Renal Cancer: Difference between revisions
No edit summary |
No edit summary |
||
| (95 intermediate revisions by 11 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''-Jason Larimore & Olivia Tefera [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | '''Original Editors '''-Jason Larimore & Olivia Tefera [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</ | </div> | ||
== Introduction == | |||
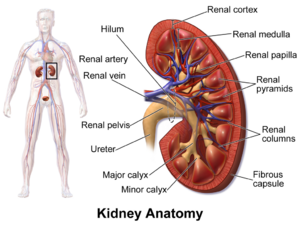
[[File:KidneyAnatomy 01.png|thumb]] | |||
Kidney cancer is particularly important because it creates a big economic burden, especially when it spread (metastatic kidney cancer). Kidney cancer primarily arises from the renal parenchyma, with clear cell renal cell carcinoma being the most common type, derived from the renal tubular epithelium, and comprising roughly 70% of cases in adults. The majority of epidemiological research tends to concentrate on kidney cancer as a whole entity, leading to a scarcity of detailed information about the various histological subtypes. Less common are tumors originating from the renal pelvis a form in the center of the kidney where urine collects, and [[Wilms Tumor|Wilms tumors]] in children that typically develops before the age of five, which are significantly rarer than renal cell carcinomas and display different epidemiologic patterns<ref>Scelo G, Larose TL. Epidemiology and risk factors for kidney cancer. Journal of Clinical Oncology. 2018 Dec 12;36(36):3574.</ref>. | |||
Over the past 28 years, there has been minimal progress in lessening the impact of kidney cancer. It's essential to intensify efforts aimed at minimizing exposure to risk factors and enhancing the prevention and early detection of this illness<ref name=":1">Safiri S, Kolahi AA, Mansournia MA, Almasi-Hashiani A, Ashrafi-Asgarabad A, Sullman MJ, Bettampadi D, Qorbani M, Moradi-Lakeh M, Ardalan M, Mokdad A. [https://www.nature.com/articles/s41598-020-70840-2#Abs1 The burden of kidney cancer and its attributable risk factors in 195 countries and territories, 1990–2017.] Scientific Reports. 2020 Aug 17;10(1):13862.</ref>. | |||
== Epidemiology == | |||
Worldwide, cancer cases rose from 18.3 million in 2007 to 24.5 million in 2017. Annually, renal cancers are responsible for over 131,000 fatalities and 342,000 new cases globally each year. Renal cell carcinomas are considered the 8th most prevalent cancer in adults, it comprise about 2% of total cancer diagnoses and constitutes 80-90% of primary malignant tumors in adult kidneys<ref name=":1" />. Patients are typically 50-70 years of age at presentation 1,2, with a moderate male predilection of 2:1 2.<ref name=":0">Radiopedia [https://radiopaedia.org/articles/renal-cell-carcinoma-1 Renal cell carcinoma] Available from:https://radiopaedia.org/articles/renal-cell-carcinoma-1 (last accessed 1.9.2020)</ref>. | |||
The most common renal neoplasm in adults is renal cell carcinoma. RCC accounts for close to 90% of all renal neoplasms and approximately 3% of all cancers. | |||
== Risk Factors == | |||
Several risk factors for kidney cancer have been identified, with some being alterable, thus presenting a chance for primary prevention. These risk factors are grouped as follows: | |||
# Lifestyle-Related Risk Factors: This includes [[Smoking Cessation and Brief Intervention|smoking]], [[obesity]], [[Alcoholism|alcohol]] use, lack of physical activity, and dietary choices. | |||
# Medical History: Factors such as [[Blood Pressure|high blood pressure]], chronic kidney conditions, kidney stones, cystic disease related to dialysis, cyclophosphamide treatment (a type of chemotherapy), post-kidney transplant, and [[diabetes]]. | |||
# Environmental and Occupational Exposures: Exposure to substances like trichloroethylene and aristolochic acid (chemical compounds known for their health risks, especially in relation to cancer). | |||
# Genetic risk factors and others.<ref name=":1" /> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Presentation is classically described as the triad of: | |||
# Macroscopic haematuria: 60% | |||
# Flank pain: 40% | |||
# Palpable flank mass: 30-40%<ref name=":0" /> | |||
This triad presents in patients with renal cell carcinoma, however this triad only found in 10-15% of patients the remaining cases present with signs and symptoms related to the site of distant metastases<ref name=":2">Maestroni U, Gasparro D, Ziglioli F, Guarino G, Campobasso D. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8577602/ Metastatic clear cell renal cell carcinoma: the great pretender and the great dilemma.] World Journal of Oncology. 2021 Oct;12(5):178.</ref>. That is why there are some cases were discovered by chance with examination<ref name=":2" />. | |||
About 25-30% of patients have metastatic disease at the time of diagnosis. Renal cancer most often spreads to the lungs (75%), regional lymph nodes (65%), bones (40%), and liver (40%).<span style="mso-spacerun: yes"><ref name="p2">Goodman CC, Fuller KS. Pathology: Implications for the physical therapist. 3rd ed. St. Louis, Missouri: Saunders Elsevier, 2009.</ref></span> The patient may complain of a cough or bone pain secondary to metastasis to the lungs or bone, respectively. | |||
{{#ev:youtube|Cq6PAVbquus|300}}<ref>Dana-Farber Cancer Institute . Signs and Symptoms of a Kidney Tumor | Dana-Farber Cancer Institute. Available from: http://www.youtube.com/watch?v=Cq6PAVbquus[last accessed 27/11/2023</ref> | |||
== Pathology == | |||
Renal cell carcinoma (RCC), or renal cancer, is categorized into four major types, determined by cellular origin: | |||
*Clear cell: 70-80%, arises from proximal convoluted tubules | |||
*Papillary: 13-20%, arises from distal convoluted tubules | |||
*Chromophobe: 5%, arises from intercalated cells of collecting ducts<ref>Muglia VF, Prando A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4492569/ Renal cell carcinoma: histological classification and correlation with imaging findings.] Radiologia brasileira. 2015 May;48:166-74.</ref> | |||
*Collecting duct: 1% of cases<ref name="p2" />. | |||
[[File:Renal cell carcinoma.jpg|thumb|235x235px|Renal cell carcinoma]] | |||
== Grading == | |||
Histological nuclear grading: | |||
The most widely used and most predictive grading system for renal cell cancer specially renal cell carcinoma is the "Fuhrman nuclear grade". The Fuhrman nuclear grade is a system used to classify the aggressiveness of kidney cancer, particularly renal cell carcinoma, based on the microscopic appearance of the cancer cells. It helps in determining the prognosis and potential treatment strategies for the disease with grade I and grade II, have a better prognosis and grade III and grade IV, suggest a poor prognosis as the following: | |||
* Grade 1: Small, round, uniform nuclei, about 10 micrometers or smaller. Nucleoli absent or not clear at 400x magnification. | |||
* Grade 2: Nuclei slightly larger than Grade 1, up to 15 micrometers, mostly uniform with some shape irregularities. Nucleoli may be seen but not distinct at 400x magnification. | |||
* Grade 3: Larger, more irregular nuclei, over 15 micrometers. Nucleoli are clearly visible at 400x magnification. | |||
* Grade 4: Very large, irregularly shaped nuclei. Nucleoli are clearly visible, and cells may have multiple nuclei. | |||
== Diagnostic Tests == | |||
[[File:Recurrent renal cell carcinoma.png|thumb|Recurrent renal cell carcinoma.]] | |||
The following tests and procedures may be used: | |||
* Physical exam and health history | |||
* Ultrasound exam | |||
* [[Blood Tests|Blood tests]]: An unusual (higher or lower than normal) amount of a substance can be a sign of disease. | |||
* Urinalysis | |||
* [[CT Scans|CT]] scan (CAT scan): A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. | |||
* [[MRI Scans|MRI]] (magnetic resonance imaging) - This procedure is also called nuclear magnetic resonance imaging (NMRI). | |||
* Biopsy - a thin needle is inserted into the tumor and a sample of tissue is withdrawn<ref>Low G, Huang G, Fu W, Moloo Z, Girgis S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4882405/ Review of renal cell carcinoma and its common subtypes in radiology]. World journal of radiology. 2016 May 5;8(5):484.</ref>. | |||
== Treatment Overview == | |||
Patients with renal cell cancer may work with a team of health care professionals to coordinate their care.eg Urologist, Surgeon, Urologic Oncologists, Medical Oncologists, Radiation Oncologists, Oncology Nurse, Registered Dietician<ref name="I">National Cancer Institute. What you need to know about kidney cancer: Treatment. http://www.cancer.gov/cancertopics/wyntk/kidney/page8 (accessed 30 Jan 2013).</ref> | |||
There are different types of treatment for patients with renal cell cancer. Five types of standard treatment are used: | |||
# Surgery | |||
# [[Radiation Side Effects and Syndromes|Radiation]] therapy | |||
# [[Chemotherapy Side Effects and Syndromes|Chemotherapy]] | |||
# Immunotherapy | |||
# Targeted therapy | |||
RCC is primarily treated by surgical interventions. Although aggressive, a radical nephrectomy is the preferred method of treatment for both localized and metastasized diseased. This consists of the removal of: | |||
*Kidney | |||
*Gerota’s fascia: fibroareolar tissue surrounding the kidney and perirenal fat | |||
*Adrenal gland | |||
*Regional lymph nodes | |||
Kidney cancer, when diagnosed at a stage where it has already spread to other organs, is often not curable. The current standard treatment for such advanced stages of kidney cancer involves the use of targeted agents. <ref name=":3">Unverzagt S, Moldenhauer I, Nothacker M, Rossmeissl D, Hadjinicolaou AV, Peinemann F, Greco F, Seliger B. [https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011673.pub2/full Immunotherapy for metastatic renal cell carcinoma.] Cochrane Database of Systematic Reviews. 2017(5).</ref>. | |||
* Targeted therapies, which work by targeting the cancer at a cellular level, have expanded the options for the treatment of kidney cancer. Targeted treatments block specific abnormal signals present in kidney cancer cells that allow them to grow. These medications have shown promise in treating kidney cancer that has spread to other areas of the body. The targeted medications Axitinib (Inlyta), Bevacizumab (Avastin), Pazopanib (Votrient), Sorafenib (Nexavar) and Sunitinib (Sutent) block signals that play a role in the growth of blood vessels that provide nutrients to cancer cells and allow cancer cells to spread. Temsirolimus (Torisel) and Everolimus (Afinitor) are targeted medications that block a signal that allows cancer cells to grow and survive. Targeted therapy medications can cause serious side effects, such as: a severe rash, diarrhea, and fatigue | |||
* Whereas targeted therapies specifically block the renal cancer cells from growing and spreading, immunotherapy works in a more general way by using the body's immune system to fight the cancer. Immunotherapy medications include Interferon and Aldesleukin (Proleukin), which are synthetic versions of chemicals made in your body. Side effects of these medications include: chills, fever, nausea, vomiting and loss of appetite<ref name=":3" />. | |||
== Physical Therapy Management == | |||
[[File:Gym equipment.png|right|frameless|456x456px]] | |||
Maintaining physical strength is important while undergoing renal cancer treatment and a physical therapist will be able to provide an exercise plan specifically designed for a patient’s needs. | |||
* If a patient had surgery to remove the tumor, modest exercise can help regain muscle tone and help to rebuild the muscles that were cut, increase that patient’s range of motion, and help to prevent complications that can occur post-surgery such as: respiratory infection, pressure sores, and the formation of a deep vein thrombosis (DVT). | |||
* Exercise can have the additional benefit of reducing stress and depression, which can be common occurrences in patients undergoing cancer treatment. | |||
* Physical therapy can also be used to combat fatigue, which is not only a common symptom of renal cancer but it can be a side effect of treatment (e.g. chemotherapy). Building up [[Endurance Exercise|endurance]] can reduce the incidence and severity of fatigue. This will be an important factor in increasing a patient’s independence and ability to maintain a high [[Quality of Life|quality of life]]. | |||
* Educate the patient regarding his or her diet, which will play an important role throughout the treatment process. | |||
* <u></u>A systematic review and meta-analysis of randomized clinical trials suggested that intradialytic exercise protocols had positive outcomes in chronic kidney disease patients with poor cardiopulmonary function and reduced exercise tolerance and ventilatory efficiency<ref>Andrade FP, Rezende PS, Ferreira TS, Borba GC, Müller AM, Rovedder PME. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6895108/ Effects of intradialytic exercise on cardiopulmonary capacity in chronic kidney disease: systematic review and meta-analysis of randomized clinical trials.] Scientific Reports. 2019 Dec 5;9(1):18470.</ref>. | |||
== Case Reports/ Case Studies == | |||
* [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3215540/ Sciatica leading to the discovery of a renal cell carcinoma] | |||
* [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3177931/ Atypical presentations and rare metastatic sites of renal cell carcinoma: a review of case reports] | |||
* [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3297757/ Hereditary leiomyomatosis and renal cell cancer presenting as metastatic kidney cancer at 18 years of age: implications for surveillance] | |||
* [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3254138/ Renal cancer and Wegener's granulomatosis: a case report] | |||
== Resources == | |||
[https://www.cancer.gov/types/kidney/patient/kidney-treatment-pdq#Keypoint3 National Cancer Institute]. | |||
[https://jnccn.org/view/journals/jnccn/13/2/article-p151.xml NCCN Guidelines] | |||
[[Oncology]] | |||
[[Oncology Rehabilitiation|Oncology rehabilitation]] | |||
[[Oncology and Palliative Care|Oncology and palliative care]] | |||
[https://www.kidneycancer.org/?s=exercise%20with%20kidney%20cancer Kidney Cancer Association] | |||
== References == | == References == | ||
<references /><nowiki>{{</nowiki> | |||
<references />{{ | |||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
[[Category:Medical]] | |||
[[Category:Oncology]] | |||
Latest revision as of 13:50, 27 November 2023
Original Editors -Jason Larimore & Olivia Tefera from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Olivia Tefera, Jason Larimore, Lucinda hampton, Admin, Khloud Shreif, Elaine Lonnemann, Kim Jackson, WikiSysop, Vidya Acharya, Wendy Walker and 127.0.0.1
Introduction[edit | edit source]
Kidney cancer is particularly important because it creates a big economic burden, especially when it spread (metastatic kidney cancer). Kidney cancer primarily arises from the renal parenchyma, with clear cell renal cell carcinoma being the most common type, derived from the renal tubular epithelium, and comprising roughly 70% of cases in adults. The majority of epidemiological research tends to concentrate on kidney cancer as a whole entity, leading to a scarcity of detailed information about the various histological subtypes. Less common are tumors originating from the renal pelvis a form in the center of the kidney where urine collects, and Wilms tumors in children that typically develops before the age of five, which are significantly rarer than renal cell carcinomas and display different epidemiologic patterns[1].
Over the past 28 years, there has been minimal progress in lessening the impact of kidney cancer. It's essential to intensify efforts aimed at minimizing exposure to risk factors and enhancing the prevention and early detection of this illness[2].
Epidemiology[edit | edit source]
Worldwide, cancer cases rose from 18.3 million in 2007 to 24.5 million in 2017. Annually, renal cancers are responsible for over 131,000 fatalities and 342,000 new cases globally each year. Renal cell carcinomas are considered the 8th most prevalent cancer in adults, it comprise about 2% of total cancer diagnoses and constitutes 80-90% of primary malignant tumors in adult kidneys[2]. Patients are typically 50-70 years of age at presentation 1,2, with a moderate male predilection of 2:1 2.[3].
The most common renal neoplasm in adults is renal cell carcinoma. RCC accounts for close to 90% of all renal neoplasms and approximately 3% of all cancers.
Risk Factors[edit | edit source]
Several risk factors for kidney cancer have been identified, with some being alterable, thus presenting a chance for primary prevention. These risk factors are grouped as follows:
- Lifestyle-Related Risk Factors: This includes smoking, obesity, alcohol use, lack of physical activity, and dietary choices.
- Medical History: Factors such as high blood pressure, chronic kidney conditions, kidney stones, cystic disease related to dialysis, cyclophosphamide treatment (a type of chemotherapy), post-kidney transplant, and diabetes.
- Environmental and Occupational Exposures: Exposure to substances like trichloroethylene and aristolochic acid (chemical compounds known for their health risks, especially in relation to cancer).
- Genetic risk factors and others.[2]
Characteristics/Clinical Presentation[edit | edit source]
Presentation is classically described as the triad of:
- Macroscopic haematuria: 60%
- Flank pain: 40%
- Palpable flank mass: 30-40%[3]
This triad presents in patients with renal cell carcinoma, however this triad only found in 10-15% of patients the remaining cases present with signs and symptoms related to the site of distant metastases[4]. That is why there are some cases were discovered by chance with examination[4].
About 25-30% of patients have metastatic disease at the time of diagnosis. Renal cancer most often spreads to the lungs (75%), regional lymph nodes (65%), bones (40%), and liver (40%).[5] The patient may complain of a cough or bone pain secondary to metastasis to the lungs or bone, respectively.
Pathology[edit | edit source]
Renal cell carcinoma (RCC), or renal cancer, is categorized into four major types, determined by cellular origin:
- Clear cell: 70-80%, arises from proximal convoluted tubules
- Papillary: 13-20%, arises from distal convoluted tubules
- Chromophobe: 5%, arises from intercalated cells of collecting ducts[7]
- Collecting duct: 1% of cases[5].
Grading[edit | edit source]
Histological nuclear grading:
The most widely used and most predictive grading system for renal cell cancer specially renal cell carcinoma is the "Fuhrman nuclear grade". The Fuhrman nuclear grade is a system used to classify the aggressiveness of kidney cancer, particularly renal cell carcinoma, based on the microscopic appearance of the cancer cells. It helps in determining the prognosis and potential treatment strategies for the disease with grade I and grade II, have a better prognosis and grade III and grade IV, suggest a poor prognosis as the following:
- Grade 1: Small, round, uniform nuclei, about 10 micrometers or smaller. Nucleoli absent or not clear at 400x magnification.
- Grade 2: Nuclei slightly larger than Grade 1, up to 15 micrometers, mostly uniform with some shape irregularities. Nucleoli may be seen but not distinct at 400x magnification.
- Grade 3: Larger, more irregular nuclei, over 15 micrometers. Nucleoli are clearly visible at 400x magnification.
- Grade 4: Very large, irregularly shaped nuclei. Nucleoli are clearly visible, and cells may have multiple nuclei.
Diagnostic Tests[edit | edit source]
The following tests and procedures may be used:
- Physical exam and health history
- Ultrasound exam
- Blood tests: An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- Urinalysis
- CT scan (CAT scan): A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- MRI (magnetic resonance imaging) - This procedure is also called nuclear magnetic resonance imaging (NMRI).
- Biopsy - a thin needle is inserted into the tumor and a sample of tissue is withdrawn[8].
Treatment Overview[edit | edit source]
Patients with renal cell cancer may work with a team of health care professionals to coordinate their care.eg Urologist, Surgeon, Urologic Oncologists, Medical Oncologists, Radiation Oncologists, Oncology Nurse, Registered Dietician[9]
There are different types of treatment for patients with renal cell cancer. Five types of standard treatment are used:
- Surgery
- Radiation therapy
- Chemotherapy
- Immunotherapy
- Targeted therapy
RCC is primarily treated by surgical interventions. Although aggressive, a radical nephrectomy is the preferred method of treatment for both localized and metastasized diseased. This consists of the removal of:
- Kidney
- Gerota’s fascia: fibroareolar tissue surrounding the kidney and perirenal fat
- Adrenal gland
- Regional lymph nodes
Kidney cancer, when diagnosed at a stage where it has already spread to other organs, is often not curable. The current standard treatment for such advanced stages of kidney cancer involves the use of targeted agents. [10].
- Targeted therapies, which work by targeting the cancer at a cellular level, have expanded the options for the treatment of kidney cancer. Targeted treatments block specific abnormal signals present in kidney cancer cells that allow them to grow. These medications have shown promise in treating kidney cancer that has spread to other areas of the body. The targeted medications Axitinib (Inlyta), Bevacizumab (Avastin), Pazopanib (Votrient), Sorafenib (Nexavar) and Sunitinib (Sutent) block signals that play a role in the growth of blood vessels that provide nutrients to cancer cells and allow cancer cells to spread. Temsirolimus (Torisel) and Everolimus (Afinitor) are targeted medications that block a signal that allows cancer cells to grow and survive. Targeted therapy medications can cause serious side effects, such as: a severe rash, diarrhea, and fatigue
- Whereas targeted therapies specifically block the renal cancer cells from growing and spreading, immunotherapy works in a more general way by using the body's immune system to fight the cancer. Immunotherapy medications include Interferon and Aldesleukin (Proleukin), which are synthetic versions of chemicals made in your body. Side effects of these medications include: chills, fever, nausea, vomiting and loss of appetite[10].
Physical Therapy Management[edit | edit source]
Maintaining physical strength is important while undergoing renal cancer treatment and a physical therapist will be able to provide an exercise plan specifically designed for a patient’s needs.
- If a patient had surgery to remove the tumor, modest exercise can help regain muscle tone and help to rebuild the muscles that were cut, increase that patient’s range of motion, and help to prevent complications that can occur post-surgery such as: respiratory infection, pressure sores, and the formation of a deep vein thrombosis (DVT).
- Exercise can have the additional benefit of reducing stress and depression, which can be common occurrences in patients undergoing cancer treatment.
- Physical therapy can also be used to combat fatigue, which is not only a common symptom of renal cancer but it can be a side effect of treatment (e.g. chemotherapy). Building up endurance can reduce the incidence and severity of fatigue. This will be an important factor in increasing a patient’s independence and ability to maintain a high quality of life.
- Educate the patient regarding his or her diet, which will play an important role throughout the treatment process.
- A systematic review and meta-analysis of randomized clinical trials suggested that intradialytic exercise protocols had positive outcomes in chronic kidney disease patients with poor cardiopulmonary function and reduced exercise tolerance and ventilatory efficiency[11].
Case Reports/ Case Studies[edit | edit source]
- Sciatica leading to the discovery of a renal cell carcinoma
- Atypical presentations and rare metastatic sites of renal cell carcinoma: a review of case reports
- Hereditary leiomyomatosis and renal cell cancer presenting as metastatic kidney cancer at 18 years of age: implications for surveillance
- Renal cancer and Wegener's granulomatosis: a case report
Resources[edit | edit source]
References[edit | edit source]
- ↑ Scelo G, Larose TL. Epidemiology and risk factors for kidney cancer. Journal of Clinical Oncology. 2018 Dec 12;36(36):3574.
- ↑ 2.0 2.1 2.2 Safiri S, Kolahi AA, Mansournia MA, Almasi-Hashiani A, Ashrafi-Asgarabad A, Sullman MJ, Bettampadi D, Qorbani M, Moradi-Lakeh M, Ardalan M, Mokdad A. The burden of kidney cancer and its attributable risk factors in 195 countries and territories, 1990–2017. Scientific Reports. 2020 Aug 17;10(1):13862.
- ↑ 3.0 3.1 Radiopedia Renal cell carcinoma Available from:https://radiopaedia.org/articles/renal-cell-carcinoma-1 (last accessed 1.9.2020)
- ↑ 4.0 4.1 Maestroni U, Gasparro D, Ziglioli F, Guarino G, Campobasso D. Metastatic clear cell renal cell carcinoma: the great pretender and the great dilemma. World Journal of Oncology. 2021 Oct;12(5):178.
- ↑ 5.0 5.1 Goodman CC, Fuller KS. Pathology: Implications for the physical therapist. 3rd ed. St. Louis, Missouri: Saunders Elsevier, 2009.
- ↑ Dana-Farber Cancer Institute . Signs and Symptoms of a Kidney Tumor | Dana-Farber Cancer Institute. Available from: http://www.youtube.com/watch?v=Cq6PAVbquus[last accessed 27/11/2023
- ↑ Muglia VF, Prando A. Renal cell carcinoma: histological classification and correlation with imaging findings. Radiologia brasileira. 2015 May;48:166-74.
- ↑ Low G, Huang G, Fu W, Moloo Z, Girgis S. Review of renal cell carcinoma and its common subtypes in radiology. World journal of radiology. 2016 May 5;8(5):484.
- ↑ National Cancer Institute. What you need to know about kidney cancer: Treatment. http://www.cancer.gov/cancertopics/wyntk/kidney/page8 (accessed 30 Jan 2013).
- ↑ 10.0 10.1 Unverzagt S, Moldenhauer I, Nothacker M, Rossmeissl D, Hadjinicolaou AV, Peinemann F, Greco F, Seliger B. Immunotherapy for metastatic renal cell carcinoma. Cochrane Database of Systematic Reviews. 2017(5).
- ↑ Andrade FP, Rezende PS, Ferreira TS, Borba GC, Müller AM, Rovedder PME. Effects of intradialytic exercise on cardiopulmonary capacity in chronic kidney disease: systematic review and meta-analysis of randomized clinical trials. Scientific Reports. 2019 Dec 5;9(1):18470.
{{