Ankle-Brachial Index: Difference between revisions
Chloe Waller (talk | contribs) No edit summary |
Chloe Waller (talk | contribs) (Update video, results and interpretation) |
||
| Line 50: | Line 50: | ||
* Supported, comfortable supine position. | * Supported, comfortable supine position. | ||
=== Technique<ref>Stanford Medicine. Introduction to Measuring the Ankle Brachial Index. Availble from: https://stanfordmedicine25.stanford.edu/the25/ankle-brachial-index.html#:~:text=The%20ABI%20is%20performed%20by,or%2010%2DmHz%20Doppler%20instrument. (Last accessed 13/09/2022)</ref> === | === Technique<ref name=":6">Stanford Medicine. Introduction to Measuring the Ankle Brachial Index. Availble from: https://stanfordmedicine25.stanford.edu/the25/ankle-brachial-index.html#:~:text=The%20ABI%20is%20performed%20by,or%2010%2DmHz%20Doppler%20instrument. (Last accessed 13/09/2022)</ref> === | ||
# Place the cuff around the patient's arm, use the doppler and press against the skin at the level of the brachial artery in the arm. Inflate the cuff to about 20 mmHg above the last audible pulse. The Doppler signal should disappear. Then slowly deflate the cuff, approximately 1 mmHg/sec. When the Doppler signal re-appears, the pressure of the cuff is equal to the brachial systolic pressure. Record the brachial systolic pressure. | # Place the cuff around the patient's arm, use the doppler and press against the skin at the level of the brachial artery in the arm. Inflate the cuff to about 20 mmHg above the last audible pulse. The Doppler signal should disappear. Then slowly deflate the cuff, approximately 1 mmHg/sec. When the Doppler signal re-appears, the pressure of the cuff is equal to the brachial systolic pressure. Record the brachial systolic pressure. | ||
| Line 65: | Line 65: | ||
{{#ev:youtube|0_0VlLSTAAE}}<ref>St Michael's Hospital. How to perform an ankle brachial index. Available from https://www.youtube.com/watch?v=0_0VlLSTAAE (Last accessed 13/09/2022)</ref> | {{#ev:youtube|0_0VlLSTAAE}}<ref>St Michael's Hospital. How to perform an ankle brachial index. Available from https://www.youtube.com/watch?v=0_0VlLSTAAE (Last accessed 13/09/2022)</ref> | ||
== | == Results and Interpretation<ref name=":6" /> == | ||
{| class="wikitable" | |||
|+ | |||
!ABI value | |||
!Interpretation | |||
!Recommendation | |||
|- | |||
|<0.5 | |||
|Severe arterial disease | |||
|Refer to vascular specialist | |||
|- | |||
|0.5-0.8 | |||
|Moderate arterial disease | |||
|Refer to vascular specialist | |||
|- | |||
|0.8-0.9 | |||
|Mild arterial disease | |||
|Treat risk factors | |||
|- | |||
|0.9-1 | |||
|Acceptable | |||
|None | |||
|- | |||
|1-1.4 | |||
|Normal range | |||
|None | |||
|- | |||
|>1.4 | |||
|Calcification of vessels | |||
|Refer to vascular specialist | |||
|} | |||
== General Considerations == | == General Considerations == | ||
| Line 79: | Line 102: | ||
* There is more decrease in ankle pressure after walking in case of moderate occlusive PAD specifically in the proximal vessels. | * There is more decrease in ankle pressure after walking in case of moderate occlusive PAD specifically in the proximal vessels. | ||
* The ABI has a high sensitivity, but these results came from one single study which may be included participants with critical limb ischemia<ref name=":1" /> or diabetic patients. | * The ABI has a high sensitivity, but these results came from one single study which may be included participants with critical limb ischemia<ref name=":1">Crawford F, Welch K, Andras A, Chappell FM. [https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010680.pub2/full Ankle brachial index for the diagnosis of lower limb peripheral arterial disease]. Cochrane Database of Systematic Reviews. 2016(9).</ref> or diabetic patients. | ||
* People with a history of PAD will demonstrate a continuous decrease of ABI over time, about 0.06 over 4.6 years. On the other side, there is a smaller decrease in the general population it's about 0.025 over 5 years<ref name=":0" />. | * People with a history of PAD will demonstrate a continuous decrease of ABI over time, about 0.06 over 4.6 years. On the other side, there is a smaller decrease in the general population it's about 0.025 over 5 years<ref name=":0" />. | ||
* If the [[Ankle and Foot|ankle]] pressure is less than 50 mm Hg it is associated with a higher risk of avascularity and [[Amputations|amputation]]. | * If the [[Ankle and Foot|ankle]] pressure is less than 50 mm Hg it is associated with a higher risk of avascularity and [[Amputations|amputation]]. | ||
* Results of included studies suggest the inter- and intra-tester reliability of the ABI is acceptable. However, inconsistencies in obtaining systolic pressure measurements, calculating ABI values, and incomplete reporting of methodologies and statistical analysis make it difficult to determine the validity of the results of included studies.<ref>Casey S, Lanting S, Oldmeadow C, Chuter V. [https://pubmed.ncbi.nlm.nih.gov/31388357/ The reliability of the ankle brachial index: a systematic review.] J Foot Ankle Res. 2019 Aug 2;12:39. </ref> | |||
== Resources == | == Resources == | ||
Revision as of 10:31, 13 September 2022
Original Editor - Khloud Shreif
Top Contributors - Khloud Shreif, Chloe Waller, Vidya Acharya and Lucinda hampton
Introduction[edit | edit source]
The ankle-brachial index (ABI) is a quick, non-invasive technique used to check vascular status and for peripheral arterial disease (PAD)[1][2]. It was first described by Winsor in 1950[3].
The ABI is the ratio between the systolic blood pressure of the lower limb (specifically at the ankle) and the upper limb, to assess for narrowing or blockages in the arteries in the legs[1][4].
Indications[edit | edit source]
Symptoms of peripheral artery disease:
- Intermittent claudication or cramping pain in the legs.[5]
- Wounds on the legs that are slow to heal.[6]
- Leg that feels colder than other parts of the body or is a different shade of color. [6]
Those with risk factors for PAD, such as:[4]
- History of tobacco use
- Restricted blood flow (atherosclerosis) in other parts of your body.
- History of stroke or transient ischemic attack.
- Family history of heart disease.
- Over 70 years of age. [5]
Contraindications[edit | edit source]
- Patients with confirmed or suspected DVT, because of the possibility of breaking of the thrombus.
- Severe leg pain.[5]
Procedures[edit | edit source]
Tools[5][edit | edit source]
- Doppler
- Blood pressure monitor.
- Pressure cuffs
Preparation[edit | edit source]
- Rest for 10-20 minutes prior to the test.
- Wear loose, comfortable clothing.
- Avoid nicotine/ smoking for 2 hours prior to the test.
- Supported, comfortable supine position.
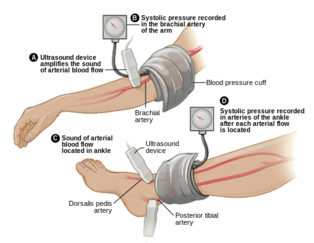
Technique[7][edit | edit source]
- Place the cuff around the patient's arm, use the doppler and press against the skin at the level of the brachial artery in the arm. Inflate the cuff to about 20 mmHg above the last audible pulse. The Doppler signal should disappear. Then slowly deflate the cuff, approximately 1 mmHg/sec. When the Doppler signal re-appears, the pressure of the cuff is equal to the brachial systolic pressure. Record the brachial systolic pressure.
- Place the cuff around the lower leg and locate two arteries:
- Dorsalis pedis, which is a branch from the anterior tibial artery, it is located between the tibialis anterior and extensor hallucis longus
- Posterior tibial artery, that is behind the medial malleolus.
- Repeat the same technique as the arm to record the dorsalis pedis and posterior tibial arterty: using the doppler to locate the signal, inflating the cuff and then deflating until the signal re-appears.
- The ABI value is calculated by taking the higher pressure of the 2 arteries at the ankle, divided by the brachial arterial systolic pressure.
- Repeat the ankle measurement for the other leg in order to calculate its ABI.
Demonstration video:
Results and Interpretation[7][edit | edit source]
| ABI value | Interpretation | Recommendation |
|---|---|---|
| <0.5 | Severe arterial disease | Refer to vascular specialist |
| 0.5-0.8 | Moderate arterial disease | Refer to vascular specialist |
| 0.8-0.9 | Mild arterial disease | Treat risk factors |
| 0.9-1 | Acceptable | None |
| 1-1.4 | Normal range | None |
| >1.4 | Calcification of vessels | Refer to vascular specialist |
General Considerations[edit | edit source]
- In normal healthy people, there is a slight decrease in ABI if measured immediately after lower limb exercises due to the decreased ankle systolic pressure because of vasodilation during lower limb exercises, and return to normal within about 3 min after rest.
- There is more decrease in ankle pressure after walking in case of moderate occlusive PAD specifically in the proximal vessels.
- The ABI has a high sensitivity, but these results came from one single study which may be included participants with critical limb ischemia[9] or diabetic patients.
- People with a history of PAD will demonstrate a continuous decrease of ABI over time, about 0.06 over 4.6 years. On the other side, there is a smaller decrease in the general population it's about 0.025 over 5 years[2].
- If the ankle pressure is less than 50 mm Hg it is associated with a higher risk of avascularity and amputation.
- Results of included studies suggest the inter- and intra-tester reliability of the ABI is acceptable. However, inconsistencies in obtaining systolic pressure measurements, calculating ABI values, and incomplete reporting of methodologies and statistical analysis make it difficult to determine the validity of the results of included studies.[10]
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 McClary KN, Massey P. Ankle Brachial Index. 2022 Jan 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–
- ↑ 2.0 2.1 Aboyans V, Criqui MH, Abraham P, Allison MA, Creager MA, Diehm C, Fowkes FG, Hiatt WR, Jönsson B, Lacroix P, Marin B. Measurement and interpretation of the ankle-brachial index: a scientific statement from the American Heart Association. Circulation. 2012 Dec 11;126(24):2890-909.
- ↑ Winsor, T. Influence of arterial disease on the systolic blood pressure gradients of the extremity. Am J Med Sci. 1950 Aug;220(2):117-26.
- ↑ 4.0 4.1 Mayo Clinic.Ankle Brachial Index. Available from:https://www.mayoclinic.org/tests-procedures/ankle-brachial-index/about/pac-20392934 (Last accessed 12/09/2022)
- ↑ 5.0 5.1 5.2 5.3 Ankle Brachial Index: Quick Reference Guide for Clinicians. Journal of Wound, Ostomy and Continence Nursing: March/April 2012 - Volume 39 - Issue 2S - p S21-S29
- ↑ 6.0 6.1 Harvard Health Publishing. Ankle-brachial index. Available from: https://www.health.harvard.edu/newsletter_article/ankle-brachial-index (Last accessed 12/09/2022).
- ↑ 7.0 7.1 Stanford Medicine. Introduction to Measuring the Ankle Brachial Index. Availble from: https://stanfordmedicine25.stanford.edu/the25/ankle-brachial-index.html#:~:text=The%20ABI%20is%20performed%20by,or%2010%2DmHz%20Doppler%20instrument. (Last accessed 13/09/2022)
- ↑ St Michael's Hospital. How to perform an ankle brachial index. Available from https://www.youtube.com/watch?v=0_0VlLSTAAE (Last accessed 13/09/2022)
- ↑ Crawford F, Welch K, Andras A, Chappell FM. Ankle brachial index for the diagnosis of lower limb peripheral arterial disease. Cochrane Database of Systematic Reviews. 2016(9).
- ↑ Casey S, Lanting S, Oldmeadow C, Chuter V. The reliability of the ankle brachial index: a systematic review. J Foot Ankle Res. 2019 Aug 2;12:39.