HIV Associated Neurocognitive Disorder (HAND): Difference between revisions
(Added image and content) |
mNo edit summary |
||
| Line 18: | Line 18: | ||
Initially known as AIDS Dementia Complex, HAND is categorized into three levels of functional impairment.<ref name=":3">Clifford DB, Ances BM. H[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4108270/ IV-associated neurocognitive disorder.] The Lancet infectious diseases. 2013 Nov 1;13(11):976-86.</ref> | Initially known as AIDS Dementia Complex, HAND is categorized into three levels of functional impairment.<ref name=":3">Clifford DB, Ances BM. H[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4108270/ IV-associated neurocognitive disorder.] The Lancet infectious diseases. 2013 Nov 1;13(11):976-86.</ref> | ||
# '''Asymptomatic Neurocognitive Impairment (ANI)''' is a mild form of HAND with impaired performance on neuropsychological tests, but affected individuals report independence in performing [[Activities of Daily Living|activities of daily living]] (ADLs) | # '''Asymptomatic Neurocognitive Impairment (ANI)''' is a mild form of HAND with impaired performance on neuropsychological tests, but affected individuals report independence in performing [[Activities of Daily Living|activities of daily living]] (ADLs) - it is still clinically relevant as ANI can progress to more severe forms of HAND | ||
# '''Mild Neurocognitive Disorder (MND)''' is a common form of HAND that mildly interferes with everyday function. | # '''Mild Neurocognitive Disorder (MND)''' is a common form of HAND that mildly interferes with everyday function. | ||
# '''HIV-associated Dementia (HAD)''' refers to HAND in its most severe form, where there is an inability to complete daily tasks independently. Alternative terms used to describe HAD include ''HIV Encephalopathy'' or ''AIDS-dementia complex.'' | # '''HIV-associated Dementia (HAD)''' refers to HAND in its most severe form, where there is an inability to complete daily tasks independently. Alternative terms used to describe HAD include ''HIV Encephalopathy'' or ''AIDS-dementia complex.'' | ||
== Epidemiology == | == Epidemiology == | ||
The exact prevalence of HAND among PLWH is not well known, as the diagnostic criteria and tools are not very sensitive of specific. There is a wide variation in prevalence between and within countries<ref name=":0">Howlett WP. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6794503/ Neurological disorders in HIV in Africa: a review.] African health sciences. 2019 Aug 20;19(2):1953-77.</ref>, but overall studies have shown a reduction in the burden of HAND since the introduction of ART. The mean prevalence of HAND in the post-ART era in Africa is estimated to be 30.4%.<ref name=":0" />With an increase in survival rate, more people with HIV are aging. With age and chronic infection comes an increased risk of vascular dementia, which could co-exist with HAND, thus making it hard to distinguish between [[Vascular Dementia|vascular dementia]] and HAND.<ref name=":2">Cysique LA, Brew BJ. [https://www.researchgate.net/profile/Lucette-Cysique/publication/330328639_Vascular_cognitive_impairment_and_HIV-associated_neurocognitive_disorder_a_new_paradigm/links/5fbf36c6299bf104cf7a5136/Vascular-cognitive-impairment-and-HIV-associated-neurocognitive-disorder-a-new-paradigm.pdf Vascular cognitive impairment and HIV-associated neurocognitive disorder: a new paradigm.] Journal of neurovirology. 2019 Oct;25:710-21.</ref> | The exact prevalence of HAND among PLWH is not well known, as the diagnostic criteria and tools are not very sensitive of specific. There is a wide variation in prevalence between and within countries<ref name=":0">Howlett WP. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6794503/ Neurological disorders in HIV in Africa: a review.] African health sciences. 2019 Aug 20;19(2):1953-77.</ref>, but overall studies have shown a reduction in the burden of HAND since the introduction of ART - i.e. although the prevalence of HAND has not changed, the milder forms account for most cases.<ref name=":5">Saylor D, Dickens AM, Sacktor N, Haughey N, Slusher B, Pletnikov M, Mankowski JL, Brown A, Volsky DJ, McArthur JC. H[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4937456/ IV-associated neurocognitive disorder—pathogenesis and prospects for treatment.] Nature Reviews Neurology. 2016 Apr;12(4):234-48.</ref> The mean prevalence of HAND in the post-ART era in Africa is estimated to be 30.4%.<ref name=":0" /> | ||
With an increase in survival rate, more people with HIV are aging. With age and chronic infection comes an increased risk of vascular dementia, which could co-exist with HAND, thus making it hard to distinguish between [[Vascular Dementia|vascular dementia]] and HAND.<ref name=":2">Cysique LA, Brew BJ. [https://www.researchgate.net/profile/Lucette-Cysique/publication/330328639_Vascular_cognitive_impairment_and_HIV-associated_neurocognitive_disorder_a_new_paradigm/links/5fbf36c6299bf104cf7a5136/Vascular-cognitive-impairment-and-HIV-associated-neurocognitive-disorder-a-new-paradigm.pdf Vascular cognitive impairment and HIV-associated neurocognitive disorder: a new paradigm.] Journal of neurovirology. 2019 Oct;25:710-21.</ref> | |||
== Aetiology == | == Aetiology == | ||
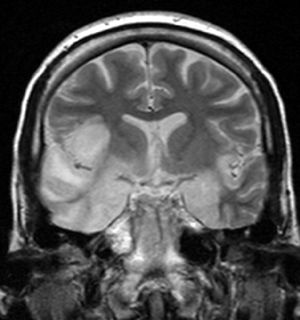
[[File:Encephalitis.jpg|thumb|Encephalitis]] | [[File:Encephalitis.jpg|thumb|Encephalitis]] | ||
HAND is caused by direct effects of the HIV infection, independent of opportunistic infections. HIV crosses the blood-brain barrier and tends to have a regional preferential distribution affecting the [[Basal Ganglia|basal ganglia]] and [[Frontal Lobe|frontal lobe]].<ref name=":1">Modi, G, Mochan A & Modi, M. Neurological Manifestations of HIV. In: Advances in HIV and AIDS Control. Volume (if applicable). Intechopen, 2018.</ref> [[Encephalitis]] | HAND is caused by direct effects of the HIV infection, independent of opportunistic infections. HIV crosses the blood-brain barrier and tends to have a regional preferential distribution affecting the [[Basal Ganglia|basal ganglia]] and [[Frontal Lobe|frontal lobe]].<ref name=":1">Modi, G, Mochan A & Modi, M. Neurological Manifestations of HIV. In: Advances in HIV and AIDS Control. Volume (if applicable). Intechopen, 2018.</ref> The pathophysiology has however changed since the introduction of ART. [[Encephalitis]] and neuronal loss caused by the HIV infection, was considered the main cause of HAND.<ref name=":5" /> It is now evident that sustained inflammation contributes to neurodegeneration. | ||
It is important to note that a poor correlation exists between histopathological changes and clinical severity - this emphasises that factors unrelated to structural damage, determine the clinical picture.<ref name=":1" /> | |||
There is some debate about the extent to which other medical problems that affect PLWH, contribute to HAND.<ref>Chan T, Marta M, Hawkins C, Rackstraw S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7497368/ Cognitive and neurologic rehabilitation strategies for central nervous system HIV infection.] Current HIV/AIDS Reports. 2020 Oct;17:514-21.</ref> Some authors have proposed that additional mechanisms might be at play in the post-ART era<ref name=":2" />. Although brain inflammation is likely still the main mechanism involved in patients who are not virally suppressed, neurovascular mechanisms seem to be at play in those who are virally supressed. It may therefore be necessary to acknowledge two distinct mechanisms that contribute to HAND - one relating to acute brain inflammatory infiltrates, and the other associated with low-grade chronic immune activation and vascular impairment.<ref name=":2" />It is likely that HAND and vascular dementia co-occur in elderly PLWH who present with cognitive impairment.<ref name=":2" /> | There is some debate about the extent to which other medical problems that affect PLWH, contribute to HAND.<ref>Chan T, Marta M, Hawkins C, Rackstraw S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7497368/ Cognitive and neurologic rehabilitation strategies for central nervous system HIV infection.] Current HIV/AIDS Reports. 2020 Oct;17:514-21.</ref> Some authors have proposed that additional mechanisms might be at play in the post-ART era<ref name=":2" />. Although brain inflammation is likely still the main mechanism involved in patients who are not virally suppressed, neurovascular mechanisms seem to be at play in those who are virally supressed. It may therefore be necessary to acknowledge two distinct mechanisms that contribute to HAND - one relating to acute brain inflammatory infiltrates, and the other associated with low-grade chronic immune activation and vascular impairment.<ref name=":2" />It is likely that HAND and vascular dementia co-occur in elderly PLWH who present with cognitive impairment.<ref name=":2" /> | ||
| Line 36: | Line 40: | ||
* High viral load | * High viral load | ||
* [[Anaemia]] | * [[Anaemia]] | ||
* Co-morbidities such as [[Cardiovascular Disease|cardiovascular disease]] (CVD)<ref name=":2" /> | * Co-morbidities such as [[Cardiovascular Disease|cardiovascular disease]] (CVD)<ref name=":2" /><ref name=":5" /> | ||
** PLWH have an increased risk of CVD, despite ART - this is understood to be as a result of chronic inflammation. [[Depression]] is also very prevalent among PLWH and has been shown to increase the risk of CVD | ** PLWH have an increased risk of CVD, despite ART - this is understood to be as a result of chronic inflammation. [[Depression]] is also very prevalent among PLWH and has been shown to increase the risk of CVD | ||
* Lifestyle factors, such as smoking, alcohol and drug use<ref name=":3" /><ref name=":2" /> | * Lifestyle factors, such as smoking, alcohol and drug use<ref name=":3" /><ref name=":2" /> | ||
| Line 149: | Line 153: | ||
==== Other Medication ==== | ==== Other Medication ==== | ||
Other strategies aimed at reducing inflammation - such as methotrexate, statins and antiepileptic medication - do not seem to have significant effects.<ref name=":0" />Symptomatic treatment for depression and psychosis in patients with HAND also forms an important part of the management plan.<ref name=":1" />Patients with HAND have an increased sensitivity to neuroleptic drugs, necessitating increased caution and monitoring when these drugs | Other strategies aimed at reducing inflammation - such as methotrexate, statins and antiepileptic medication - do not seem to have significant effects.<ref name=":0" />Symptomatic treatment for depression and psychosis in patients with HAND also forms an important part of the management plan.<ref name=":1" />Patients with HAND have an increased sensitivity to neuroleptic drugs, necessitating increased caution and monitoring when these drugs. | ||
Research is ongoing to identify medicinal approaches that could prevent neurodegeneration.<ref name=":5" /> | |||
=== Rehabilitation === | === Rehabilitation === | ||
Revision as of 07:38, 6 December 2023
Original Editor - Blessed Denzel Vhudzijena
Top Contributors - Melissa Coetsee, Blessed Denzel Vhudzijena and Kim Jackson
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (23/03/23)
Introduction[edit | edit source]
People living HIV (PLWH) are at risk of developing a range of cognitive, motor, and/or mood problems collectively known as HIV-Associated Neurocognitive Disorder (HAND). Although severe and progressive neurocognitive impairment has become rare in the era of potent antiretroviral therapy (ART), many patients with HIV worldwide still suffer from cognitive impairment. Typical symptoms include difficulties with attention, concentration, and memory; loss of motivation; irritability; depression; and slowed movements.[1]
Among HIV infected patients, HAND remains a feared complication of HIV infection. In addition neurocognitive impairment may affect adherence to treatment and ultimately result in increased morbidity and mortality.
Categories of HAND[edit | edit source]
Initially known as AIDS Dementia Complex, HAND is categorized into three levels of functional impairment.[1]
- Asymptomatic Neurocognitive Impairment (ANI) is a mild form of HAND with impaired performance on neuropsychological tests, but affected individuals report independence in performing activities of daily living (ADLs) - it is still clinically relevant as ANI can progress to more severe forms of HAND
- Mild Neurocognitive Disorder (MND) is a common form of HAND that mildly interferes with everyday function.
- HIV-associated Dementia (HAD) refers to HAND in its most severe form, where there is an inability to complete daily tasks independently. Alternative terms used to describe HAD include HIV Encephalopathy or AIDS-dementia complex.
Epidemiology[edit | edit source]
The exact prevalence of HAND among PLWH is not well known, as the diagnostic criteria and tools are not very sensitive of specific. There is a wide variation in prevalence between and within countries[2], but overall studies have shown a reduction in the burden of HAND since the introduction of ART - i.e. although the prevalence of HAND has not changed, the milder forms account for most cases.[3] The mean prevalence of HAND in the post-ART era in Africa is estimated to be 30.4%.[2]
With an increase in survival rate, more people with HIV are aging. With age and chronic infection comes an increased risk of vascular dementia, which could co-exist with HAND, thus making it hard to distinguish between vascular dementia and HAND.[4]
Aetiology[edit | edit source]
HAND is caused by direct effects of the HIV infection, independent of opportunistic infections. HIV crosses the blood-brain barrier and tends to have a regional preferential distribution affecting the basal ganglia and frontal lobe.[5] The pathophysiology has however changed since the introduction of ART. Encephalitis and neuronal loss caused by the HIV infection, was considered the main cause of HAND.[3] It is now evident that sustained inflammation contributes to neurodegeneration.
It is important to note that a poor correlation exists between histopathological changes and clinical severity - this emphasises that factors unrelated to structural damage, determine the clinical picture.[5]
There is some debate about the extent to which other medical problems that affect PLWH, contribute to HAND.[6] Some authors have proposed that additional mechanisms might be at play in the post-ART era[4]. Although brain inflammation is likely still the main mechanism involved in patients who are not virally suppressed, neurovascular mechanisms seem to be at play in those who are virally supressed. It may therefore be necessary to acknowledge two distinct mechanisms that contribute to HAND - one relating to acute brain inflammatory infiltrates, and the other associated with low-grade chronic immune activation and vascular impairment.[4]It is likely that HAND and vascular dementia co-occur in elderly PLWH who present with cognitive impairment.[4]
Possible risk factors for HAND[2]:
- Advanced age
- Advanced WHO HIV clinical stage
- Low CD4 count
- High viral load
- Anaemia
- Co-morbidities such as cardiovascular disease (CVD)[4][3]
- PLWH have an increased risk of CVD, despite ART - this is understood to be as a result of chronic inflammation. Depression is also very prevalent among PLWH and has been shown to increase the risk of CVD
- Lifestyle factors, such as smoking, alcohol and drug use[1][4]
- Low socio-economic status and education levels[4]
Clinical Presentation[edit | edit source]
The manifestations of HAND include cognitive, behavioural and motor dysfunction which are indicative of frontal lobe and basal ganglia involvement.[5]When clear focal neurological signs are present (eg. hemiplegia, apraxia, aphasia) other pathologies should be considered. The table below summarises the clinical signs associated with HAND:[5]
| Cognitive decline | Behavioural abnormalities | Motor dysfunction | |
|---|---|---|---|
| Domains affected and clinical effects | Affects verbal and visual memory, complex sequencing and mental flexibility
|
|
|
| Implications | Patients forget appointments and medication adherence may decline. Maintaining conversations become harder. Increasing difficulty in performing more complex ADL's independently. | Social withdrawal and psychiatric presentations that can affect relationships | Deteriorating handwriting and increased clumsiness. Increasing dependence for basic ADLs |
The dominant domains affected seem to be influenced by whether HAND developed prior to or after initiating ART:
- Pre-ART HAND: psychomotor slowing - inattention, slow thinking, forgetfulness, unsteady gait, tremor, social withdrawal[2]
- Post-ART HAND: more cortical involvement - impaired learning ability, memory executive function and extrapyramidal motor features[2]
In advanced HAND, patients develop mutism and incontinence, followed by a vegetative state.[5]
Diagnosis[edit | edit source]
HAND is a clinical diagnosis based on exclusion. It is however possible for HAND to be present along with other neurological conditions. Diagnosis is based on the following criteria[5]:
- Positive HIV test
- History of progressive changes in cognition and behaviour
- Impairment in at least two domains of neuropsychological performance
- Absence of:
- Focal neurological signs
- Intoxication withdrawal
- Metabolic derangement
- CNS opportunistic infection
- CNS neoplastic lesion
Differential Diagnosis[edit | edit source]
See the page on Neurological Complications Associated with HIV. In PLWH who have had prior brain damage due to HIV (eg. opportunistic infections), with stable viral load, need to be differentiated from patients who present with virally mediated neurological signs.[1][7]
- CNS Lymphoma
- Progressive multifocal leukoencephalopathy (PML)
- Opportunistic infections, including toxoplasmosis and cryptococcal meningitis.
- Vitamin B-12 and folate deficiency
- Vascular dementia
- Depression
Investigations[edit | edit source]
Cerebrospinal fluid (CSF) investigations and neuroimaging (MRI and CT-brain) are useful to exclude other potential causes of cognitive changes in PLWH.[5]Encephalopathies caused by substance abuse or head injury need to be excluded. Blood tests can also be useful to investigate hepatic or renal failure as a possible cause of metabolic encephalopathy.[5]
| Blood tests | CSF | Neuroimaging |
|---|---|---|
| Full blood count
Urea & Creatinine Liver function Vit B12 level Syphilis serology CD4 count and viral load |
Usually abnormal in patients with HAND - lymphocytic pleocytosis with mildly elevated protein. These findings are however not specific to HAND. CSF analysis helps to exclude opportunistic infections. | Cerebral atrophy with ventricular enlargement may be present in HAND. |
Outcome Measures[edit | edit source]
Neuropsychometric tests that measure psychomotor speed, verbal and non-verbal learning and sustained attention, can be used as a screening and monitoring tool. Normal values for African regions are however lacking, which questions the validity of many existing tests. In order to detect more mild deficits, more difficult tests are often indicated.[5]Although a comprehensive assessment is not always possible in busy clinical settings, brief memory tests should be performed in order to improve the likelihood of ART adherence.
- Montreal Cognitive Assessment: Measures attention, concentration, memory, executive functioning and reasoning. Although not optimal for detecting HAND, this test may be useful for monitoring neurocognitive function.[7]
- International HIV Dementia Scale (IHDS): Measures motor speed, psychomotor speed and learning, registration and memory; a score of <10 is regarded to be indicative of HAND, but poor sensitivity and specificity means that this test can not be used in isolation.[2]It may be useful in detecting HAD, but not ANI and MND.
- Mini-Mental (MMSE): Not sufficiently sensitive for HAND - areas of working memory and attention are not accounted for[7]
- Functional Assessment Measure: Measures psychosocial and cognitive function (not HIV specific)
Management[edit | edit source]
Management is multi-dimensional and should include both prevention and treatment strategies.
Prevention Strategies[edit | edit source]
- Early detection and management of cardiovascular risk factors - this includes screening, optimal management of high blood pressure and diabetes, as well as lifestyle modifications and interventions (smoking cessation and physical activity).[4]
- Screening for early signs of cognitive impairment and initiating cognitive training early.[4]
Medical Treatment[edit | edit source]
The most important strategy is to start ART as early as possible (which also implies early detection of HIV infection). ART can prevent HAND, slow the progression and even lead to some improvements in neurocognitive function.
ART[edit | edit source]
Early initiation of ART helps to prevent HAND in PLWH. In patients who already present with HAND, some improvement may occur once ART is initiated, but these improvements usually plateau after 9-months on ART.[2] Many patients affected by HAND will experience persistence of symptoms. Combined ART regimes with better central nervous system penetration can help to prevent HAND.
Other Medication[edit | edit source]
Other strategies aimed at reducing inflammation - such as methotrexate, statins and antiepileptic medication - do not seem to have significant effects.[2]Symptomatic treatment for depression and psychosis in patients with HAND also forms an important part of the management plan.[5]Patients with HAND have an increased sensitivity to neuroleptic drugs, necessitating increased caution and monitoring when these drugs.
Research is ongoing to identify medicinal approaches that could prevent neurodegeneration.[3]
Rehabilitation[edit | edit source]
The rehabilitation team can include a physiotherapist (PT), occupational therapist (OT), speech therapist (ST) and psychologist (Psych). All rehabilitation professionals working with PLWH can be involved in screening for cognitive impairment to ensure early detection and intervention. The table below summarises the scope of interventions for HAND, as well as the rehabilitation team members usually responsible for each aspect:
| Intervention: | Details | Team members |
|---|---|---|
| Addressing CVD risk factors such as smoking, physical activity and depression | ||
| Neurocognitive Interventions | ||
| Interventions to improve behavioural symptoms and independence in ADLs | ||
| Caregivers' educational and emotional support | ||
| Physical rehabilitation to improve balance and ambulation |
Conclusion[edit | edit source]
ART has resulted in significant improvements in the outcomes of PLWH, but full protection of the nervous system is yet to be achieved. The deficits caused by HAND now require more in depth assessments, as changes are more subtle. It is likely that multiple mechanisms contribute to neurocognitive impairments in PLWH, and therefore a multi-disciplinary approach is important to ensure optimal independence and quality of life for PLWH.[1]
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Clifford DB, Ances BM. HIV-associated neurocognitive disorder. The Lancet infectious diseases. 2013 Nov 1;13(11):976-86.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Howlett WP. Neurological disorders in HIV in Africa: a review. African health sciences. 2019 Aug 20;19(2):1953-77.
- ↑ 3.0 3.1 3.2 3.3 Saylor D, Dickens AM, Sacktor N, Haughey N, Slusher B, Pletnikov M, Mankowski JL, Brown A, Volsky DJ, McArthur JC. HIV-associated neurocognitive disorder—pathogenesis and prospects for treatment. Nature Reviews Neurology. 2016 Apr;12(4):234-48.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Cysique LA, Brew BJ. Vascular cognitive impairment and HIV-associated neurocognitive disorder: a new paradigm. Journal of neurovirology. 2019 Oct;25:710-21.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 Modi, G, Mochan A & Modi, M. Neurological Manifestations of HIV. In: Advances in HIV and AIDS Control. Volume (if applicable). Intechopen, 2018.
- ↑ Chan T, Marta M, Hawkins C, Rackstraw S. Cognitive and neurologic rehabilitation strategies for central nervous system HIV infection. Current HIV/AIDS Reports. 2020 Oct;17:514-21.
- ↑ 7.0 7.1 7.2 Valcour VG. Evaluating cognitive impairment in the clinical setting: practical screening and assessment tools. Topics in antiviral medicine. 2011 Dec;19(5):175.