSsoxgnn1kF5uKQOhEQHuyU93f91F9F_Nn2G7BR4EV6zRSGKj1RJQz76TUMwX8uF5VogWIu2ifSLEqP15sRuioXrJ5S30L7nEd9BO-WDuNsrITy8Q-NlOKaQgcgi2Souw6eNgAW9E_CabAoaOohLFhJViafBXNCJklI1xCW5oefxrJvZmagpMfCfbK3GOd5kBAyhGvsHEWZf5JKsODwgYUhO1yyy9IZQABb0kPrQY7EFOaqaqPCxh05GTpc2MLqZmtVXIoPRaxcLNAhV3Ftbhau8sQ48Z0uHBNbErgIBG_lhnnwb4yadf950l9UWb55kyJZOUFP_zXkuBknMkCoDl8I2XLkcr7tIVo4fX_Nxa15wRKjFbzyoUF8BMzOQRrBsYdcwS9-rLE7T1xCrrUgqZVQ_S2jOW_U4EfeALlCJz_YBOxa7gIzoDfAX6zOHPoxJHQb5bEEbij3GcBdM1X-IDIl5l7np8wA Pulmonary Atelectasis. Anesthesiology] [Internet]. 2005 Apr 1 [cited 2021 Nov 19];102(4):838–54.</ref><ref>Priftis KN, Rubin B. [https://www.semanticscholar.org/paper/Atelectasis%2C-Middle-Lobe-Syndrome-and-Plastic-Priftis-Rubin/7f3852fc6ba113a1c95e1d7166ff58e02dda16c3 Atelectasis, Middle Lobe Syndrome and Plastic Bronchitis]. Paediatric Bronchoscopy [Internet]. 2010 [cited 2021 Nov 20];149–55. </ref><ref name=":6">Ray K, Bodenham A, Paramasivam E. [https://academic.oup.com/bjaed/article/14/5/236/286828 Pulmonary atelectasis in anaesthesia and critical care.] Continuing Education in Anaesthesia Critical Care & Pain [Internet]. 2014 Oct [cited 2021 Nov 19];14(5):236–45. </ref><ref>Domino KB. [https://watermark.silverchair.com/20191000_0-00012.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAucwggLjBgkqhkiG9w0BBwagggLUMIIC0AIBADCCAskGCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQMxYo4pkl59eKRPec3AgEQgIICmnv-XL-UKZ_D6uk8clbSqJAlFrh4vk2w2BuKeobo1Ng230DAe5scvejktVy0eBEsTX7F2SEyCxulihfxY9rz1UnuccPznOO9fBYCS_C5tcdbMZrgUWkO2YFRhlxSWFAGjj8XyR4VpDYUjQvqfj6mI99wQtGhFS0CTq2pMLF9xIAXwicIqAve6xnXzS3W2mynrcvlc3jQjWJ5r0g4OO_tVSVDlNPwS_3wddv0kpYU-3KfPgABC_toy4iszzDTqepWt9RA3e5W8GDQKI3pYpTG36IwBBROKE6falj64kvO_51QM9OyMjh0zruZlxYpD8i4SrcBabJqChJ4quLWjoqn3GuQfrWz0IVcnVPSQqmWM-UJRdEwB5Ll7eaNQ3vRUke8nuc7zgOfErwmHfikUsBCKCIjKMaVpUnMmXHbN_01vfVxKOfkIYZoOvvmFB8a6Rdiow7xLyuz__wMqmjKrpfg6-svS7id6_ei-5vEA--NKpbV3Jm8_h-sQQvv0kbWq2WEBDc5e2kGgv-1_jtqxcqTQ6iZANE_HzL413E10pfDIGpgjGDYF_WyLP3rgPohgWzg6l_mFqDN8LMqZzSp2DgmCljEdG51RSCmXdotJgNz8Dazl9NTX5Ai6YgMLOpIBjwcfzAkcvY3lhAS3TLqVVRdew11iXJDJMYAZAjznZE3idCZI4iRUwXTKVID3JxOcF95BRV9zE8DDKJBGjWLlAqqttae_hROsZSdYMil2qhzutMs35K4sjKoGaYxKDgJWTdEYvWBoI58UqPlFos2RHDEgUEIjowRCHf6UtQACovkZJmMldkoGyKFTD64leG4Eg4Jrr0Qta85vTu-Mh7l-KQFiRH7MHoQpgWwlhxtjKiLzPF8Va-oItrjSirgSQ Pre-emergence Oxygenation and Postoperative Atelectasis.] Anesthesiology [Internet]. 2019 Oct 1 [cited 2021 Nov 20];131(4):771–3. </ref><ref>Kavanagh BP. [https://www.minervamedica.it/en/getfreepdf/TnpVang3bXVBU1JPeVdsTU1BY3Y0V3pMblJrS2VZZFE4UjBNd3JJZW0rY09xclZ3bFhzdnBsdmptWjdpRzFZUA%253D%253D/R02Y2008N06A0285.pdf Perioperative atelectasis.] Minerva anestesiologica [Internet]. 2021 [cited 2021 Nov 19];74(6).</ref><ref name=":7">Restrepo RD, Braverman J. [https://www.tandfonline.com/doi/pdf/10.1586/17476348.2015.996134?needAccess=true Current challenges in the recognition, prevention and treatment of perioperative pulmonary atelectasis.] Expert Review of Respiratory Medicine [Internet]. 2014 Dec 26 [cited 2021 Nov 19];9(1):97–107. </ref><ref>Johnston C, Carvalho WB de. [https://pubmed.ncbi.nlm.nih.gov/18989568/ Atelectasias em pediatria: mecanismos, diagnóstico e tratamento. Revista da Associação Médica Brasileira] [Internet]. 2008 Oct [cited 2021 Nov 19];54(5). </ref><ref>Atağ E. [https://jag.journalagent.com/hnhjournal/pdfs/HNHJ_61_2_139_144.pdf Etiology, diagnosis and treatment in childhood atelectasis.] Haydarpasa Numune Training and Research Hospital Medical Journal [Internet]. 2020 [cited 2021 Nov 19]; Available from: <nowiki>https://jag.journalagent.com/hnhjournal/pdfs/HNHJ_61_2_139_144.pdf</nowiki></ref><ref>Navas-Blanco JR, Dudaryk R. [https://link.springer.com/content/pdf/10.1186/s12871-020-01095-7.pdf Management of Respiratory Distress Syndrome due to COVID-19 infection.] BMC Anesthesiology [Internet]. 2020 Jul 20 [cited 2021 Nov 20];20(1). </ref><ref>WRIGHT WR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1591744/pdf/canmedaj00642-0021.pdfhttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC1591744/pdf/canmedaj00642-0021.pdf Atelectasis.] Canadian Medical Association journal [Internet]. 2021 [cited 2021 Nov 20];62(3).</ref> | Following table comprises the classification of atelectasis based on pathophysiologic mechanism<ref name=":2" /><ref name=":4" /><ref name=":5" /><ref>Raman TS, Mathew S, Garcha PS. [https://pubmed.ncbi.nlm.nih.gov/10216624/ Atelectasis in children.] Indian pediatrics. 1998 May;35(5):429-35.</ref><ref>Culiner MM. [https://pubmed.ncbi.nlm.nih.gov/5947916/ The right middle lobe syndrome, a non-obstructive complex.] Diseases of the Chest. 1966; 50(1):57-66.</ref><ref>Sutnick AI, Soloff LA. [https://pubmed.ncbi.nlm.nih.gov/14104855/ Atelectasis with pneumonia: a pathophysiologic study.] Annals of internal medicine. 1964;60:39-46.</ref><ref>Magnusson L, Spahn DR. "[https://pubmed.ncbi.nlm.nih.gov/12821566/ New concepts of atelectasis during general anaesthesia.]" BR J Anaesth. 2003;91.1: 61-72.</ref><ref>Woodring J H, & Reed JC . [https://pubmed.ncbi.nlm.nih.gov/8820021/ Types and mechanisms of pulmonary atelectasis]. J Thorac Imag 1996;11:92-108''.''</ref><ref>Nazir A Lone, MD, MBBS, MPH, FACP, FCCP. [https://emedicine.medscape.com/article/1001160-clinical#showall Pulmonary Atelectasis Clinical Presentation: History, Physical, Causes] [Internet]. Medscape.com. Medscape; 2020 [cited 2021 Nov 19]. </ref><ref>Duggan M, Kavanagh Brian P, Warltier David C. [https://watermark.silverchair.com/0000542-200504000-00021.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAvkwggL1BgkqhkiG9w0BBwagggLmMIIC4gIBADCCAtsGCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQM1M0kQp1WSf9k3E1pAgEQgIICrLMn-sN1G756LQkSnJ_jRLF23z5xUtHzyRTvKKqa6S2JY74yR68UsnLh8BNiq5XazGaZmYCwX6jMqwhqGyXljP8w9iRmCqNG3VAPCNodaTv3AZ5C3WwjFWriShxwo2TGcwzS-OZ3peld3sILyDNKQbB_6uqtsYSKhOFpvx9EPgG030EMF5Dy3_frh4odd-wqYniZRDycQTGWXI2fafXX6b3bnOyxguU6PHdRpk2vz6278whwwmYxqVo9qHmM0N1xCMiU4ug-ZSvqbKDzLX-ogkLQnglLya866_RflkevOGtSMVTyTKY7DH15zsIUQwHI2idz3hV1r8C64XLsgV8QmoRJ7XAZ8RLGtjmfHEBq07iieihFK2y22aUH4JMzbk1ocI-xI0k5yFDJylttJ2xZK-AzaZlgdUENRb1z_Oeb-ZwCH2dhdZmbSsoxgnn1kF5uKQOhEQHuyU93f91F9F_Nn2G7BR4EV6zRSGKj1RJQz76TUMwX8uF5VogWIu2ifSLEqP15sRuioXrJ5S30L7nEd9BO-WDuNsrITy8Q-NlOKaQgcgi2Souw6eNgAW9E_CabAoaOohLFhJViafBXNCJklI1xCW5oefxrJvZmagpMfCfbK3GOd5kBAyhGvsHEWZf5JKsODwgYUhO1yyy9IZQABb0kPrQY7EFOaqaqPCxh05GTpc2MLqZmtVXIoPRaxcLNAhV3Ftbhau8sQ48Z0uHBNbErgIBG_lhnnwb4yadf950l9UWb55kyJZOUFP_zXkuBknMkCoDl8I2XLkcr7tIVo4fX_Nxa15wRKjFbzyoUF8BMzOQRrBsYdcwS9-rLE7T1xCrrUgqZVQ_S2jOW_U4EfeALlCJz_YBOxa7gIzoDfAX6zOHPoxJHQb5bEEbij3GcBdM1X-IDIl5l7np8wA Pulmonary Atelectasis. Anesthesiology] [Internet]. 2005 Apr 1 [cited 2021 Nov 19];102(4):838–54.</ref><ref>Priftis KN, Rubin B. [https://www.semanticscholar.org/paper/Atelectasis%2C-Middle-Lobe-Syndrome-and-Plastic-Priftis-Rubin/7f3852fc6ba113a1c95e1d7166ff58e02dda16c3 Atelectasis, Middle Lobe Syndrome and Plastic Bronchitis]. Paediatric Bronchoscopy [Internet]. 2010 [cited 2021 Nov 20];149–55. </ref><ref name=":6">Ray K, Bodenham A, Paramasivam E. [https://academic.oup.com/bjaed/article/14/5/236/286828 Pulmonary atelectasis in anaesthesia and critical care.] Continuing Education in Anaesthesia Critical Care & Pain [Internet]. 2014 Oct [cited 2021 Nov 19];14(5):236–45. </ref><ref>Domino KB. [https://watermark.silverchair.com/20191000_0-00012.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAucwggLjBgkqhkiG9w0BBwagggLUMIIC0AIBADCCAskGCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQMxYo4pkl59eKRPec3AgEQgIICmnv-XL-UKZ_D6uk8clbSqJAlFrh4vk2w2BuKeobo1Ng230DAe5scvejktVy0eBEsTX7F2SEyCxulihfxY9rz1UnuccPznOO9fBYCS_C5tcdbMZrgUWkO2YFRhlxSWFAGjj8XyR4VpDYUjQvqfj6mI99wQtGhFS0CTq2pMLF9xIAXwicIqAve6xnXzS3W2mynrcvlc3jQjWJ5r0g4OO_tVSVDlNPwS_3wddv0kpYU-3KfPgABC_toy4iszzDTqepWt9RA3e5W8GDQKI3pYpTG36IwBBROKE6falj64kvO_51QM9OyMjh0zruZlxYpD8i4SrcBabJqChJ4quLWjoqn3GuQfrWz0IVcnVPSQqmWM-UJRdEwB5Ll7eaNQ3vRUke8nuc7zgOfErwmHfikUsBCKCIjKMaVpUnMmXHbN_01vfVxKOfkIYZoOvvmFB8a6Rdiow7xLyuz__wMqmjKrpfg6-svS7id6_ei-5vEA--NKpbV3Jm8_h-sQQvv0kbWq2WEBDc5e2kGgv-1_jtqxcqTQ6iZANE_HzL413E10pfDIGpgjGDYF_WyLP3rgPohgWzg6l_mFqDN8LMqZzSp2DgmCljEdG51RSCmXdotJgNz8Dazl9NTX5Ai6YgMLOpIBjwcfzAkcvY3lhAS3TLqVVRdew11iXJDJMYAZAjznZE3idCZI4iRUwXTKVID3JxOcF95BRV9zE8DDKJBGjWLlAqqttae_hROsZSdYMil2qhzutMs35K4sjKoGaYxKDgJWTdEYvWBoI58UqPlFos2RHDEgUEIjowRCHf6UtQACovkZJmMldkoGyKFTD64leG4Eg4Jrr0Qta85vTu-Mh7l-KQFiRH7MHoQpgWwlhxtjKiLzPF8Va-oItrjSirgSQ Pre-emergence Oxygenation and Postoperative Atelectasis.] Anesthesiology [Internet]. 2019 Oct 1 [cited 2021 Nov 20];131(4):771–3. </ref><ref>Kavanagh BP. [https://www.minervamedica.it/en/getfreepdf/TnpVang3bXVBU1JPeVdsTU1BY3Y0V3pMblJrS2VZZFE4UjBNd3JJZW0rY09xclZ3bFhzdnBsdmptWjdpRzFZUA%253D%253D/R02Y2008N06A0285.pdf Perioperative atelectasis.] Minerva anestesiologica [Internet]. 2021 [cited 2021 Nov 19];74(6).</ref><ref name=":7">Restrepo RD, Braverman J. [https://www.tandfonline.com/doi/pdf/10.1586/17476348.2015.996134?needAccess=true Current challenges in the recognition, prevention and treatment of perioperative pulmonary atelectasis.] Expert Review of Respiratory Medicine [Internet]. 2014 Dec 26 [cited 2021 Nov 19];9(1):97–107. </ref><ref>Johnston C, Carvalho WB de. [https://pubmed.ncbi.nlm.nih.gov/18989568/ Atelectasias em pediatria: mecanismos, diagnóstico e tratamento. Revista da Associação Médica Brasileira] [Internet]. 2008 Oct [cited 2021 Nov 19];54(5). </ref><ref>Atağ E. [https://jag.journalagent.com/hnhjournal/pdfs/HNHJ_61_2_139_144.pdf Etiology, diagnosis and treatment in childhood atelectasis.] Haydarpasa Numune Training and Research Hospital Medical Journal [Internet]. 2020 [cited 2021 Nov 19]; Available from: <nowiki>https://jag.journalagent.com/hnhjournal/pdfs/HNHJ_61_2_139_144.pdf</nowiki></ref><ref>Navas-Blanco JR, Dudaryk R. [https://link.springer.com/content/pdf/10.1186/s12871-020-01095-7.pdf Management of Respiratory Distress Syndrome due to COVID-19 infection.] BMC Anesthesiology [Internet]. 2020 Jul 20 [cited 2021 Nov 20];20(1). </ref><ref>WRIGHT WR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1591744/pdf/canmedaj00642-0021.pdfhttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC1591744/pdf/canmedaj00642-0021.pdf Atelectasis.] Canadian Medical Association journal [Internet]. 2021 [cited 2021 Nov 20];62(3).</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 42: | Line 40: | ||
|- | |- | ||
|Compression of Lung Tissue | |Compression of Lung Tissue | ||
| | |When there is an imbalance of net forces across an alveolar wall, it causes the alveoli to collapse. this mechanism of atelectasis causes the lung tissue to compress. | ||
| | | | ||
* Passive Atelectasis | * Passive Atelectasis | ||
| Line 49: | Line 47: | ||
* Airway Stenosis | * Airway Stenosis | ||
* Inflammation and edema caused by aspiration or inhalation injury (smoke, chemical agents) | * Inflammation and edema caused by aspiration or inhalation injury (smoke, chemical agents) | ||
* [[ | * [[Oedema Assessment|Edema]] of the airway | ||
* Bronchial tumor | * Bronchial tumor | ||
* Granuloma | * Granuloma | ||
| Line 66: | Line 64: | ||
|A second major reason is gas resorption. This may occur in two ways. | |A second major reason is gas resorption. This may occur in two ways. | ||
* If | * If there is a complete occlusion of the airway, the alveolar gas can only exit via the bloodstream and not the alveolar unit, this obstruction can cause atelectasis. | ||
* The second and perhaps more important mechanism of gas resorption may occur in areas | * The second and perhaps more important mechanism of gas resorption may occur due to the ventilation/perfusion mismatch in certain areas of the lung. If the alveolar oxygen increases because of the increased inspired oxygen concentration and the nitrogen does not, uptake will be high resulting in less alveolar splinting and decreased lung volume. | ||
| | | | ||
* Obstructive Atelectasis | * Obstructive Atelectasis | ||
| Line 83: | Line 81: | ||
|- | |- | ||
|Impairment of Surfactant Function | |Impairment of Surfactant Function | ||
| | |Deficiency of acquired dysfunction(e . g ., for premature neonates) can result in lacking surfactant capacity. Surfactant reduces alveolar surface tension, stabilising the alveoli and preventing collapse. When inactivated, decreased expansion of the alveoli can occur as a result of increased local surface tension causing a reduction in resting lung volume globally. | ||
| | | | ||
* Adhesive atelectasis | * Adhesive atelectasis | ||
| Line 97: | Line 95: | ||
{{#ev:youtube|watch?v=gjLCu8qe2nI&ab_channel=NinjaNerdLectures}}<ref>reference</ref> | {{#ev:youtube|watch?v=gjLCu8qe2nI&ab_channel=NinjaNerdLectures}}<ref>reference</ref> | ||
=== | === Patterns of Collapse === | ||
Atelectasis can be classified on the basis of location according to radiological patterns of collapse<ref name=":6" /> | Atelectasis can be classified on the basis of location according to radiological patterns of collapse<ref name=":6" />. | ||
==== Complete | ==== Complete Collapse ==== | ||
The | The white out (complete opacification of a hemithorax) can be seen in complete lung collapse. This appearance can be confused with a large [[Pleural Effusion|pleural effusion]], but the mediastinal shift towards a collapsed lung can distinguish it from pleural effusion where the shift is in the opposite direction of the pathology. | ||
==== Lobar | ==== Lobar Collapse ==== | ||
Characteristic features associated with individual lobar collapse are as follows: | Characteristic features associated with individual lobar collapse are as follows: | ||
===== Right upper lobe (RUL) collapse ===== | ===== Right upper lobe (RUL) collapse ===== | ||
* | * Elevation of the right hilum | ||
* | * Elevation of the minor fissure. | ||
* Golden S sign(The minor fissure is usually convex superiorly but may appear concave because of an underlying mass lesion). | * Minor and major fissures may be visible on the lateral view. | ||
* Golden S sign is present (The minor fissure is usually convex superiorly but may appear concave because of an underlying mass lesion). | |||
===== Right middle lobe (RML) collapse ===== | ===== Right middle lobe (RML) collapse ===== | ||
* | * Results in minimal opacity and is often overlooked. | ||
* | * In a posterior -anterior view, the loss of silhouette of the right heart border can be seen. | ||
* | * A wedge-shaped opacity can be seen on the lateral view as the result of right horizontal and oblique fissures moving towards each other. | ||
===== Right lower lobe (RLL) collapse ===== | ===== Right lower lobe (RLL) collapse ===== | ||
* | * Triangular opacity can be seen alongside the right heart border. | ||
* | * The right hemidiaphragm may appear elevated because of the obliteration. | ||
* right heart border is clearly seen. | * The right heart border is clearly seen. | ||
* | * Loss of the right hemidiaphragm outline posteriorly and denser lower thoracic vertebrae can be observed on the lateral view. | ||
===== Left upper lobe (LUL) collapse ===== | ===== Left upper lobe (LUL) collapse ===== | ||
* | * It appears as a veil-like opacity because of the absence of minor fissure, stretching out from the hilum and disappearing inferiorly. | ||
* | * The major fissure is seen displaced anteriorly and the lower lobe is hyper-expanded on the lateral view. | ||
* Luftsichel sign (hyper-expanded superior segment of the left lower lobe | * Luftsichel sign is present (hyper-expanded superior segment of the left lower lobe). | ||
===== Left Lower Lobe (LLL) collapse ===== | ===== Left Lower Lobe (LLL) collapse ===== | ||
* | * Increased retrocardiac opacity is seen which shadows the left hemidiaphragm. | ||
* | * Loss of the Left hemidiaphragm outline posteriorly and denser lower thoracic vertebrae can be observed on the lateral view. | ||
The video below demonstrates | |||
The video below demonstrates the lobar classification of atelectasis on a radiograph: | |||
{{#ev:youtube|4oYBLkbDjhg}}<ref>reference</ref> | {{#ev:youtube|4oYBLkbDjhg}}<ref>reference</ref> | ||
| Line 173: | Line 174: | ||
* Hypoxia/[[Hypoxaemia|hypoxemia]] | * Hypoxia/[[Hypoxaemia|hypoxemia]] | ||
== Diagnosis == | |||
[[File:Atelectasia1.jpg|thumb]] | |||
*[[Chest X-Rays|Chest X-ray]]<ref name=":4" /><ref>Khan AN, Al-Jahdali H, AL-Ghanem S, Gouda A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714572/pdf/ATM-04-149.pdf Reading chest radiographs in the critically ill (Part II): Radiography of lung pathologies common in the ICU patient.] Annals of Thoracic Medicine [Internet]. 2009;4(3):149–57. </ref> | *[[Chest X-Rays|Chest X-ray]]<ref name=":4" /><ref>Khan AN, Al-Jahdali H, AL-Ghanem S, Gouda A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714572/pdf/ATM-04-149.pdf Reading chest radiographs in the critically ill (Part II): Radiography of lung pathologies common in the ICU patient.] Annals of Thoracic Medicine [Internet]. 2009;4(3):149–57. </ref> | ||
* Bronchoscopy<ref name=":8">Woodring J. [https://www.ajronline.org/doi/pdfplus/10.2214/ajr.150.4.757 Determining the cause of pulmonary atelectasis: a comparison of plain radiography and CT.] American Journal of Roentgenology. 1988 Apr;150(4):757–63.</ref> | * Bronchoscopy<ref name=":8">Woodring J. [https://www.ajronline.org/doi/pdfplus/10.2214/ajr.150.4.757 Determining the cause of pulmonary atelectasis: a comparison of plain radiography and CT.] American Journal of Roentgenology. 1988 Apr;150(4):757–63.</ref> | ||
* [[CT Scans|CT Scan]]<ref name=":8" /> | *[[CT Scans|CT Scan]]<ref name=":8" /> | ||
* [[Ultrasound Scans|Ultrasound]]<ref>Lichtenstein D, Meziere G. [https://www.researchgate.net/publication/287527270_Ultrasound_diagnosis_of_atelectasis Ultrasound diagnosis of atelectasis] [Internet]. ResearchGate. unknown; 2005 [cited 2021 Nov 20]. </ref><ref>Liu J, Chen S-W, Liu F, Li Q-P, Kong X-Y, Feng Z-C. [https://pubmed.ncbi.nlm.nih.gov/25341049/ The Diagnosis of Neonatal Pulmonary Atelectasis Using Lung Ultrasonography.] Chest [Internet]. 2015 Apr [cited 2021 Nov 20];147(4):1013–9. </ref><ref>Acosta CM, Maidana GA, Jacovitti D, Belaunzarán A, Cereceda S, Rae E, et al. [https://pubs.asahq.org/anesthesiology/article/120/6/1370/11911/Accuracy-of-Transthoracic-Lung-Ultrasound-for Accuracy of Transthoracic Lung Ultrasound for Diagnosing Anesthesia-induced Atelectasis in Children.] Anesthesiology [Internet]. 2014 Jun 1 [cited 2021 Nov 20];120(6):1370–9. </ref> | *[[Ultrasound Scans|Ultrasound]]<ref>Lichtenstein D, Meziere G. [https://www.researchgate.net/publication/287527270_Ultrasound_diagnosis_of_atelectasis Ultrasound diagnosis of atelectasis] [Internet]. ResearchGate. unknown; 2005 [cited 2021 Nov 20]. </ref><ref>Liu J, Chen S-W, Liu F, Li Q-P, Kong X-Y, Feng Z-C. [https://pubmed.ncbi.nlm.nih.gov/25341049/ The Diagnosis of Neonatal Pulmonary Atelectasis Using Lung Ultrasonography.] Chest [Internet]. 2015 Apr [cited 2021 Nov 20];147(4):1013–9. </ref><ref>Acosta CM, Maidana GA, Jacovitti D, Belaunzarán A, Cereceda S, Rae E, et al. [https://pubs.asahq.org/anesthesiology/article/120/6/1370/11911/Accuracy-of-Transthoracic-Lung-Ultrasound-for Accuracy of Transthoracic Lung Ultrasound for Diagnosing Anesthesia-induced Atelectasis in Children.] Anesthesiology [Internet]. 2014 Jun 1 [cited 2021 Nov 20];120(6):1370–9. </ref> | ||
{{#ev:youtube|watch?v=OcIxL56an3c}} | |||
Following video explains the interpretation of the chest x-ray:{{#ev:youtube|watch?v=OcIxL56an3c}}<ref>reference</ref> | |||
== Prevention == | == Prevention == | ||
* It can be prevented by avoiding general anesthesia.<ref name=":4" /> | * It can be prevented by avoiding general anesthesia.<ref name=":4" /> | ||
* The use of [[Non Invasive Ventilation|continuous positive airway pressure (CPAP)]], low tidal volumes, lowest possible FiO2 during induction and maintenance, Positive end-expiratory pressure (PEEP), and lung recruitment maneuvers will help in preventing atelectasis at the point when the use of general anesthesia is unavoidable.<ref name=":4" /> | * The use of [[Non Invasive Ventilation|continuous positive airway pressure (CPAP)]], low tidal volumes, lowest possible FiO2 during induction (to limit absorption atelectasis) and maintenance, Positive end-expiratory pressure (PEEP), and lung recruitment maneuvers will help in preventing atelectasis at the point when the use of general anesthesia is unavoidable.<ref name=":4" /> | ||
* Early mobilization.<ref name=":4" /><ref name=":0">Stiller K, Geake T, Taylor J, Grant R, Hall B. [https://pubmed.ncbi.nlm.nih.gov/2245671/ Acute lobar atelectasis: a comparison of two chest physiotherapy regimens.] Chest. 1990 Dec 1;98(6):1336-40.</ref><ref name=":9">Possa SS, Amador CB, Costa AM, Sakamoto ET, Kondo CS, Vasconcellos AM, et al. I[https://pubmed.ncbi.nlm.nih.gov/24290563/ mplementation of a guideline for physical therapy in the postoperative period of upper abdominal surgery reduces the incidence of atelectasis and length of hospital stay.] Rev Port Neumol 2014;20(2): 69-77.</ref><ref name=":10">Moradian ST, Najafloo M, Mahmoudi H, Ghiasi MS. [https://pubmed.ncbi.nlm.nih.gov/28838589/ Early mobilization reduces the atelectasis and pleural effusion in patients undergoing coronary artery bypass graft surgery: A randomized clinical trial]. J Vasc Nurs 2017;35(3):141–145. </ref> | * Early mobilization.<ref name=":4" /><ref name=":0">Stiller K, Geake T, Taylor J, Grant R, Hall B. [https://pubmed.ncbi.nlm.nih.gov/2245671/ Acute lobar atelectasis: a comparison of two chest physiotherapy regimens.] Chest. 1990 Dec 1;98(6):1336-40.</ref><ref name=":9">Possa SS, Amador CB, Costa AM, Sakamoto ET, Kondo CS, Vasconcellos AM, et al. I[https://pubmed.ncbi.nlm.nih.gov/24290563/ mplementation of a guideline for physical therapy in the postoperative period of upper abdominal surgery reduces the incidence of atelectasis and length of hospital stay.] Rev Port Neumol 2014;20(2): 69-77.</ref><ref name=":10">Moradian ST, Najafloo M, Mahmoudi H, Ghiasi MS. [https://pubmed.ncbi.nlm.nih.gov/28838589/ Early mobilization reduces the atelectasis and pleural effusion in patients undergoing coronary artery bypass graft surgery: A randomized clinical trial]. J Vasc Nurs 2017;35(3):141–145. </ref> | ||
* adequate [[Pain Medications|pain]] control.<ref name=":4" /> | * adequate [[Pain Medications|pain]] control.<ref name=":4" /> | ||
| Line 202: | Line 213: | ||
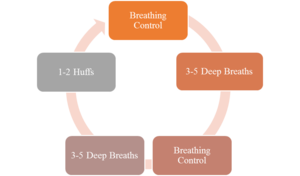
|Airway clearance techniques | |Airway clearance techniques | ||
| | | | ||
* Suctioning of respiratory secretions. | * [[Suctioning|Suctioning of respiratory secretions.]] | ||
* Percussion and vibration therapy. | * [[Respiratory Physiotherapy|Percussion and vibration therapy.]] | ||
* Positive | * [[Positive Expiratory Pressure (PEP) Devices|Positive expiratory pressure.]] | ||
* Active cycle of breathing technique. | * [[Active Cycle of Breathing Technique|Active cycle of breathing technique.]] | ||
* Postural drainage. | * [[Postural Drainage|Postural drainage.]] | ||
* Chest high-frequency oscillations (CHFO) can be delivered via The Metaneb System. | * Chest high-frequency oscillations (CHFO) can be delivered via The Metaneb System. | ||
* Mechanical insufflation and exsufflation. | * [[Assisted Coughing|Mechanical insufflation and exsufflation.]] | ||
* Manual lung hyperinflation. | * [[Manual Hyperinflation|Manual lung hyperinflation.]] | ||
|[[File:The Active Cycle of Breathing Technique.png|thumb]] | |[[File:The Active Cycle of Breathing Technique.png|thumb]] | ||
|- | |- | ||
|Breathing exercises | |Breathing exercises | ||
| | | | ||
* Incentive spirometry | * [[Incentive Spirometry|Incentive spirometry]] | ||
* Sustained maximal inspiration | * Sustained maximal inspiration | ||
* Intermittent positive pressure breathing | * [[Intermittent positive pressure breathing]] | ||
|[[File:Incentive Spirometry using 3 balls.jpg|thumb]] | |[[File:Incentive Spirometry using 3 balls.jpg|thumb]] | ||
|- | |- | ||
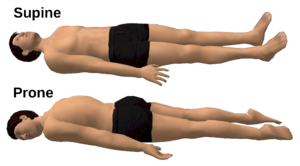
|Positioning | |Positioning | ||
| | | | ||
* Kinetic Therapy | * Kinetic Therapy: It is defined as the continuous turning of a patient slowly along the longitudinal axis to ≥ 40° onto each side, using a specialized bed. | ||
* Turning side to side | * Turning side to side | ||
* Prone positioning | * Prone positioning | ||
| Line 240: | Line 251: | ||
Flexible bronchoscopy can be used for both diagnosing and treating a patient with atelectasis. It is a safe mode of treatment for lung collapse. It can be used under the following circumstances: | Flexible bronchoscopy can be used for both diagnosing and treating a patient with atelectasis. It is a safe mode of treatment for lung collapse. It can be used under the following circumstances: | ||
# | # When the retained secretions with an air bronchogram pattern are present only to the extent of segmental bronchi causing lobar atelectasis. | ||
# when standard chest physiotherapy has been | # when standard chest physiotherapy has been failed to produce a positive outcome. | ||
# | # Life-threatening partial- or complete-lung atelectasis | ||
# | # When vigorous chest therapy is not favorable for the patient or contraindicated for example individuals with chest trauma, unstable vertebral fractures, extensive burns, smoke inhalation, neuromuscular diseases, etc. | ||
# | # when there is a question in diagnosing the patient.<ref>Raoof, Suhail M.D. [https://journals.lww.com/bronchology/Fulltext/2002/01000/Is_Bronchoscopy_Indicated_in_the_Management_of.14.aspx Is Bronchoscopy Indicated in the Management of Atelectasis?], Journal of Bronchology: January 2002 - Volume 9 - Issue 1 - p 52-58 </ref> | ||
Following video shows how bronchoscopy is performed to remove an inhaled foreign body: | |||
{{#ev:youtube|_w7oaWzYHK0}}<ref>reference</ref> | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Atelectasis is | Atelectasis is a pathology that often occurs secondary to an underlying condition or as a postoperative complication and can be significantly morbid or mortal. There is consensus in the literature whether or not it is always preventable but there are different conservative and non-conservative approaches that have shown to be effective in preventing and treating atelectasis.<ref name=":4" /> | ||
== References == | == References == | ||
Latest revision as of 09:17, 30 August 2023
Original Editor - Hing Long Yip
Top Contributors = Areeba Raja, Elena Ferrero Vila, Hing Long Yip, Kim Jackson, Lucinda hampton, Jonathan Wong, Wendy Walker and Sujoy Bose
Introduction[edit | edit source]
Atelectasis is a condition in which there is collapse of lung tissue (parenchyma) with loss of volume. The word "parenchyma" signifies the functional units, the alveoli, of the lungs. Atelectasis describes involvement of relatively smaller units (of alveoli). When larger units of lung parenchyma is involved it is called "collapse" (or collapsed lung), which is essentially just a larger atelectasis. Atelectasis does not involve the airways.
The loss of volume leads to an impaired gaseous exchange between CO2 and O2. It is a reversible condition and usually occurs secondary to an underlying pathology.[1][2]
Epidemiology[edit | edit source]
- Atelectasis does not preferentially affect either sex.
- Incidence doesn't increase in patient with increased age, COPD or asthma.
- The incidence of atelectasis in patients who have recently undergone general anesthesia is as high as 90%[3], with up to 20 - 25% of normal lung noted to be either poorly aerated or atelectatic on CT during anesthesia[4]
- It is commonly observed as a complication in post-operative patients whose breathing mechanism is impacted by the procedure, pain, and prolonged resting.
- Atelectasis is less commonly seen in patients with conditions like COPD, bronchiectasis, and cystic fibrosis.
- Cephalad displacement of the diaphragm in Obese and/or pregnant patients is more likely to cause atelectasis.[2]Atelectasis was found to increase with an increase in BMI for both normal and overweight patients[5].
Classification[edit | edit source]
It can be classified as follows[6]
- pathophysiological mechanism (e.g., compressive atelectasis, absorption atelectasis, surfactant impairment atelectasis)
- the amount of lung involved (e.g., lobar, segmental, or subsegmental atelectasis)
- the location (i.e., specific lobe or segment location).
Pathophysiology[edit | edit source]
Following table comprises the classification of atelectasis based on pathophysiologic mechanism[1][2][6][7][8][9][10][11][12][13][14][15][16][17][18][19][20][21][22]
| Pathophysiologic Mechanism | Pathogenesis | Associated Types of Atelectasis | Cause |
|---|---|---|---|
| Compression of Lung Tissue | When there is an imbalance of net forces across an alveolar wall, it causes the alveoli to collapse. this mechanism of atelectasis causes the lung tissue to compress. |
|
|
| Absorption of Alveolar Air | A second major reason is gas resorption. This may occur in two ways.
|
|
|
| Impairment of Surfactant Function | Deficiency of acquired dysfunction(e . g ., for premature neonates) can result in lacking surfactant capacity. Surfactant reduces alveolar surface tension, stabilising the alveoli and preventing collapse. When inactivated, decreased expansion of the alveoli can occur as a result of increased local surface tension causing a reduction in resting lung volume globally. |
|
|
Patterns of Collapse[edit | edit source]
Atelectasis can be classified on the basis of location according to radiological patterns of collapse[15].
Complete Collapse[edit | edit source]
The white out (complete opacification of a hemithorax) can be seen in complete lung collapse. This appearance can be confused with a large pleural effusion, but the mediastinal shift towards a collapsed lung can distinguish it from pleural effusion where the shift is in the opposite direction of the pathology.
Lobar Collapse[edit | edit source]
Characteristic features associated with individual lobar collapse are as follows:
Right upper lobe (RUL) collapse[edit | edit source]
- Elevation of the right hilum
- Elevation of the minor fissure.
- Minor and major fissures may be visible on the lateral view.
- Golden S sign is present (The minor fissure is usually convex superiorly but may appear concave because of an underlying mass lesion).
Right middle lobe (RML) collapse[edit | edit source]
- Results in minimal opacity and is often overlooked.
- In a posterior -anterior view, the loss of silhouette of the right heart border can be seen.
- A wedge-shaped opacity can be seen on the lateral view as the result of right horizontal and oblique fissures moving towards each other.
Right lower lobe (RLL) collapse[edit | edit source]
- Triangular opacity can be seen alongside the right heart border.
- The right hemidiaphragm may appear elevated because of the obliteration.
- The right heart border is clearly seen.
- Loss of the right hemidiaphragm outline posteriorly and denser lower thoracic vertebrae can be observed on the lateral view.
Left upper lobe (LUL) collapse[edit | edit source]
- It appears as a veil-like opacity because of the absence of minor fissure, stretching out from the hilum and disappearing inferiorly.
- The major fissure is seen displaced anteriorly and the lower lobe is hyper-expanded on the lateral view.
- Luftsichel sign is present (hyper-expanded superior segment of the left lower lobe).
Left Lower Lobe (LLL) collapse[edit | edit source]
- Increased retrocardiac opacity is seen which shadows the left hemidiaphragm.
- Loss of the Left hemidiaphragm outline posteriorly and denser lower thoracic vertebrae can be observed on the lateral view.
The video below demonstrates the lobar classification of atelectasis on a radiograph:
Clinical Implications[edit | edit source]
Following are the clinical implications of atelectasis [18][25]
- Decreased lung compliance
- Hypoxemia
- Increased pulmonary vascular resistance (PVR)
- Inflammation as a local tissue biologic response
- Local immune dysfunction
- Damage of the alveolar-capillary barrier
- Potential loss of lung fluid clearance
- Increased lung protein permeability
- Susceptibility to infection
- Impaired penetration of antibiotics into lung tissue
- Factors that can initiate or exaggerate lung injury
- Acute respiratory failure.
Clinical Presentation[edit | edit source]
The signs and symptoms of atelectasis are often non-specific:[1][26]
- Chest pain
- Shallow breathing pattern
- Reduced chest expansion
- Increased respiratory rate
- Increased work of breathing
- Reduced breath sound on the ipsilateral side of auscultation. In cases of the upper lobe atelectasis, bronchial sounds may be heard, because of the proximity to the major airways.
- Hypoxia/hypoxemia
Diagnosis[edit | edit source]
- Chest X-ray[2][27]
- Bronchoscopy[28]
- CT Scan[28]
- Ultrasound[29][30][31]
Following video explains the interpretation of the chest x-ray:
Prevention[edit | edit source]
- It can be prevented by avoiding general anesthesia.[2]
- The use of continuous positive airway pressure (CPAP), low tidal volumes, lowest possible FiO2 during induction (to limit absorption atelectasis) and maintenance, Positive end-expiratory pressure (PEEP), and lung recruitment maneuvers will help in preventing atelectasis at the point when the use of general anesthesia is unavoidable.[2]
- Early mobilization.[2][33][34][35]
- adequate pain control.[2]
- minimizing parenteral opioid administration.[2]
Management[edit | edit source]
Management of atelectasis depends upon the duration and severity of the condition, from non-invasive intervention ( chest physiotherapy and pharmacological agents) to invasive treatment (bronchoscopy) can be opted according to the individual's state of health.[1]
Physiotherapy Management[edit | edit source]
Different physical therapy interventions have shown to be beneficial in the resolution of atelectasis. Physical therapy treatment can also be used as a preventative or prophylactic measure before surgery. [2]
The table below contains the different physical therapy treatment options in patients with atelectasis.[2][33][34][35][36][37][38][39][40][41][42][43][44][45][46][47][48][49][50][51][52][53]
| Physical Therapy Treatment | ||
|---|---|---|
| Airway clearance techniques |
|
|
| Breathing exercises |
|
|
| Positioning |
|
|
| Early mobilization |
|
|
The Video below demonstrates on the use incentive spirometer:
The Video below demonstrates on different chest physiotherapy treatment options in pediatric population:
Non-conservative Management[edit | edit source]
Flexible bronchoscopy can be used for both diagnosing and treating a patient with atelectasis. It is a safe mode of treatment for lung collapse. It can be used under the following circumstances:
- When the retained secretions with an air bronchogram pattern are present only to the extent of segmental bronchi causing lobar atelectasis.
- when standard chest physiotherapy has been failed to produce a positive outcome.
- Life-threatening partial- or complete-lung atelectasis
- When vigorous chest therapy is not favorable for the patient or contraindicated for example individuals with chest trauma, unstable vertebral fractures, extensive burns, smoke inhalation, neuromuscular diseases, etc.
- when there is a question in diagnosing the patient.[56]
Following video shows how bronchoscopy is performed to remove an inhaled foreign body:
Clinical Bottom Line[edit | edit source]
Atelectasis is a pathology that often occurs secondary to an underlying condition or as a postoperative complication and can be significantly morbid or mortal. There is consensus in the literature whether or not it is always preventable but there are different conservative and non-conservative approaches that have shown to be effective in preventing and treating atelectasis.[2]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Peroni DG, Boner AL. Atelectasis: mechanisms, diagnosis and management. Paediatr Respir Rev. 2000;1:274-8.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Grott K, Dunlap JD. Atelectasis. StatPearls [Internet]. 2020 Aug 10.Available from: https://www.ncbi.nlm.nih.gov/books/NBK545316/#!po=10.0000 (accessed 18.4.2021)
- ↑ Hedenstierna G, Tokics L, Reinius H, Rothen HU, Östberg E, Öhrvik J. Higher age and obesity limit atelectasis formation during anaesthesia: an analysis of computed tomography data in 243 subjects. British journal of anaesthesia. 2020 Mar 1;124(3):336-44.
- ↑ Reber A, Engberg G, Sporre B, Kviele L, Rothen HU, Wegenius G, Nylund U, Hedenstierna G. Volumetric analysis of aeration in the lungs during general anaesthesia. British journal of anaesthesia. 1996 Jun 1;76(6):760-6.
- ↑ Hedenstierna G, Tokics L, Reinius H, Rothen HU, Östberg E, Öhrvik J. Higher age and obesity limit atelectasis formation during anaesthesia: an analysis of computed tomography data in 243 subjects. British journal of anaesthesia : BJA. 2020;124(3):336–44.
- ↑ 6.0 6.1 Stark P. Atelectasis: Types and pathogenesis in adults [Internet]. 2020.
- ↑ Raman TS, Mathew S, Garcha PS. Atelectasis in children. Indian pediatrics. 1998 May;35(5):429-35.
- ↑ Culiner MM. The right middle lobe syndrome, a non-obstructive complex. Diseases of the Chest. 1966; 50(1):57-66.
- ↑ Sutnick AI, Soloff LA. Atelectasis with pneumonia: a pathophysiologic study. Annals of internal medicine. 1964;60:39-46.
- ↑ Magnusson L, Spahn DR. "New concepts of atelectasis during general anaesthesia." BR J Anaesth. 2003;91.1: 61-72.
- ↑ Woodring J H, & Reed JC . Types and mechanisms of pulmonary atelectasis. J Thorac Imag 1996;11:92-108.
- ↑ Nazir A Lone, MD, MBBS, MPH, FACP, FCCP. Pulmonary Atelectasis Clinical Presentation: History, Physical, Causes [Internet]. Medscape.com. Medscape; 2020 [cited 2021 Nov 19].
- ↑ Duggan M, Kavanagh Brian P, Warltier David C. Pulmonary Atelectasis. Anesthesiology [Internet]. 2005 Apr 1 [cited 2021 Nov 19];102(4):838–54.
- ↑ Priftis KN, Rubin B. Atelectasis, Middle Lobe Syndrome and Plastic Bronchitis. Paediatric Bronchoscopy [Internet]. 2010 [cited 2021 Nov 20];149–55.
- ↑ 15.0 15.1 Ray K, Bodenham A, Paramasivam E. Pulmonary atelectasis in anaesthesia and critical care. Continuing Education in Anaesthesia Critical Care & Pain [Internet]. 2014 Oct [cited 2021 Nov 19];14(5):236–45.
- ↑ Domino KB. Pre-emergence Oxygenation and Postoperative Atelectasis. Anesthesiology [Internet]. 2019 Oct 1 [cited 2021 Nov 20];131(4):771–3.
- ↑ Kavanagh BP. Perioperative atelectasis. Minerva anestesiologica [Internet]. 2021 [cited 2021 Nov 19];74(6).
- ↑ 18.0 18.1 Restrepo RD, Braverman J. Current challenges in the recognition, prevention and treatment of perioperative pulmonary atelectasis. Expert Review of Respiratory Medicine [Internet]. 2014 Dec 26 [cited 2021 Nov 19];9(1):97–107.
- ↑ Johnston C, Carvalho WB de. Atelectasias em pediatria: mecanismos, diagnóstico e tratamento. Revista da Associação Médica Brasileira [Internet]. 2008 Oct [cited 2021 Nov 19];54(5).
- ↑ Atağ E. Etiology, diagnosis and treatment in childhood atelectasis. Haydarpasa Numune Training and Research Hospital Medical Journal [Internet]. 2020 [cited 2021 Nov 19]; Available from: https://jag.journalagent.com/hnhjournal/pdfs/HNHJ_61_2_139_144.pdf
- ↑ Navas-Blanco JR, Dudaryk R. Management of Respiratory Distress Syndrome due to COVID-19 infection. BMC Anesthesiology [Internet]. 2020 Jul 20 [cited 2021 Nov 20];20(1).
- ↑ WRIGHT WR. Atelectasis. Canadian Medical Association journal [Internet]. 2021 [cited 2021 Nov 20];62(3).
- ↑ reference
- ↑ reference
- ↑ Zeng C, Lagier D, Lee J-W, Vidal Melo MF. Perioperative Pulmonary Atelectasis: Part I. Biology and Mechanisms. Anesthesiology [Internet]. 2021 Sep 8 [cited 2021 Nov 19];
- ↑ Duggan M, Kavanagh BP. Atelectasis in the perioperative patient. Curr Opin Anaesthesiol. 2007;20:37-42.
- ↑ Khan AN, Al-Jahdali H, AL-Ghanem S, Gouda A. Reading chest radiographs in the critically ill (Part II): Radiography of lung pathologies common in the ICU patient. Annals of Thoracic Medicine [Internet]. 2009;4(3):149–57.
- ↑ 28.0 28.1 Woodring J. Determining the cause of pulmonary atelectasis: a comparison of plain radiography and CT. American Journal of Roentgenology. 1988 Apr;150(4):757–63.
- ↑ Lichtenstein D, Meziere G. Ultrasound diagnosis of atelectasis [Internet]. ResearchGate. unknown; 2005 [cited 2021 Nov 20].
- ↑ Liu J, Chen S-W, Liu F, Li Q-P, Kong X-Y, Feng Z-C. The Diagnosis of Neonatal Pulmonary Atelectasis Using Lung Ultrasonography. Chest [Internet]. 2015 Apr [cited 2021 Nov 20];147(4):1013–9.
- ↑ Acosta CM, Maidana GA, Jacovitti D, Belaunzarán A, Cereceda S, Rae E, et al. Accuracy of Transthoracic Lung Ultrasound for Diagnosing Anesthesia-induced Atelectasis in Children. Anesthesiology [Internet]. 2014 Jun 1 [cited 2021 Nov 20];120(6):1370–9.
- ↑ reference
- ↑ 33.0 33.1 Stiller K, Geake T, Taylor J, Grant R, Hall B. Acute lobar atelectasis: a comparison of two chest physiotherapy regimens. Chest. 1990 Dec 1;98(6):1336-40.
- ↑ 34.0 34.1 Possa SS, Amador CB, Costa AM, Sakamoto ET, Kondo CS, Vasconcellos AM, et al. Implementation of a guideline for physical therapy in the postoperative period of upper abdominal surgery reduces the incidence of atelectasis and length of hospital stay. Rev Port Neumol 2014;20(2): 69-77.
- ↑ 35.0 35.1 Moradian ST, Najafloo M, Mahmoudi H, Ghiasi MS. Early mobilization reduces the atelectasis and pleural effusion in patients undergoing coronary artery bypass graft surgery: A randomized clinical trial. J Vasc Nurs 2017;35(3):141–145.
- ↑ Westerdahl, Elisabeth, et al. “Deep-Breathing Exercises Reduce Atelectasis and Improve Pulmonary Function after Coronary Artery Bypass Surgery.” Chest, vol. 128, no. 5, Nov. 2005, pp. 3482–3488, 10.1378/chest.128.5.3482. Accessed 10 Apr. 2019.
- ↑ Ciesla, Nancy D. “Chest Physical Therapy for Patients in the Intensive Care Unit.” Physical Therapy, vol. 76, no. 6, 1 June 1996, pp. 609–625, pubmed.ncbi.nlm.nih.gov/8650276/, 10.1093/ptj/76.6.609. Accessed 30 Jan. 2022.
- ↑ França EÉ;Ferrari F;Fernandes P;Cavalcanti R;Duarte A;Martinez BP;Aquim EE;Damasceno MC. “Physical Therapy in Critically Ill Adult Patients: Recommendations from the Brazilian Association of Intensive Care Medicine Department of Physical Therapy.” Revista Brasileira de Terapia Intensiva, vol. 24, no. 1, 2012, pubmed.ncbi.nlm.nih.gov/23917708/. Accessed 30 Jan. 2022.
- ↑ Raoof, Suhail, et al. “Effect of Combined Kinetic Therapy and Percussion Therapy on the Resolution of Atelectasis in Critically Ill Patients.” Chest, vol. 115, no. 6, June 1999, pp. 1658–1666, 10.1378/chest.115.6.1658. Accessed 22 Feb. 2021.
- ↑ Siriwat, Rasintra, et al. “Mechanical Insufflation-Exsufflation versus Conventional Chest Physiotherapy in Children with Cerebral Palsy.” Respiratory Care, vol. 63, no. 2, 24 Oct. 2017, pp. 187–193, pubmed.ncbi.nlm.nih.gov/29066586/, 10.4187/respcare.05663. Accessed 28 Jan. 2022.
- ↑ Wu, Meng-Fang, et al. “The Effects of Mechanical Insufflation-Exsufflation on Lung Function and Complications in Cardiac Surgery Patients: A Pilot Study.” Journal of Cardiothoracic Surgery, vol. 16, no. 1, Dec. 2021, cardiothoracicsurgery.biomedcentral.com/articles/10.1186/s13019-021-01738-x, 10.1186/s13019-021-01738-x. Accessed 30 Jan. 2022.
- ↑ Ferreira de Camillis, Márcio Luiz, et al. “Effects of Mechanical Insufflation-Exsufflation on Airway Mucus Clearance among Mechanically Ventilated ICU Subjects.” Respiratory Care, vol. 63, no. 12, 17 July 2018, pp. 1471–1477, rc.rcjournal.com/content/63/12/1471, 10.4187/respcare.06253. Accessed 30 Jan. 2022.
- ↑ Toor, Harjyot, et al. “Efficacy of Incentive Spirometer in Increasing Maximum Inspiratory Volume in an Out-Patient Setting.” Cureus, 4 Oct. 2021, www.cureus.com/articles/64625-efficacy-of-incentive-spirometer-in-increasing-maximum-inspiratory-volume-in-an-out-patient-setting, 10.7759/cureus.18483. Accessed 30 Jan. 2022.
- ↑ Mendes LP, Teixeira LS, da Cruz LJ, Vieira DS, Parreira VF. Sustained maximal inspiration has similar effects compared to incentive spirometers. Respiratory physiology & neurobiology. 2019 Mar 1;261:67-74.
- ↑ Tan AK. Incentive spirometry for tracheostomy and laryngectomy patients. The Journal of otolaryngology. 1995 Oct;24(5):292-4.
- ↑ Denehy, L. “The Use of Manual Hyperinflation in Airway Clearance.” European Respiratory Journal, vol. 14, no. 4, Oct. 1999, p. 958, pubmed.ncbi.nlm.nih.gov/10573249/, 10.1034/j.1399-3003.1999.14d38.x. Accessed 30 Jan. 2022.
- ↑ Paulus, Frederique, et al. “Benefits and Risks of Manual Hyperinflation in Intubated and Mechanically Ventilated Intensive Care Unit Patients: A Systematic Review.” Critical Care, vol. 16, no. 4, 2012, p. R145, ccforum.biomedcentral.com/articles/10.1186/cc11457#:~:text=Manual%20hyperinflation%20(MH)%2C%20a,prevent%20plugging%20of%20the%20airways., 10.1186/cc11457. Accessed 28 Jan. 2022.
- ↑ Schechter MS. “Airway Clearance Applications in Infants and Children.” Respiratory Care, vol. 52, no. 10, 2015, pubmed.ncbi.nlm.nih.gov/17894905/. Accessed 28 Jan. 2022.
- ↑ BALTIERI, Letícia, et al. “Use of Positive Pressure in the Bariatric Surgery and Effects on Pulmonary Function and Prevalence of Atelectasis: Randomized and Blinded Clinical Trial.” ABCD. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo), vol. 27, no. suppl 1, 2014, pp. 26–30, pubmed.ncbi.nlm.nih.gov/25409961/, 10.1590/s0102-6720201400s100007. Accessed 28 Jan. 2022.
- ↑ Bilan, Nemat, and Bita Poorshiri. “The Role of Chest Physiotherapy in Prevention of Postextubation Atelectasis in Pediatric Patients with Neuromuscular Diseases.” Iranian Journal of Child Neurology, vol. 7, no. 1, 2013, pp. 21–4, www.ncbi.nlm.nih.gov/pmc/articles/PMC3943081/. Accessed 28 Jan. 2022.
- ↑ MORRAN, C.G., et al. “RANDOMIZED CONTROLLED TRIAL of PHYSIOTHERAPY for POSTOPERATIVE PULMONARY COMPLICATIONS.” British Journal of Anaesthesia, vol. 55, no. 11, Nov. 1983, pp. 1113–1117, pubmed.ncbi.nlm.nih.gov/6357256/, 10.1093/bja/55.11.1113. Accessed 28 Jan. 2022.
- ↑ Ortiz-Pujols, Shiara, et al. “Chest High-Frequency Oscillatory Treatment for Severe Atelectasis in a Patient with Toxic Epidermal Necrolysis.” Journal of Burn Care & Research, vol. 34, no. 2, 2013, pp. e112–e115, www.ncbi.nlm.nih.gov/pmc/articles/PMC3606286/, 10.1097/bcr.0b013e318257d83e. Accessed 28 Jan. 2022.
- ↑ Schindler MB. Treatment of atelectasis: where is the evidence?. Critical Care. 2005 Aug;9(4):341.
- ↑ reference
- ↑ reference
- ↑ Raoof, Suhail M.D. Is Bronchoscopy Indicated in the Management of Atelectasis?, Journal of Bronchology: January 2002 - Volume 9 - Issue 1 - p 52-58
- ↑ reference