Noonan Syndrome: Difference between revisions
No edit summary |
Rucha Gadgil (talk | contribs) No edit summary |
||
| (92 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editor '''- [[User:Kirenga Bamurange Liliane|Kirenga Bamurange Liliane]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
== Definition == | == Definition == | ||
Noonan Syndrome (NS) is | [[File:12 years Old female with Noonan Syndrome.PNG|thumb|NS Typical webbed neck, structural curve with rib deformity.|384x384px|alt=]]Noonan syndrome (NS) is a rare autosomal dominant condition or a [[Genetic Conditions and Inheritance|genetic]] mutation present from birth, that causes a distinctive appearance and a range of health problems<ref name=":0">Noonan Syndrome: Practice Essentials. Available from:https://emedicine.medscape.com/article/947504-overview#a4 ( accessed 14 September, 2020)</ref>. The most consistent features are wide-set eyes, low-set ears, short stature, and pulmonic stenosis. <ref>Allen MJ, Sharma S. [https://www.ncbi.nlm.nih.gov/books/NBK532269/ Noonan Syndrome.] InStatPearls [Internet] 2021 Jul 25. StatPearls Publishing.Available: https://www.ncbi.nlm.nih.gov/books/NBK532269/<nowiki/>(accessed 4.3.2022)</ref>People with Noonan syndrome may be mildly affected, or more severely affected. Noonan syndrome develops in a baby before birth. Sometimes, the disorder is diagnosed straight away, but some children with mild symptoms aren't diagnosed until they get older.<ref name=":2">Health Direct [https://www.healthdirect.gov.au/noonan-syndrome Noonan Syndrome] Available: https://www.healthdirect.gov.au/noonan-syndrome<nowiki/>(accessed 4.3.2022)</ref> | ||
Noonan and Ehmke were the first to describe a succession of patients with same similarities including unusual faces and multiple malformations like congenital heart disease. | Noonan and Ehmke were the first to describe a succession of patients with the same similarities including unusual faces and multiple malformations like congenital heart disease. These patients were previously thought to have a form of [[Turner Syndrome]], which has a lot of similarities in its clinical features with Noonan Syndrome.<ref name=":0" /> | ||
== Epidemiology == | |||
The estimated incidence is at ~1 in 1000-2500. As individuals have normal number of chromosomes, both males and females can be affected.<ref>Radiopedia Noonan Syndrome Available: https://radiopaedia.org/articles/noonan-syndrome<nowiki/>(accessed 4.3.2022)</ref> | |||
The | == Pathological Process == | ||
[[File:Autosomal Dominant Gene Structure.png|thumb|345x345px|Autosomal Dominant Gene Structure ]]The inheritance is autosomal dominant although a significant proportion of cases are sporadic. Many genes have been implicated, the most common being the PTPN11 gene which encodes for SHP2, which results in an inability to inactivate SHP2 causing increased signalling of the Ras/MAPK pathway. | |||
There are 2 types of mutations that cause Noonan Syndrome: | |||
* | * '''Inherited:''' Children who have one parent with NS who carries the defective gene (autosomal dominant) have a 50% chance of developing the disorder. | ||
* '''Random:''' NS can develop because of a new mutation in children who don't have a genetic predisposition for the disorder (de novo).<ref name=":3">Noonan Syndrome. Available from:https://www.mayoclinic.org/diseases-conditions/noonan-syndrome/symptoms-causes/syc-20354422 ( accessed 15 September, 2020)</ref> | |||
== Clinical Presentation == | |||
[[File:3 months old infant with Noonan Syndrome.jpg|thumb|NS at 3 months: Eyebrow slant, left-side eyelid dropping|440x440px|alt=]]NS is most often characterized by facial and musculoskeletal features. Although these features are more present during early childhood, they change over time and appear less characteristic during adulthood: | |||
* In the newborn infant, the head is large with a small face, a tall forehead, wide-spaced eyes, short nose, low set ears, and a broad or webbed neck | |||
[[File:Noonan Syndrome Infant.jpg|thumb|434x434px|Low set posteriorly rotated, abnormally formed ear: 3 month with NS|alt=]] | |||
''' | |||
== | |||
Many infants with NS also have heart (cardiac) defects such as: | |||
* [[Cardiac Valve Defects|Pulmonary valvular stenosis]] | |||
* Hypertrophic [[Cardiomyopathies|cardiomyopathy]] | |||
* Septal defects | |||
NS | The following characteristics are also seen among individuals with NS: | ||
* Short stature: up to 83% of people with NS have a short stature | * Short stature: up to 83% of people with NS have a short stature | ||
* Pectus deformity of the chest with | * Pectus deformity of the chest with [[Pectus carinatum ( pigeon chest )|pectus carinatum]] (hollow chest) | ||
* Kyphosis | * [[Kyphosis]] | ||
* Scoliosis | * [[Scoliosis]] | ||
* Cubitus valgus (outward deviation of the elbows) | * Cubitus valgus (outward deviation of the elbows) | ||
* Rounded shoulders | * Rounded shoulders | ||
* Rib abnormalities | * [[Ribs|Rib]] abnormalities | ||
* Genu valgum ( Knock knees) | * Genu valgum ( Knock knees) | ||
* Joint hyperextensibility (see [[Beighton score|Beighton]] score) | |||
* Talipes equinovarus ([[Clubfoot, Management and Barriers to treatment in underdeveloped countries.|club foot]])<ref>Van der Burgt I. Noonan syndrome. Orphanet journal of rare diseases. 2007 Dec;2(1):1-6.</ref> | |||
* | |||
Individuals with NS may also present less common problems including: | Individuals with NS may also present less common problems including: | ||
* | * Learning disability: children with NS tend to often have a mild learning disability due to a lower IQ average | ||
* Feeding problems: children with NS may have problems with sucking and chewing | * [[Feeding the Child with Cerebral Palsy|Feeding problems]]: children with NS may have problems with sucking and chewing | ||
* Speech problems: articulation difficulty due to a high arched palate and weak muscles | * Speech problems: articulation difficulty due to a high arched palate and weak muscles | ||
* | * [[Behavioral problems in children|Behavioral problems]]: some children with NS may have attention problems or difficulty to describe their or people emotions | ||
* Eyes condition such as squint, lazy eye | * Eyes condition such as squint, lazy eye | ||
* Hearing loss | * Hearing loss | ||
* Hypotonia: decreased muscle tone will make children with NS reach early milestones later compared to other children | * Hypotonia: decreased muscle tone will make children with NS reach early milestones later compared to other children | ||
* Undescended testicles: one | * Undescended testicles: one or both testicles may fail to drop into the scrotum in boys with NS | ||
* | * Infertility can be diagnosed in boys if undescended testicles are not corrected at an early age | ||
* Lymphoedema | * [[Lymphoedema]] | ||
* Bone marrow problems | * [[Bone Marrow|Bone marrow]] problems- [[Leukemia]] | ||
* Skin problems such as dystrophic nails; extra prominence on pads of fingers and toes; follicular keratosis; hyperelastic skin; moles; thick curly hair or thin sparse hair | * [[Skin]] problems such as dystrophic nails; extra prominence on pads of fingers and toes; follicular keratosis; hyperelastic skin; moles; thick curly hair or thin sparse hair.<ref name=":1">Bhambhani V, Muenke M. Noonan syndrome. Am Fam Physician. 2014; 89(1):37-43.</ref> | ||
== Diagnosis == | |||
Diagnosis is usually based on the child’s appearance and health problems, and is confirmed with genetic testing. This will involve a blood test. Further tests may be needed and include: heart investigations including an [[electrocardiogram]] (ECG) and echocardiogram (ultrasound).<ref name=":2" /> | |||
== | == Differential Diagnosis == | ||
Several conditions identified as RASopathies have similarities with NS. These conditions all have similar signs and symptoms and are caused by changes in the same cell signaling pathway. | |||
Besides NS, the RASopathies consist of cardiofaciocutaneous syndrome, Costello syndrome, Neurofibromatosis type 1, Legius syndrome, and Noonan syndrome with multiple lentigines.<ref>Noonan Syndrome - Genetics Home Reference. U.S National Library of Medicine. Available from: https://ghr.nlm.nih.gov/condition/noonan-syndrome#sourcesforpage (accessed 19 September, 2020) | |||
</ref> The differential diagnosis, therefore, includes [[William's Syndrome|Williams syndrome]], intrauterine exposure to primidone, fetal alcohol syndrome, and Aarskog syndrome. Other cardiocutaneous syndromes such as LEOPARD syndrome, Neurofibromatosis, and Watson syndrome have a markedly overlapping phenotype.<ref>Allanson, JE. Noonan Syndrome. Journal of Medical Genetics,1987, 4: 9-13</ref> | |||
== | == Management == | ||
Living with Noonan syndrome: Most children with Noonan syndrome go on to lead normal lives in adulthood. However, a child newly diagnosed with the disorder may need a number of treatments, and regular tests to monitor their condition over time. The types of treatment and support required will depend on the problems they experience<ref name=":2" />. A regular comprehensive follow-up in a multidisciplinary approach is needed to manage the medical and developmental complications of Noonan syndrome.<ref name=":3" /> | |||
=== Medical Management === | |||
The medical treatment will focus on problems such as: | |||
* '''Heart Defects:''' | |||
** With pulmonary stenosis: no treatment will be required if it's mild. If it's severe a surgery to narrow the valves will be required | |||
** Hypertrophic cardiomyopathy may need to be treated with either medication such as beta-blockers or surgery to remove or destroy some of the excess heart muscle | |||
** Septal defects usually get better with age and thus do not need any treatment.<ref name=":4">Noonan syndrome - Treatment [Internet]. nhs.uk. 2020 [cited 25 September 2020]. Available from: <nowiki>https://www.nhs.uk/conditions/noonan-syndrome/treatment/</nowiki> | |||
</ref> | |||
* '''Growth issues:''' A growth hormone therapy is given around 4 to 5 years old. The medication Somatropin, a single daily injection is the most used. By adulthood, some people with NS may have normal height, but short stature is more common. | |||
*'''Feeding and speech problems:''' Speech Therapy is needed to effectively use the muscles of the mouth and develop them. | |||
*'''Undescended testicles''': A surgical procedure called orchidopexy is performed | |||
*'''Learning Disabilities:''' Special educational needs and the assessment procedure.<ref name=":4" /> | |||
*'''Gross and fine motor delays''' to be assessed and treated by Occupational Therapists and Physiotherapy | |||
People of any age with Noonan syndrome may be at an increased risk of cancer. They need to adopt healthy habits throughout life. It is imperative that they regularly do have physical checkups and screenings.<ref name=":5">Noonan Syndrome. Available from https://www.stjude.org/disease/noonan-syndrome.html ( accessed 22 September, 2020)</ref> | |||
== | === Physiotherapy Management === | ||
In addition to medical management, patients may need to be referred for physiotherapy. The physiotherapy treatment will focus on patient education, improvement of the range of motion; strengthening exercises as well as pain management. | |||
Early Intervention is crucial for a child diagnosed with Noonan Syndrome as they have [[Child Development|delayed motor milestones]]. The following exercises improve and maintain flexibility, endurance, strength, coordination, and balance in children with NS:<ref>4. [Internet]. Bigleapsct.com. 2020 [cited 25 September 2020]. Available from: <nowiki>https://www.bigleapsct.com/single-post/2016/05/16/Noonan-Syndrome</nowiki> </ref> | |||
# '''Sit-ups:''' From lying down on their back the child comes up to a full sitting position by holding the therapist's fingers | |||
# '''Tall kneel:''' This is a great exercise for balance and core strength | |||
# '''Sitting balance''' as a great activity for core balance, strength, and body awareness. | |||
# '''Sit to stand from step stool:''' This is a great leg strengthening activity as the child stands up from the sitting position. | |||
# '''Stepping over obstacles:''' it's an important activity as balance is challenging for children with NS | |||
# '''Crawling over pillows''' as a great overall strengthening and motor planning activity. | |||
# '''Stair negotiation skills:''' As children with NS have a hard time alternating their feet on the stairs because of poor balance and short stature; this is a very good practice for them. | |||
# '''Therapy ball:''' The child lies on their back over the ball and reaches back for something, and comes up to a sitting position | |||
# '''Passive bicycle kicks''' while singing | |||
# '''Standing or walking on different surfaces''' such as hardwood floor, pillows, balance disc, shoes on grass, shoes on wood chips at the playground. | |||
# '''Lying on the back''' to massage the bottom of their feet for proprioceptive input; which helps with independent walking and balance on the stairs. | |||
# '''Joint Compressions''' help in body awareness with independent standing/walking and balance on various surfaces. | |||
In their study on perceived motor problems in daily life, Croonen et.al (2016); showed that people with NS reported particular problems related to pain; decreased muscle strength, fatigue, and clumsiness and their evident impact on functioning in their daily activities. Most people with NS believed that exercise, appropriate physiotherapy advice, and other supportive intervention are key elements to improved motor performance.<ref>Croonen EA, Harmsen M, Van der Burgt I, Draaisma JM, Noordam K, Essink M, Nijhuis‐van der Sanden MW. Perceived motor problems in daily life: Focus group interviews with people with Noonan syndrome and their relatives. American Journal of Medical Genetics Part A. 2016 Sep;170(9):2349-56. | |||
</ref> | |||
== | == Prevention == | ||
There is no known way to prevent Noonan Syndrome because it occurs spontaneously, However, it is recommended that people with a history of NS get genetic counseling before they have children.<ref>Noonan Syndrome. Available from: http://pennstatehershey.adam.com/content.aspx?productid=112&pid=1&gid=001656 (Accessed 4 October 2020)</ref> If Noonan syndrome is detected early, it's possible that ongoing and comprehensive care may lessen some of its complications such as heart disease.<ref name=":3" /> | |||
== Prognosis == | |||
Noonan Syndrome is a lifelong condition. People with NS are differently affected and therefore their life expectancy will depend on the presence and severity of congenital heart defects Noonan Syndrome.<ref>Noonan Syndrome. Available from:https://rarediseases.info.nih.gov/diseases/10955/noonan-syndrome ( Accessed 28 September, 2020)</ref> | |||
<div class="col-md-6"> {{#ev:youtube|28ID5WP2lAw|250}} <div class="text-right"><ref>Noonan Foundation. Overview of the genetics of Noonan syndrome. Available from: http://www.youtube.com/watch?v=28ID5WP2lAw&t=327s [last accessed 3/10/2020]</ref></div></div> | |||
<div class="col-md-6"> {{#ev:youtube|Ctp6Msz3Kgc|250}} <div class="text-right"><ref>The Traveling Awareness Bears. Noonan Syyndrome Awarenenss. Available from: http://www.youtube.com/watch?v=Ctp6Msz3Kgc [last accessed 3/10/2020]</ref></div></div> | |||
== References | == References == | ||
<references /> | <references /> | ||
[[Category:Paediatrics]] | |||
[[Category:Paediatrics - Conditions]] | |||
[[ Category: Conditions]] | |||
[[Category: Genetic Disorders]] | |||
Latest revision as of 22:30, 10 May 2024
Definition[edit | edit source]
Noonan syndrome (NS) is a rare autosomal dominant condition or a genetic mutation present from birth, that causes a distinctive appearance and a range of health problems[1]. The most consistent features are wide-set eyes, low-set ears, short stature, and pulmonic stenosis. [2]People with Noonan syndrome may be mildly affected, or more severely affected. Noonan syndrome develops in a baby before birth. Sometimes, the disorder is diagnosed straight away, but some children with mild symptoms aren't diagnosed until they get older.[3]
Noonan and Ehmke were the first to describe a succession of patients with the same similarities including unusual faces and multiple malformations like congenital heart disease. These patients were previously thought to have a form of Turner Syndrome, which has a lot of similarities in its clinical features with Noonan Syndrome.[1]
Epidemiology[edit | edit source]
The estimated incidence is at ~1 in 1000-2500. As individuals have normal number of chromosomes, both males and females can be affected.[4]
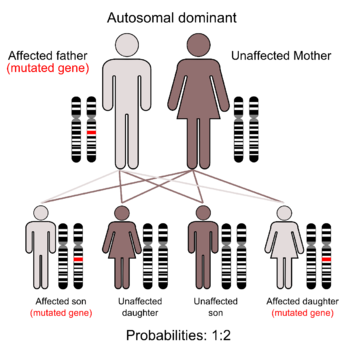
Pathological Process[edit | edit source]
The inheritance is autosomal dominant although a significant proportion of cases are sporadic. Many genes have been implicated, the most common being the PTPN11 gene which encodes for SHP2, which results in an inability to inactivate SHP2 causing increased signalling of the Ras/MAPK pathway.
There are 2 types of mutations that cause Noonan Syndrome:
- Inherited: Children who have one parent with NS who carries the defective gene (autosomal dominant) have a 50% chance of developing the disorder.
- Random: NS can develop because of a new mutation in children who don't have a genetic predisposition for the disorder (de novo).[5]
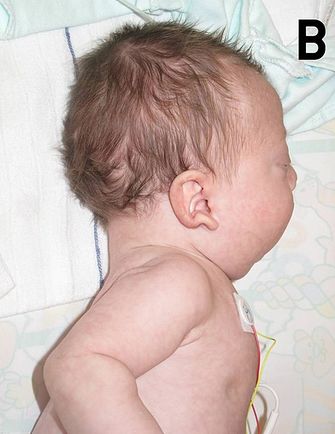
Clinical Presentation[edit | edit source]
NS is most often characterized by facial and musculoskeletal features. Although these features are more present during early childhood, they change over time and appear less characteristic during adulthood:
- In the newborn infant, the head is large with a small face, a tall forehead, wide-spaced eyes, short nose, low set ears, and a broad or webbed neck
Many infants with NS also have heart (cardiac) defects such as:
- Pulmonary valvular stenosis
- Hypertrophic cardiomyopathy
- Septal defects
The following characteristics are also seen among individuals with NS:
- Short stature: up to 83% of people with NS have a short stature
- Pectus deformity of the chest with pectus carinatum (hollow chest)
- Kyphosis
- Scoliosis
- Cubitus valgus (outward deviation of the elbows)
- Rounded shoulders
- Rib abnormalities
- Genu valgum ( Knock knees)
- Joint hyperextensibility (see Beighton score)
- Talipes equinovarus (club foot)[6]
Individuals with NS may also present less common problems including:
- Learning disability: children with NS tend to often have a mild learning disability due to a lower IQ average
- Feeding problems: children with NS may have problems with sucking and chewing
- Speech problems: articulation difficulty due to a high arched palate and weak muscles
- Behavioral problems: some children with NS may have attention problems or difficulty to describe their or people emotions
- Eyes condition such as squint, lazy eye
- Hearing loss
- Hypotonia: decreased muscle tone will make children with NS reach early milestones later compared to other children
- Undescended testicles: one or both testicles may fail to drop into the scrotum in boys with NS
- Infertility can be diagnosed in boys if undescended testicles are not corrected at an early age
- Lymphoedema
- Bone marrow problems- Leukemia
- Skin problems such as dystrophic nails; extra prominence on pads of fingers and toes; follicular keratosis; hyperelastic skin; moles; thick curly hair or thin sparse hair.[7]
Diagnosis[edit | edit source]
Diagnosis is usually based on the child’s appearance and health problems, and is confirmed with genetic testing. This will involve a blood test. Further tests may be needed and include: heart investigations including an electrocardiogram (ECG) and echocardiogram (ultrasound).[3]
Differential Diagnosis[edit | edit source]
Several conditions identified as RASopathies have similarities with NS. These conditions all have similar signs and symptoms and are caused by changes in the same cell signaling pathway.
Besides NS, the RASopathies consist of cardiofaciocutaneous syndrome, Costello syndrome, Neurofibromatosis type 1, Legius syndrome, and Noonan syndrome with multiple lentigines.[8] The differential diagnosis, therefore, includes Williams syndrome, intrauterine exposure to primidone, fetal alcohol syndrome, and Aarskog syndrome. Other cardiocutaneous syndromes such as LEOPARD syndrome, Neurofibromatosis, and Watson syndrome have a markedly overlapping phenotype.[9]
Management[edit | edit source]
Living with Noonan syndrome: Most children with Noonan syndrome go on to lead normal lives in adulthood. However, a child newly diagnosed with the disorder may need a number of treatments, and regular tests to monitor their condition over time. The types of treatment and support required will depend on the problems they experience[3]. A regular comprehensive follow-up in a multidisciplinary approach is needed to manage the medical and developmental complications of Noonan syndrome.[5]
Medical Management[edit | edit source]
The medical treatment will focus on problems such as:
- Heart Defects:
- With pulmonary stenosis: no treatment will be required if it's mild. If it's severe a surgery to narrow the valves will be required
- Hypertrophic cardiomyopathy may need to be treated with either medication such as beta-blockers or surgery to remove or destroy some of the excess heart muscle
- Septal defects usually get better with age and thus do not need any treatment.[10]
- Growth issues: A growth hormone therapy is given around 4 to 5 years old. The medication Somatropin, a single daily injection is the most used. By adulthood, some people with NS may have normal height, but short stature is more common.
- Feeding and speech problems: Speech Therapy is needed to effectively use the muscles of the mouth and develop them.
- Undescended testicles: A surgical procedure called orchidopexy is performed
- Learning Disabilities: Special educational needs and the assessment procedure.[10]
- Gross and fine motor delays to be assessed and treated by Occupational Therapists and Physiotherapy
People of any age with Noonan syndrome may be at an increased risk of cancer. They need to adopt healthy habits throughout life. It is imperative that they regularly do have physical checkups and screenings.[11]
Physiotherapy Management[edit | edit source]
In addition to medical management, patients may need to be referred for physiotherapy. The physiotherapy treatment will focus on patient education, improvement of the range of motion; strengthening exercises as well as pain management.
Early Intervention is crucial for a child diagnosed with Noonan Syndrome as they have delayed motor milestones. The following exercises improve and maintain flexibility, endurance, strength, coordination, and balance in children with NS:[12]
- Sit-ups: From lying down on their back the child comes up to a full sitting position by holding the therapist's fingers
- Tall kneel: This is a great exercise for balance and core strength
- Sitting balance as a great activity for core balance, strength, and body awareness.
- Sit to stand from step stool: This is a great leg strengthening activity as the child stands up from the sitting position.
- Stepping over obstacles: it's an important activity as balance is challenging for children with NS
- Crawling over pillows as a great overall strengthening and motor planning activity.
- Stair negotiation skills: As children with NS have a hard time alternating their feet on the stairs because of poor balance and short stature; this is a very good practice for them.
- Therapy ball: The child lies on their back over the ball and reaches back for something, and comes up to a sitting position
- Passive bicycle kicks while singing
- Standing or walking on different surfaces such as hardwood floor, pillows, balance disc, shoes on grass, shoes on wood chips at the playground.
- Lying on the back to massage the bottom of their feet for proprioceptive input; which helps with independent walking and balance on the stairs.
- Joint Compressions help in body awareness with independent standing/walking and balance on various surfaces.
In their study on perceived motor problems in daily life, Croonen et.al (2016); showed that people with NS reported particular problems related to pain; decreased muscle strength, fatigue, and clumsiness and their evident impact on functioning in their daily activities. Most people with NS believed that exercise, appropriate physiotherapy advice, and other supportive intervention are key elements to improved motor performance.[13]
Prevention[edit | edit source]
There is no known way to prevent Noonan Syndrome because it occurs spontaneously, However, it is recommended that people with a history of NS get genetic counseling before they have children.[14] If Noonan syndrome is detected early, it's possible that ongoing and comprehensive care may lessen some of its complications such as heart disease.[5]
Prognosis[edit | edit source]
Noonan Syndrome is a lifelong condition. People with NS are differently affected and therefore their life expectancy will depend on the presence and severity of congenital heart defects Noonan Syndrome.[15]
References[edit | edit source]
- ↑ 1.0 1.1 Noonan Syndrome: Practice Essentials. Available from:https://emedicine.medscape.com/article/947504-overview#a4 ( accessed 14 September, 2020)
- ↑ Allen MJ, Sharma S. Noonan Syndrome. InStatPearls [Internet] 2021 Jul 25. StatPearls Publishing.Available: https://www.ncbi.nlm.nih.gov/books/NBK532269/(accessed 4.3.2022)
- ↑ 3.0 3.1 3.2 Health Direct Noonan Syndrome Available: https://www.healthdirect.gov.au/noonan-syndrome(accessed 4.3.2022)
- ↑ Radiopedia Noonan Syndrome Available: https://radiopaedia.org/articles/noonan-syndrome(accessed 4.3.2022)
- ↑ 5.0 5.1 5.2 Noonan Syndrome. Available from:https://www.mayoclinic.org/diseases-conditions/noonan-syndrome/symptoms-causes/syc-20354422 ( accessed 15 September, 2020)
- ↑ Van der Burgt I. Noonan syndrome. Orphanet journal of rare diseases. 2007 Dec;2(1):1-6.
- ↑ Bhambhani V, Muenke M. Noonan syndrome. Am Fam Physician. 2014; 89(1):37-43.
- ↑ Noonan Syndrome - Genetics Home Reference. U.S National Library of Medicine. Available from: https://ghr.nlm.nih.gov/condition/noonan-syndrome#sourcesforpage (accessed 19 September, 2020)
- ↑ Allanson, JE. Noonan Syndrome. Journal of Medical Genetics,1987, 4: 9-13
- ↑ 10.0 10.1 Noonan syndrome - Treatment [Internet]. nhs.uk. 2020 [cited 25 September 2020]. Available from: https://www.nhs.uk/conditions/noonan-syndrome/treatment/
- ↑ Noonan Syndrome. Available from https://www.stjude.org/disease/noonan-syndrome.html ( accessed 22 September, 2020)
- ↑ 4. [Internet]. Bigleapsct.com. 2020 [cited 25 September 2020]. Available from: https://www.bigleapsct.com/single-post/2016/05/16/Noonan-Syndrome
- ↑ Croonen EA, Harmsen M, Van der Burgt I, Draaisma JM, Noordam K, Essink M, Nijhuis‐van der Sanden MW. Perceived motor problems in daily life: Focus group interviews with people with Noonan syndrome and their relatives. American Journal of Medical Genetics Part A. 2016 Sep;170(9):2349-56.
- ↑ Noonan Syndrome. Available from: http://pennstatehershey.adam.com/content.aspx?productid=112&pid=1&gid=001656 (Accessed 4 October 2020)
- ↑ Noonan Syndrome. Available from:https://rarediseases.info.nih.gov/diseases/10955/noonan-syndrome ( Accessed 28 September, 2020)
- ↑ Noonan Foundation. Overview of the genetics of Noonan syndrome. Available from: http://www.youtube.com/watch?v=28ID5WP2lAw&t=327s [last accessed 3/10/2020]
- ↑ The Traveling Awareness Bears. Noonan Syyndrome Awarenenss. Available from: http://www.youtube.com/watch?v=Ctp6Msz3Kgc [last accessed 3/10/2020]