Wallerian Degeneration: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (12 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User: | <div class="editorbox"> '''Original Editor '''- [[User:Anthonia Abraham|Anthonia Abraham]] <br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
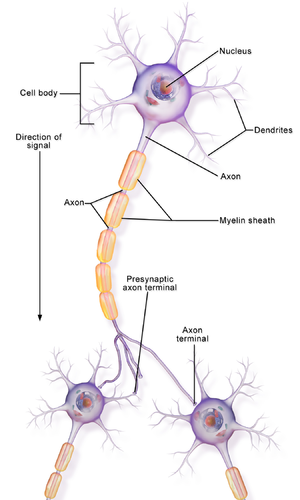
[[File:Neuron Part 1.png|right|frameless]] | |||
Wallerian degeneration is an active process of anterograde degeneration of the distal end of an [[Axons|axon]] that is a result of a [[Nerve Injury Rehabilitation|nerve lesion]].<ref>Conforti L, Gilley J, Coleman MP. Wallerian degeneration: an emerging axon death pathway linking injury and disease. Nature Reviews Neuroscience. 2014 Jun;15(6):394-409.</ref> It occurs between 7 to 21 days after the lesion occurs. After the 21st day, acute nerve degeneration will show on the electromyograph. Although primarily an anterograde process, there is evidence that retrograde degeneration (Wallerian-like) can also be involved, affecting the neuron's cell body and proximal part of the axon. | |||
Within a [[Neurone|nerve]], each axon is surrounded by a layer of connective tissue called the endoneurium. The axons are bundled together into groups called fascicles, and each fascicle is wrapped in a layer of connective tissue called the perineurium. Finally, the entire nerve is wrapped in a layer of connective tissue called the epineurium.<ref>Purves D, Augustine GJ, Fitzpatrick D, Hall WC, LaMantia AS, McNamara JO, White LE.[https://archive.org/details/neuroscienceissu00purv ''Neuroscience''] (4 ed.). Sinauer Associates. 2008 pp. [https://archive.org/details/neuroscienceissu00purv/page/n36 11]–20. </ref> | |||
== Mechanism of Injury == | |||
The pathological process of Wallerian degeneration is in 3 stages; | |||
'''Axon Degeneration''' | |||
Within approximately 30 minutes of injury, there is a separation of the proximal and distal ends of the nerve. After a short latency period, the transected membranes are sealed until degeneration which is marked by the formation of axonal sprouts. This occurs in less than a day and allows for nerve renervation and regeneration | |||
'''Myelin Clearance''' | |||
This occurs by the 7th day when macrophages are signaled by the Schwann cells to clean up axonal and myelin debris.<ref>Gaudet AD, Popovich PG &Ramer MS. Wallerian degeneration: Gaining perspective on inflammatory events after peripheral nerve injury.Journal of Neuroinflammation.2011 Available from.https://jneuroinflammation.biomedcentral.com/articles/10.1186/1742-2094-8-110 (accessed on 06/04/2021)</ref> Usually, the rate of clearance is slower in the [[Introduction to Neuroanatomy|Central Nervous System]](CNS) than in the Peripheral Nervous System (PNS) due to the clearance rate of myelin. Another reason for the different rates is the change in permeability of the blood-tissue barrier in the two systems. In PNS, the permeability increases throughout the distal stump, but the barrier disruption in CNS is limited to just the site of injury. Also in the CNS, [[Glial Cells|oligodendrocytes]] inhibit regeneration. | |||
'''Regeneration''' | |||
If soma/ cell body is damaged, a neuron cannot regenerate. However, if the injury is at the end of the axon, at a growth of 1mm per day, the distal segment undergoes granular disintegration over several days to weeks and cytoplasmic elements begin to accumulate.<ref>Coleman MP, Conforti L, Buckmaster EA, Tarlton A, Ewing RM, Brown MC, Lyon MF, Perry VH (August 1998). [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC21448 "An 85-kb tandem triplication in the slow Wallerian degeneration (Wlds) mouse"]. ''Proceedings of the National Academy of Sciences of the United States of America''. '''95''' (17): 9985–90. Bibcode:[https://ui.adsabs.harvard.edu/abs/1998PNAS...95.9985C 1998PNAS...95.9985C]. doi:[https://doi.org/10.1073%2Fpnas.95.17.9985 10.1073/pnas.95.17.9985]. PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC21448 21448]. PMID [https://pubmed.ncbi.nlm.nih.gov/9707587 9707587].</ref>{{#ev:youtube|EcX7DWjC-7o}}<ref>Medical & Exercise Physiology School.Wallerian degeneration/ regeneration process of nerve fiber/axon cut and progressive response. Available from https://www.youtube.com/watch?v=kbzYML05Vac (last accessed 5 March 2021)</ref> | |||
{{#ev:youtube|P02ea4jf50g}}<ref>The Young Orthopod. Nerve Regeneration. Available from https://www.https://www.youtube.com/watch?v=P02ea4jf50g&t=192s (last accessed 6 March 2021)</ref> | |||
== Clinical Presentation == | == Clinical Presentation == | ||
Presentations of nerve damage may include: | |||
* Reduced or loss of function in associated structures to damaged nerves | |||
* Gradual onset of numbness, prickling or tingling in feet or hands, which can spread upward into legs and arms | |||
* | |||
* Gradual onset of numbness, prickling | |||
* Sharp, jabbing, throbbing, freezing, or burning pain | * Sharp, jabbing, throbbing, freezing, or burning pain | ||
* Extreme sensitivity to touch | * Extreme sensitivity to touch | ||
* Lack of coordination and falling | * Lack of [[Coordination Exercises|coordination]] and [[Falls|falling]] | ||
* Muscle weakness or paralysis if motor nerves are affected | * Muscle weakness or paralysis if [[Motor Neurone|motor nerves]] are affected | ||
* Neuromatous or causalgia pain | * Neuromatous or causalgia pain | ||
== Diagnostic | == Diagnostic Procedures == | ||
* Nerve | * Electromyography | ||
* | |||
* Nerve conduction studies | |||
* [[Pain Assessment|Pain assessment]] | |||
* Sensation deficit and [[skin]] condition tests | |||
* Muscle strength/loss | |||
* Functional deficits<br> | |||
== Outcome Measures == | == Outcome Measures == | ||
Depends on various criteria but could include: | Depends on various criteria including pain and psychosocial skills but could include: | ||
* [[Muscle Strength|Oxford scale]] | * [[Muscle Strength Testing|Oxford scale]] | ||
* [[Visual Analogue Scale|Visual analogue scale]] | * [[Visual Analogue Scale|Visual analogue scale]] | ||
* [[Short-form McGill Pain Questionnaire|Short form McGill]] pain questionnaire | * [[Short-form McGill Pain Questionnaire|Short form McGill]] pain questionnaire | ||
(see [[Outcome Measures|Outcome Measures Database]]) | (see [[Outcome Measures|Outcome Measures Database]]) | ||
== Management / Interventions == | == Management / Interventions == | ||
See [[Nerve Injury Rehabilitation]] | |||
Cryotherapy<ref>https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4315870/</ref>, | Wallerian Degeneration can instigate a nerve repair mechanism. Managing nerve damage can include the use of :[[Cryotherapy]]<ref>Hsu M,and Stevenson FF.Wallerian Degeneration and Recovery of Motor Nerves after Multiple Focused Cold Therapies. US National Library of Medicine.National Institutes of Health.2015 ; 51(2): 268–275.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4315870/ (accessed on 6/04/2021)</ref>, [[Therapeutic Exercise|Exercise,]] Neurorehabilitation, and [[Surgery and General Anaesthetic|Surgery.]] | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Neurology]] | |||
[[Category:Rehabilitation]] | |||
[[Category:Physiology]] | |||
[[Category:Conditions]] | |||
Latest revision as of 13:31, 4 May 2023
Top Contributors - Anthonia Abraham, Kim Jackson, Cindy John-Chu and Lucinda hampton
Clinically Relevant Anatomy[edit | edit source]
Wallerian degeneration is an active process of anterograde degeneration of the distal end of an axon that is a result of a nerve lesion.[1] It occurs between 7 to 21 days after the lesion occurs. After the 21st day, acute nerve degeneration will show on the electromyograph. Although primarily an anterograde process, there is evidence that retrograde degeneration (Wallerian-like) can also be involved, affecting the neuron's cell body and proximal part of the axon.
Within a nerve, each axon is surrounded by a layer of connective tissue called the endoneurium. The axons are bundled together into groups called fascicles, and each fascicle is wrapped in a layer of connective tissue called the perineurium. Finally, the entire nerve is wrapped in a layer of connective tissue called the epineurium.[2]
Mechanism of Injury[edit | edit source]
The pathological process of Wallerian degeneration is in 3 stages;
Axon Degeneration
Within approximately 30 minutes of injury, there is a separation of the proximal and distal ends of the nerve. After a short latency period, the transected membranes are sealed until degeneration which is marked by the formation of axonal sprouts. This occurs in less than a day and allows for nerve renervation and regeneration
Myelin Clearance
This occurs by the 7th day when macrophages are signaled by the Schwann cells to clean up axonal and myelin debris.[3] Usually, the rate of clearance is slower in the Central Nervous System(CNS) than in the Peripheral Nervous System (PNS) due to the clearance rate of myelin. Another reason for the different rates is the change in permeability of the blood-tissue barrier in the two systems. In PNS, the permeability increases throughout the distal stump, but the barrier disruption in CNS is limited to just the site of injury. Also in the CNS, oligodendrocytes inhibit regeneration.
Regeneration
If soma/ cell body is damaged, a neuron cannot regenerate. However, if the injury is at the end of the axon, at a growth of 1mm per day, the distal segment undergoes granular disintegration over several days to weeks and cytoplasmic elements begin to accumulate.[4]
Clinical Presentation[edit | edit source]
Presentations of nerve damage may include:
- Reduced or loss of function in associated structures to damaged nerves
- Gradual onset of numbness, prickling or tingling in feet or hands, which can spread upward into legs and arms
- Sharp, jabbing, throbbing, freezing, or burning pain
- Extreme sensitivity to touch
- Lack of coordination and falling
- Muscle weakness or paralysis if motor nerves are affected
- Neuromatous or causalgia pain
Diagnostic Procedures[edit | edit source]
- Electromyography
- Nerve conduction studies
- Sensation deficit and skin condition tests
- Muscle strength/loss
- Functional deficits
Outcome Measures[edit | edit source]
Depends on various criteria including pain and psychosocial skills but could include:
- Oxford scale
- Visual analogue scale
- Short form McGill pain questionnaire
(see Outcome Measures Database)
Management / Interventions[edit | edit source]
See Nerve Injury Rehabilitation
Wallerian Degeneration can instigate a nerve repair mechanism. Managing nerve damage can include the use of :Cryotherapy[7], Exercise, Neurorehabilitation, and Surgery.
References[edit | edit source]
- ↑ Conforti L, Gilley J, Coleman MP. Wallerian degeneration: an emerging axon death pathway linking injury and disease. Nature Reviews Neuroscience. 2014 Jun;15(6):394-409.
- ↑ Purves D, Augustine GJ, Fitzpatrick D, Hall WC, LaMantia AS, McNamara JO, White LE.Neuroscience (4 ed.). Sinauer Associates. 2008 pp. 11–20.
- ↑ Gaudet AD, Popovich PG &Ramer MS. Wallerian degeneration: Gaining perspective on inflammatory events after peripheral nerve injury.Journal of Neuroinflammation.2011 Available from.https://jneuroinflammation.biomedcentral.com/articles/10.1186/1742-2094-8-110 (accessed on 06/04/2021)
- ↑ Coleman MP, Conforti L, Buckmaster EA, Tarlton A, Ewing RM, Brown MC, Lyon MF, Perry VH (August 1998). "An 85-kb tandem triplication in the slow Wallerian degeneration (Wlds) mouse". Proceedings of the National Academy of Sciences of the United States of America. 95 (17): 9985–90. Bibcode:1998PNAS...95.9985C. doi:10.1073/pnas.95.17.9985. PMC 21448. PMID 9707587.
- ↑ Medical & Exercise Physiology School.Wallerian degeneration/ regeneration process of nerve fiber/axon cut and progressive response. Available from https://www.youtube.com/watch?v=kbzYML05Vac (last accessed 5 March 2021)
- ↑ The Young Orthopod. Nerve Regeneration. Available from https://www.https://www.youtube.com/watch?v=P02ea4jf50g&t=192s (last accessed 6 March 2021)
- ↑ Hsu M,and Stevenson FF.Wallerian Degeneration and Recovery of Motor Nerves after Multiple Focused Cold Therapies. US National Library of Medicine.National Institutes of Health.2015 ; 51(2): 268–275.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4315870/ (accessed on 6/04/2021)