Gait Deviations Associated with Pelvis and Knee Pain Syndromes: Difference between revisions
No edit summary |
No edit summary |
||
| (12 intermediate revisions by 4 users not shown) | |||
| Line 4: | Line 4: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
This article discusses gait deviations associated with pain syndromes in the pelvis and knee. | This article discusses [[gait]] deviations associated with [[Pain Behaviours|pain]] syndromes in the [[pelvis]] and [[knee]]. While this information focuses on certain regions of the body, remember that the human body functions within a [[Kinetic Chain|kinetic chain]]. No one movement is ever completely isolated and without effect on another.<ref name=":1">Howell, D, Gait Deviation Associated with Pain Syndromes in the Pelvis and Knee. Gait Analysis. Plus. 2022</ref> | ||
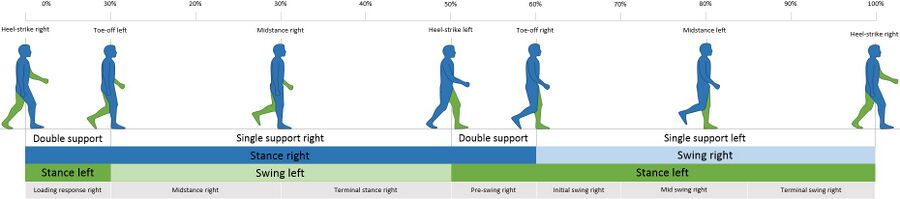
For a review of the gait cycle, please | For a review of the gait cycle, please see [[Gait Cycle|this article]]. For an overview of gait deviations, please review [[Gait Deviations|this article]]. To review common gait terminology and definitions, please see [[Gait Definitions|this article]]. | ||
[[File:Gait cycle.jpg|center|frameless|900x900px]] | [[File:Gait cycle.jpg|center|frameless|900x900px]] | ||
== Pain Syndromes and Gait Deviation == | == Pain Syndromes and Gait Deviation == | ||
Gait deviations are likely related to the development and or associated with musculoskeletal pain syndromes. | Gait deviations are likely related to the development of and / or associated with musculoskeletal pain syndromes. It is often the complaint of pain that will lead a patient to physiotherapy. It is the role of the physiotherapist to educate the patient on the aetiology of their pain while treating and correcting the noted gait deviation.<ref name=":1" /> <blockquote>A '''gait deviation''' is an abnormality in the gait cycle that can effect the trunk, hip, knee, or ankle joint. Gait deviations can stem from increased age and / or certain pathologies. These pathologies can be musculoskeletal or neurological in nature.<ref>Vazquez-Galliano J, Kimawi I, Chang L. [https://now.aapmr.org/biomechanic-of-gait-and-treatment-of-abnormal-gait-patterns/ Biomechanic of Gait and Treatment of Abnormal Gait Patterns]. (2020)</ref> Gait deviations can have a tremendous impact on a patient's [[Quality of Life|quality of life]], morbidity, and mortality.<ref>Ataullah AHM, De Jesus O. Gait Disturbances. [Updated 2021 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan Available:https://www.ncbi.nlm.nih.gov/books/NBK560610/<nowiki/>(accessed 30/05/2022)</ref></blockquote>The most commonly noted gait deviations for pain syndromes include:<ref name=":1" /> | ||
# Decreased gait velocity (most frequent gait deviation for patients with neurological deficits) | # Decreased gait velocity (most frequent gait deviation for patients with [[Neurological Disorders|neurological]] deficits) | ||
# Decreased vertical oscillation of centre of mass | # Decreased vertical oscillation of centre of mass | ||
# Delayed heel off | # Delayed heel off | ||
== Walking Speed, the Sixth Vital Sign == | == Walking Speed, the Sixth Vital Sign == | ||
According to a 2009 paper by Fritz, walking speed (ie gait velocity) is "almost the perfect measure." | According to a 2009 paper by Fritz,<ref name=":0" /> walking speed (ie gait velocity) is "almost the perfect measure." Patient self-selected walking speed has been found to be a reliable, valid, sensitive and specific measure which correlates with functional ability, and [[balance]] confidence.<ref name=":0">Fritz S, Lusardi M. White paper:“[https://digitalcommons.sacredheart.edu/cgi/viewcontent.cgi?article=1134&=&context=pthms_fac&=&sei-redir=1&referer=https%253A%252F%252Fscholar.google.com%252Fscholar%253Fhl%253Den%2526as_sdt%253D0%25252C44%2526q%253DWalking%252Bspeed%25253A%252BThe%252BSixth%252BVital%252BSign%25252C%252BStacy%252BFritz%25252C%252B2009%2526btnG%253D#search=%22Walking%20speed%3A%20Sixth%20Vital%20Sign%2C%20Stacy%20Fritz%2C%202009%22 walking speed: the sixth vital sign]”. Journal of geriatric physical therapy. 2009 Jan 1;32(2):2-5.</ref> <blockquote>"Walking speed, like [[Blood Pressure|blood pressure]], may be a general indicator that can predict future events and reflect various underlying physiological processes. While walking speed cannot stand alone as the only predictor of functional abilities, just at blood pressure is not the only sign of [[Coronary Artery Disease (CAD)|heart disease]]; walking speed can be used as a functional “[[Vital Signs|vital sign]]” to help determine outcomes such as functional status, discharge location, and the need for rehabilitation."<ref name=":0" /></blockquote>'''Applications of walking speed as a clinical measure''':<ref name=":0" /><ref>Salbach NM, MacKay-Lyons M, Solomon P, Howe JA, McDonald A, Bayley MT, Veitch S, Sivarajah L, Cacoilo J, Mihailidis A. [https://www.tandfonline.com/doi/pdf/10.1080/09638288.2020.1867653?needAccess=true&role=button The role of theory to develop and evaluate a toolkit to increase clinical measurement and interpretation of walking speed and distance in adults post-stroke]. Disability and Rehabilitation. 2022 Jul 3;44(14):3719-35.</ref> | ||
# Has the potential to predict future health status and functional decline | # Has the potential to predict future health status and functional decline | ||
| Line 23: | Line 23: | ||
# Reflects both patient functional and physiological changes | # Reflects both patient functional and physiological changes | ||
# Is a factor in determining potential for rehabilitation | # Is a factor in determining potential for rehabilitation | ||
# Aids in prediction of falls and fear of falling | # Aids in prediction of [[falls]] and [[Fear of Falling|fear of falling]] | ||
# Walking speed progression has been linked to clinical meaningful changes in quality of life | # Walking speed progression has been linked to clinical meaningful changes in quality of life | ||
According to Fritz et al 2009, the average walking speed for [[Older People - An Introduction|geriatric adults]] is 1-1.4 m/sec.<ref name=":0" /> The preferred average walking speed in healthy adults, aged up to 50 years, is 1.4 m/sec.<ref name=":5" /> This suggests that deviant gait velocity is measured at a pace slower than 1-1.4 m/sec.<ref name=":1" /> | |||
The average stride length in healthy adults ranges between 150 and 170 cm. The average cadence in young adults ranges between 115 and 120 steps/min. Geriatric adults prefer a 40 % wider step width than younger adults. A 2017 study found that ageing is "associated with a decline in gait speed and step length whereas cadence remains relatively stable."<ref name=":5">Pirker W, Katzenschlager R. [https://link.springer.com/article/10.1007/s00508-016-1096-4 Gait disorders in adults and the elderly]. Wiener Klinische Wochenschrift. 2017 Feb;129(3):81-95.</ref> | |||
Please watch the following video for further discussion on walking speed and how to measure it in the clinic using the 10-metre walk test. | Please watch the following video for further discussion on walking speed and how to measure it in the clinic using the 10-metre walk test. | ||
| Line 36: | Line 38: | ||
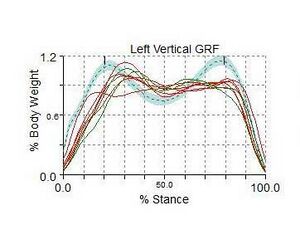
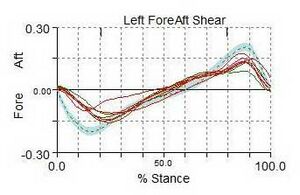
'''Ground reaction force''' is a summation of all the forces transmitted from the ground up into the body.<ref name=":1" /> Ground reaction force is influenced from all directions: vertical, anterior-posterior, and medial-lateral. These forces are typically measured and recorded using a three-dimensional force plate.<ref name=":2">Yu L, Mei Q, Xiang L, et al. [https://www.frontiersin.org/articles/10.3389/fbioe.2021.629809/full#refer1 Principal Component Analysis of the Running Ground Reaction Forces With Different Speeds]. Front. Bioeng. Biotechnol.. 2021; 9:629809.</ref><ref>Tesio, L., & Rota, V. (2019). [https://www.frontiersin.org/articles/10.3389/fneur.2019.00999/full The Motion of Body Center of Mass During Walking: A Review Oriented to Clinical Applications.] Front Neurol, 10, 999. </ref> | '''Ground reaction force''' is a summation of all the forces transmitted from the ground up into the body.<ref name=":1" /> Ground reaction force is influenced from all directions: vertical, anterior-posterior, and medial-lateral. These forces are typically measured and recorded using a three-dimensional force plate.<ref name=":2">Yu L, Mei Q, Xiang L, et al. [https://www.frontiersin.org/articles/10.3389/fbioe.2021.629809/full#refer1 Principal Component Analysis of the Running Ground Reaction Forces With Different Speeds]. Front. Bioeng. Biotechnol.. 2021; 9:629809.</ref><ref>Tesio, L., & Rota, V. (2019). [https://www.frontiersin.org/articles/10.3389/fneur.2019.00999/full The Motion of Body Center of Mass During Walking: A Review Oriented to Clinical Applications.] Front Neurol, 10, 999. </ref> | ||
[[File:Braking forces.jpeg|thumb|Example of an anterior-posterior ground reaction force.]] | [[File:Braking forces.jpeg|thumb|Example of an anterior-posterior ground reaction force.]] | ||
During walking, the '''vertical ground reaction force''' is the largest component of the total ground reaction force. This creates forces greater than a person's total body weight per step. The graphed curve of the vertical ground reaction force consists of two peaks: the impact loading<ref name=":1" /> or passive (weight acceptance as the heel strikes the ground) peak and the active (push off) peak.<ref name=":2" /> <ref name=":3">Jiang X, Napier C, Hannigan B, Eng JJ, Menon C. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7436236/ Estimating vertical ground reaction force during walking using a single inertial sensor]. Sensors. 2020 Jan;20(15):4345.</ref>The passive peak is caused by the foot pushing against the ground, whereas the active peak is caused by the active force applied by the foot as it pushes away from the ground. The '''anterior-posterior ground reaction force''' includes braking peak and propulsion peak.<ref name=":2" /> The unique patterns of these peaks illustrate the load forces at the joints and muscles of the lower extremity. These forces felt throughout the limb can influence the development or exacerbation of musculoskeletal overuse or stress injuries.<ref name=":3" /><ref name=":4">Lewis CL, Halverstadt AL, Graber KA, Perkins Z, Keiser E, Belcher H, Khuu A, Loverro KL. [https://www.ncbi.nlm.nih.gov/pmc/articles/pmc8421535/ Individuals With Pre-arthritic Hip Pain Walk With Hip Motion Alterations Common in Individuals With Hip OA]. Frontiers in Sports and Active Living. 2021;3.</ref> | During walking, the '''vertical ground reaction force''' is the largest component of the total ground reaction force. This creates forces greater than a person's total body weight per step. The graphed curve of the vertical ground reaction force consists of two peaks: the impact loading<ref name=":1" /> or passive (weight acceptance as the heel strikes the ground) peak and the active (push off) peak.<ref name=":2" /> <ref name=":3">Jiang X, Napier C, Hannigan B, Eng JJ, Menon C. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7436236/ Estimating vertical ground reaction force during walking using a single inertial sensor]. Sensors. 2020 Jan;20(15):4345.</ref> The passive peak is caused by the foot pushing against the ground, whereas the active peak is caused by the active force applied by the foot as it pushes away from the ground. The '''anterior-posterior ground reaction force''' includes braking peak and propulsion peak.<ref name=":2" /> The unique patterns of these peaks illustrate the load forces at the joints and muscles of the lower extremity. These forces felt throughout the limb can influence the development or exacerbation of musculoskeletal [[Overuse Injuries in Sport|overuse]] or [[Stress Fractures|stress injuries]].<ref name=":3" /><ref name=":4">Lewis CL, Halverstadt AL, Graber KA, Perkins Z, Keiser E, Belcher H, Khuu A, Loverro KL. [https://www.ncbi.nlm.nih.gov/pmc/articles/pmc8421535/ Individuals With Pre-arthritic Hip Pain Walk With Hip Motion Alterations Common in Individuals With Hip OA]. Frontiers in Sports and Active Living. 2021;3.</ref> | ||
When interpreting a ground reaction curve, the steeper the curve the more significant the impact forces. The curve on the anterior-posterior curve (the breaking forces) will be negative. In general, the greater the forces, the greater risk for stress or overuse injuries.<ref name=":1" /><ref name=":4" /> | When interpreting a ground reaction curve, the steeper the curve the more significant the impact forces. The curve on the anterior-posterior curve (the breaking forces) will be negative. In general, the greater the forces, the greater risk for stress or overuse injuries.<ref name=":1" /><ref name=":4" /> | ||
Please view the following video for a quick yet detailed overview of ground reaction forces during the human gait cycle. This video provides excellent | Please view the following video for a quick yet detailed overview of ground reaction forces during the human gait cycle. This video provides excellent visualisation of how ground reaction forces shift in different directions as the person moves through space. | ||
{{#ev:youtube| Y2RHvicAM2o |500}}<ref>JYouTube. Ground Reaction Force During the Gait Cycle | Alexandra Kopelovich. | {{#ev:youtube| Y2RHvicAM2o |500}}<ref>JYouTube. Ground Reaction Force During the Gait Cycle | Alexandra Kopelovich. | ||
| Line 54: | Line 56: | ||
|'''Increased vertical oscillation of [[Centre of Gravity|centre of mass]]''' | |'''Increased vertical oscillation of [[Centre of Gravity|centre of mass]]''' | ||
* "Too much up and down motion" | * "Too much up and down motion" | ||
|Choose a fixed location such as the top of the head, sacrum, or belt line. | |Choose a fixed location such as the top of the head, sacrum, or belt line. Compare the highest point during swing phase to the lowest point during stance phase. | ||
* When running: 6-8 cm or 2-3 inches<ref>Souza RB. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4714754/ An evidence-based videotaped running biomechanics analysis]. Physical Medicine and Rehabilitation Clinics. 2016 Feb 1;27(1):217-36.</ref> | * When running: 6-8 cm or 2-3 inches is normal<ref>Souza RB. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4714754/ An evidence-based videotaped running biomechanics analysis]. Physical Medicine and Rehabilitation Clinics. 2016 Feb 1;27(1):217-36.</ref> | ||
* When walking: 9.5cm or 3.5 inches<ref>Bogey RA, Barnes LA, Perry J. Computer algorithms to characterize individual subject EMG profiles during gait. Archives of physical medicine and rehabilitation. 1992 Sep 1;73(9):835-41.</ref> | * When walking: 9.5cm or 3.5 inches is normal<ref>Bogey RA, Barnes LA, Perry J. Computer algorithms to characterize individual subject EMG profiles during gait. Archives of physical medicine and rehabilitation. 1992 Sep 1;73(9):835-41.</ref> | ||
| | | | ||
* Bounding or bouncy gait | * Bounding or bouncy gait | ||
* | * Is considered deviant if decreasing the magnitude of the vertical oscillation of centre of mass decreases or eliminates pain symptoms | ||
| | | | ||
* Increased float time in running | * Increased float time in running | ||
| Line 68: | Line 70: | ||
|- | |- | ||
|'''Decreased vertical oscillation of centre of mass''' | |'''Decreased vertical oscillation of centre of mass''' | ||
| | |Same as above | ||
| | | | ||
* Shuffling gait | * Shuffling gait | ||
| Line 79: | Line 81: | ||
|- | |- | ||
|'''Contralateral pelvic drop''' | |'''Contralateral pelvic drop''' | ||
|During stance phase, a line drawn between the posterior superior iliac spines (PSIS | |During stance phase, a line drawn between the posterior superior iliac spines (PSIS) should deviate no more than four degrees inferiorly | ||
|During stance phase, the line between the | |During stance phase, the line between the PSISs will deviate inferiorly more than four degrees. | ||
* Can be related to an anatomically long leg during stance phase | * Can be related to an anatomically long leg during stance phase | ||
| Line 86: | Line 88: | ||
* Lateral pelvic shift | * Lateral pelvic shift | ||
* Absence of daylight between the thighs and knees | * Absence of daylight between the thighs and knees | ||
* Foot strike occurs across midline of the body | * Foot strike occurs across the midline of the body | ||
* Oblique popliteal skin crease | * Oblique popliteal skin crease | ||
* Excessive medial femoral internal rotation | * Excessive medial femoral internal rotation | ||
| Line 95: | Line 97: | ||
ie: hip or pelvic hiking | ie: hip or pelvic hiking | ||
|During stance phase, a line drawn between the posterior superior iliac spines (PSIS | |During stance phase, a line drawn between the posterior superior iliac spines (PSIS) should deviate no more than four degrees superiorly | ||
|During stance phase, the line between the | |During stance phase, the line between the PSISs will deviate superiorly more than four degrees. | ||
* Commonly seen in patient with neurological impairments | * Commonly seen in patient with neurological impairments | ||
| Line 112: | Line 114: | ||
* Lateral pelvic drop | * Lateral pelvic drop | ||
* Lateral pelvic shift | * Lateral pelvic shift | ||
* Excessive | * Excessive medial femoral rotation | ||
* Oblique popliteal skin crease | * Oblique popliteal skin crease | ||
* Genu valgus | * Genu valgus | ||
| Line 131: | Line 133: | ||
|'''Popliteal skin crease''' | |'''Popliteal skin crease''' | ||
* Excessive femoral medial rotation | * Excessive femoral medial rotation | ||
|When viewed from behind during stance phase, the skin crease on the back of the knee should be horizontal | |When viewed from behind during stance phase, the skin crease on the back of the knee should be horizontal | ||
|When viewed from behind, the skin crease will be oblique from superior-lateral to inferior-medial (inferring there is excessive movement of the femur into medial rotation). | |When viewed from behind, the skin crease will be oblique from superior-lateral to inferior-medial (inferring there is excessive movement of the femur into medial rotation). | ||
| Line 140: | Line 142: | ||
* No daylight between the knees | * No daylight between the knees | ||
* Genu valgus | * Genu valgus | ||
* | * In-toe gait | ||
* Heel whip | * Heel whip | ||
* Excessive pronation | * Excessive pronation | ||
| Line 146: | Line 148: | ||
|'''Varus thrust''' | |'''Varus thrust''' | ||
|During stance phase, when viewed from front or behind, there should be little to no lateral/medial deviation or translation of the knee | |During stance phase, when viewed from front or behind, there should be little to no lateral/medial deviation or translation of the knee | ||
|During stance phase, when viewed from front or behind, there is a high-velocity small-amplitude lateral deviation of the knee with a rapid return to neutral alignment | |During stance phase, when viewed from front or behind, there is a high-velocity small-amplitude lateral deviation of the knee with a rapid return to neutral alignment | ||
| | | | ||
* Excessive lateral lean of the trunk | * Excessive lateral lean of the trunk | ||
| Line 165: | Line 167: | ||
* Back pain | * Back pain | ||
* Knee pain | * Knee pain | ||
* Medial tibial stress syndrome | * [[Medial Tibial Stress Syndrome|Medial tibial stress syndrome]] | ||
* Achilles pain in runners | * Achilles pain in runners | ||
* Plantar heel pain syndrome | * [[Plantar Heel Pain|Plantar heel pain syndrome]] | ||
|- | |- | ||
|'''Decreased vertical oscillation of centre of mass''' | |'''Decreased vertical oscillation of centre of mass''' | ||
| Line 180: | Line 182: | ||
* Gluteal tendinopathy | * Gluteal tendinopathy | ||
* Piriformis syndrome | * Piriformis syndrome | ||
* Anterior and or lateral knee pain | * Anterior and / or lateral knee pain | ||
* Patellofemoral arthralgia | * Patellofemoral arthralgia | ||
* [[Iliotibial Band Syndrome|Iliotibial band syndrome]] | * [[Iliotibial Band Syndrome|Iliotibial band syndrome]] | ||
| Line 197: | Line 199: | ||
|- | |- | ||
|'''Lack of knee separation''' | |'''Lack of knee separation''' | ||
* " | * "Absence of daylight" between thighs or knees | ||
| | | | ||
* Gluteal tendinopathy | * Gluteal tendinopathy | ||
| Line 265: | Line 267: | ||
<references /> | <references /> | ||
[[Category: | [[Category:Plus Content]] | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Gait]] | [[Category:Gait]] | ||
[[Category:Pain]] | [[Category:Pain]] | ||
Latest revision as of 03:11, 30 October 2023
Top Contributors - Stacy Schiurring, Lucinda hampton, Jess Bell and Kim Jackson
Introduction[edit | edit source]
This article discusses gait deviations associated with pain syndromes in the pelvis and knee. While this information focuses on certain regions of the body, remember that the human body functions within a kinetic chain. No one movement is ever completely isolated and without effect on another.[1]
For a review of the gait cycle, please see this article. For an overview of gait deviations, please review this article. To review common gait terminology and definitions, please see this article.
Pain Syndromes and Gait Deviation[edit | edit source]
Gait deviations are likely related to the development of and / or associated with musculoskeletal pain syndromes. It is often the complaint of pain that will lead a patient to physiotherapy. It is the role of the physiotherapist to educate the patient on the aetiology of their pain while treating and correcting the noted gait deviation.[1]
A gait deviation is an abnormality in the gait cycle that can effect the trunk, hip, knee, or ankle joint. Gait deviations can stem from increased age and / or certain pathologies. These pathologies can be musculoskeletal or neurological in nature.[2] Gait deviations can have a tremendous impact on a patient's quality of life, morbidity, and mortality.[3]
The most commonly noted gait deviations for pain syndromes include:[1]
- Decreased gait velocity (most frequent gait deviation for patients with neurological deficits)
- Decreased vertical oscillation of centre of mass
- Delayed heel off
Walking Speed, the Sixth Vital Sign[edit | edit source]
According to a 2009 paper by Fritz,[4] walking speed (ie gait velocity) is "almost the perfect measure." Patient self-selected walking speed has been found to be a reliable, valid, sensitive and specific measure which correlates with functional ability, and balance confidence.[4]
"Walking speed, like blood pressure, may be a general indicator that can predict future events and reflect various underlying physiological processes. While walking speed cannot stand alone as the only predictor of functional abilities, just at blood pressure is not the only sign of heart disease; walking speed can be used as a functional “vital sign” to help determine outcomes such as functional status, discharge location, and the need for rehabilitation."[4]
Applications of walking speed as a clinical measure:[4][5]
- Has the potential to predict future health status and functional decline
- Can be used to predict future hospitalisation, discharge location and patient mortality
- Reflects both patient functional and physiological changes
- Is a factor in determining potential for rehabilitation
- Aids in prediction of falls and fear of falling
- Walking speed progression has been linked to clinical meaningful changes in quality of life
According to Fritz et al 2009, the average walking speed for geriatric adults is 1-1.4 m/sec.[4] The preferred average walking speed in healthy adults, aged up to 50 years, is 1.4 m/sec.[6] This suggests that deviant gait velocity is measured at a pace slower than 1-1.4 m/sec.[1]
The average stride length in healthy adults ranges between 150 and 170 cm. The average cadence in young adults ranges between 115 and 120 steps/min. Geriatric adults prefer a 40 % wider step width than younger adults. A 2017 study found that ageing is "associated with a decline in gait speed and step length whereas cadence remains relatively stable."[6]
Please watch the following video for further discussion on walking speed and how to measure it in the clinic using the 10-metre walk test.
Ground Reaction Forces[edit | edit source]
Ground reaction force is a summation of all the forces transmitted from the ground up into the body.[1] Ground reaction force is influenced from all directions: vertical, anterior-posterior, and medial-lateral. These forces are typically measured and recorded using a three-dimensional force plate.[8][9]
During walking, the vertical ground reaction force is the largest component of the total ground reaction force. This creates forces greater than a person's total body weight per step. The graphed curve of the vertical ground reaction force consists of two peaks: the impact loading[1] or passive (weight acceptance as the heel strikes the ground) peak and the active (push off) peak.[8] [10] The passive peak is caused by the foot pushing against the ground, whereas the active peak is caused by the active force applied by the foot as it pushes away from the ground. The anterior-posterior ground reaction force includes braking peak and propulsion peak.[8] The unique patterns of these peaks illustrate the load forces at the joints and muscles of the lower extremity. These forces felt throughout the limb can influence the development or exacerbation of musculoskeletal overuse or stress injuries.[10][11]
When interpreting a ground reaction curve, the steeper the curve the more significant the impact forces. The curve on the anterior-posterior curve (the breaking forces) will be negative. In general, the greater the forces, the greater risk for stress or overuse injuries.[1][11]
Please view the following video for a quick yet detailed overview of ground reaction forces during the human gait cycle. This video provides excellent visualisation of how ground reaction forces shift in different directions as the person moves through space.
Gait Deviations[1][edit | edit source]
| Gait Deviation | Expected Movement Pattern | Deviant Movement Pattern | Secondary Signs Associated with Deviant Movement |
|---|---|---|---|
Increased vertical oscillation of centre of mass
|
Choose a fixed location such as the top of the head, sacrum, or belt line. Compare the highest point during swing phase to the lowest point during stance phase. |
|
|
| Decreased vertical oscillation of centre of mass | Same as above |
|
|
| Contralateral pelvic drop | During stance phase, a line drawn between the posterior superior iliac spines (PSIS) should deviate no more than four degrees inferiorly | During stance phase, the line between the PSISs will deviate inferiorly more than four degrees.
|
|
| Contralateral pelvic elevation
|
During stance phase, a line drawn between the posterior superior iliac spines (PSIS) should deviate no more than four degrees superiorly | During stance phase, the line between the PSISs will deviate superiorly more than four degrees.
|
|
Lack of knee separation
|
Unless morbidly obese, when walking and viewed from front or behind, there should be a space or "daylight" between the knees and thighs. | When walking and viewed from front or behind, there is an absence of space or "daylight" between the knees or thighs.
|
|
| Foot crossing the midline | When walking and viewed from front or behind, the opposite foot strike should be visible and not cross a vertical line which travels from the belly button to the ground.
|
When walking and viewed from behind, the opposite foot strike is not visible because the foot crosses the vertical line.
|
|
Popliteal skin crease
|
When viewed from behind during stance phase, the skin crease on the back of the knee should be horizontal | When viewed from behind, the skin crease will be oblique from superior-lateral to inferior-medial (inferring there is excessive movement of the femur into medial rotation).
|
|
| Varus thrust | During stance phase, when viewed from front or behind, there should be little to no lateral/medial deviation or translation of the knee | During stance phase, when viewed from front or behind, there is a high-velocity small-amplitude lateral deviation of the knee with a rapid return to neutral alignment |
|
Pain Syndromes Associated with Gait Deviations[1][edit | edit source]
| Gait Deviation | Associated Pain
and Pain Syndromes |
|---|---|
Increased vertical oscillation of centre of mass
|
|
| Decreased vertical oscillation of centre of mass |
|
| Contralateral pelvic drop |
|
| Contralateral pelvic elevation |
|
Lack of knee separation
|
|
| Foot crossing the midline |
|
Popliteal skin crease
|
|
| Varus thrust |
|
Resources[edit | edit source]
Recommended videos of gait deviations:
- Gait Deviations: Hip, Pelvis, Trunk
- Gait Deviations: Knee Joint
Recommended Journal Articles:
- Fritz S, Lusardi M. White paper:“walking speed: the sixth vital sign”. Journal of geriatric physical therapy. 2009 Jan 1;32(2):2-5.
- Tesio, L., & Rota, V. (2019). The Motion of Body Center of Mass During Walking: A Review Oriented to Clinical Applications. Front Neurol, 10, 999.
Clinical Resources:
- Directions for the 10-metre Walk Test
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Howell, D, Gait Deviation Associated with Pain Syndromes in the Pelvis and Knee. Gait Analysis. Plus. 2022
- ↑ Vazquez-Galliano J, Kimawi I, Chang L. Biomechanic of Gait and Treatment of Abnormal Gait Patterns. (2020)
- ↑ Ataullah AHM, De Jesus O. Gait Disturbances. [Updated 2021 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan Available:https://www.ncbi.nlm.nih.gov/books/NBK560610/(accessed 30/05/2022)
- ↑ 4.0 4.1 4.2 4.3 4.4 Fritz S, Lusardi M. White paper:“walking speed: the sixth vital sign”. Journal of geriatric physical therapy. 2009 Jan 1;32(2):2-5.
- ↑ Salbach NM, MacKay-Lyons M, Solomon P, Howe JA, McDonald A, Bayley MT, Veitch S, Sivarajah L, Cacoilo J, Mihailidis A. The role of theory to develop and evaluate a toolkit to increase clinical measurement and interpretation of walking speed and distance in adults post-stroke. Disability and Rehabilitation. 2022 Jul 3;44(14):3719-35.
- ↑ 6.0 6.1 Pirker W, Katzenschlager R. Gait disorders in adults and the elderly. Wiener Klinische Wochenschrift. 2017 Feb;129(3):81-95.
- ↑ YouTube. Why does your WALKING SPEED matter? (Walk Talk - Episode 1) | Mission Gait. Available from: https://www.youtube.com/watch?v=aFsjfZH6VTk [last accessed 30/05/2022]
- ↑ 8.0 8.1 8.2 Yu L, Mei Q, Xiang L, et al. Principal Component Analysis of the Running Ground Reaction Forces With Different Speeds. Front. Bioeng. Biotechnol.. 2021; 9:629809.
- ↑ Tesio, L., & Rota, V. (2019). The Motion of Body Center of Mass During Walking: A Review Oriented to Clinical Applications. Front Neurol, 10, 999.
- ↑ 10.0 10.1 Jiang X, Napier C, Hannigan B, Eng JJ, Menon C. Estimating vertical ground reaction force during walking using a single inertial sensor. Sensors. 2020 Jan;20(15):4345.
- ↑ 11.0 11.1 Lewis CL, Halverstadt AL, Graber KA, Perkins Z, Keiser E, Belcher H, Khuu A, Loverro KL. Individuals With Pre-arthritic Hip Pain Walk With Hip Motion Alterations Common in Individuals With Hip OA. Frontiers in Sports and Active Living. 2021;3.
- ↑ JYouTube. Ground Reaction Force During the Gait Cycle | Alexandra Kopelovich. Available from: https://www.youtube.com/watch?v=Y2RHvicAM2o [last accessed 29/05/2022]
- ↑ Souza RB. An evidence-based videotaped running biomechanics analysis. Physical Medicine and Rehabilitation Clinics. 2016 Feb 1;27(1):217-36.
- ↑ Bogey RA, Barnes LA, Perry J. Computer algorithms to characterize individual subject EMG profiles during gait. Archives of physical medicine and rehabilitation. 1992 Sep 1;73(9):835-41.
- ↑ JYouTube. Gait Deviations: Hip, Pelvis, Trunk | Alexandra Kopelovich. Available from: https://www.youtube.com/watch?v=N_zt5fC6SOE [last accessed 30/05/2022]
- ↑ JYouTube. Gait Deviations: Compensatory Knee Joint Strategies | Alexandra Kopelovich. Available from: https://www.youtube.com/watch?v=Jz8ko_uVWII [last accessed 30/05/2022]
- ↑ JYouTube. Gait Deviations: Knee Joint Complex Secondary to Knee Joint Dysfunction | Alexandra Kopelovich. Available from: https://www.youtube.com/watch?v=T4SdJxzPdUo [last accessed 30/05/2022]