Beta-Blockers: Difference between revisions
No edit summary |
(page link update) |
||
| (5 intermediate revisions by 2 users not shown) | |||
| Line 5: | Line 5: | ||
Beta-blockers are a broad class of medications that are used for various clinical benefits but also carry the potential for adverse effects<ref name=":1">Farzam K, Jan A. Beta blockers. StatPearls [Internet]. 2020 Jul 8.Available:https://www.ncbi.nlm.nih.gov/books/NBK532906/ (accessed 6.4.2021)</ref>. | Beta-blockers are a broad class of medications that are used for various clinical benefits but also carry the potential for adverse effects<ref name=":1">Farzam K, Jan A. Beta blockers. StatPearls [Internet]. 2020 Jul 8.Available:https://www.ncbi.nlm.nih.gov/books/NBK532906/ (accessed 6.4.2021)</ref>. | ||
Beta blockers uses range from lowering [[Blood Pressure|blood pressure]] to improving [[Heart Failure|heart failure]] (once a mainstay for treating high blood pressure, beta blockers have been elbowed aside by newer drugs, such as [[ACE Inhibitors | Beta blockers uses range from lowering [[Blood Pressure|blood pressure]] to improving [[Heart Failure|heart failure]] (once a mainstay for treating high blood pressure, beta blockers have been elbowed aside by newer drugs, such as [[ACE Inhibitors: Congestive Heart Failure|ACE inhibitors]], and older ones, such as thiazide [[diuretics]]). | ||
Beta receptors (tiny proteins) sit on the outer surface of many cells. There are three main types. | Beta receptors (tiny proteins) sit on the outer surface of many cells. There are three main types. | ||
# Beta-1 receptors are found almost exclusively in heart cells. | # Beta-1 receptors are found almost exclusively in heart cells. | ||
# Beta-2 receptors reside mostly in lung and blood vessel cells, though heart cells also have some. | # Beta-2 receptors reside mostly in [[Lung Anatomy|lung]] and [[Blood Physiology|blood vessel]] cells, though heart cells also have some. | ||
# Beta-3 receptors are located on fat cells.<ref name=":2">Harvard Edu. [https://www.health.harvard.edu/heart-health/beta-blockers-cardiac-jacks-of-all-trades Beta Blockers: Jack of all trades] Available from: https://www.health.harvard.edu/heart-health/beta-blockers-cardiac-jacks-of-all-trades<nowiki/>(accessed 4.6.2021)</ref> | # Beta-3 receptors are located on fat cells.<ref name=":2">Harvard Edu. [https://www.health.harvard.edu/heart-health/beta-blockers-cardiac-jacks-of-all-trades Beta Blockers: Jack of all trades] Available from: https://www.health.harvard.edu/heart-health/beta-blockers-cardiac-jacks-of-all-trades<nowiki/>(accessed 4.6.2021)</ref> | ||
Beta receptors latch onto chemical messengers released by the nervous system and initiate sympathetic activation eg the heart beats faster, blood vessels constrict, the airways relax, and the kidneys increase production of a protein that boosts blood pressure. | Beta receptors latch onto [[Cytokines|chemical messengers]] released by the nervous system and initiate [[Vagus Nerve|sympathetic activation]] eg the heart beats faster, blood vessels constrict, the airways relax, and the [[Kidney|kidneys]] increase production of a protein that boosts blood pressure. Beta blockers subvert these processes by settling onto beta receptors and preventing the chemical messengers from binding to their receptors eg slows the heart, improves the conduction of electrical signals in the heart, relaxes blood vessels, and lowers blood pressure<ref name=":2" />. | ||
Beta blockers subvert these processes by settling onto beta receptors and preventing the chemical messengers from binding to their receptors eg slows the heart, improves the conduction of electrical signals in the heart, relaxes blood vessels, and lowers blood pressure<ref name=":2" />. | |||
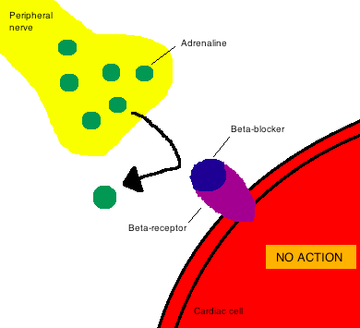
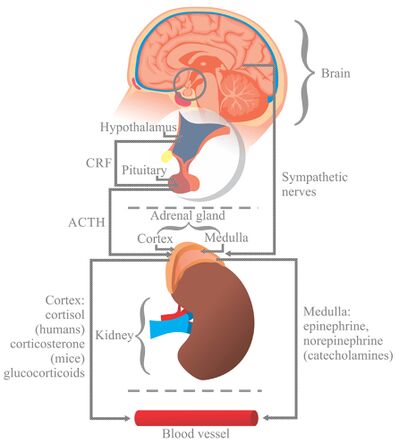
Image 1: Beta-blockers cause a competitive inhibition of the β-receptor, which counters the effects of catecholamines. Catecholamines are hormones made by your adrenal glands eg adrenalin. The adrenal glands send catecholamines into the blood when a person is physically or emotionally stressed<ref>Web med Catecholamines Available:https://www.webmd.com/heart-disease/catecholamines-test-facts (accessed 6.4.2021)</ref>. | Image 1: Beta-blockers cause a competitive inhibition of the β-receptor, which counters the effects of catecholamines. Catecholamines are hormones made by your adrenal glands eg adrenalin. The adrenal glands send catecholamines into the blood when a person is physically or emotionally stressed<ref>Web med Catecholamines Available:https://www.webmd.com/heart-disease/catecholamines-test-facts (accessed 6.4.2021)</ref>. | ||
== Function == | == Function == | ||
[[File:Beta blockers table.png|right|frameless|413x413px]] | |||
Beta-blockers, as a class of medications, are essential drugs and are first-line treatments in many acute and chronic conditions.<ref name=":1" /> There are two types of beta receptors in the body drugs are target: | Beta-blockers, as a class of medications, are essential drugs and are first-line treatments in many acute and chronic conditions.<ref name=":1" /> There are two types of beta receptors in the body drugs are target: | ||
| Line 32: | Line 31: | ||
== Uses == | == Uses == | ||
Glaucoma: Ophthalmic solutions are used to decrease eye pressures, though the mechanisms are not fully understood<ref name=":3">Straight a nursing Beta blockers Available:https://www.straightanursingstudent.com/beta-blockers/ (accessed 4.6.2021)</ref>. | * [[File:Heart Attack.png|right|frameless]][[Hypertension]]: Beta blockers are commonly prescribed to treat hypertension. | ||
* [[Angina]]: Decreasing the rate lowers myocardial oxygen demand. Decreasing blood pressure leads to a decrease in afterload, which decreases the workload of the heart, which also lowers myocardial oxygen demand. | |||
* [[Heart Arrhythmias: Assessment|Dysrhythmias]]: Beta blockers are often used to control the rate in [[Atrial Fibrillation|atrial fibrillation]]. | |||
* [[Myocardial Infarction|Myocardial infarction]]: When given within 24-hours of onset, beta blockers reduce cardiac workload and improve likelihood of survival. | |||
* [[Heart Failure|Heart failure]]: Beta blockers are used in coordination with other medications to slow the progression of heart failure. Metoprolol and carvedilol are the main ones used to slow the heart rate (giving the heart time to “rest” between beats) and lower blood pressure, which decreases afterload and, therefore, the workload of the heart. | |||
* [[Migraine Headache|Migraines]]: Some beta blockers (such as atenolol, metoprolol, timolol and propranolol) are used to help prevent migraines by inhibiting arterial dilation in the brain. | |||
* Glaucoma: Ophthalmic solutions are used to decrease eye pressures, though the mechanisms are not fully understood<ref name=":3">Straight a nursing Beta blockers Available:https://www.straightanursingstudent.com/beta-blockers/ (accessed 4.6.2021)</ref>. | |||
== Beta Blockers And CHF == | == Beta Blockers And CHF == | ||
[[File:Depiction of a person suffering from heart failure.png|right|frameless|399x399px]] | [[File:Depiction of a person suffering from heart failure.png|right|frameless|399x399px]] | ||
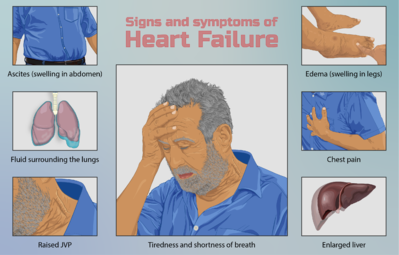
Beta blockers are considered the primary drugs for the pharmacological management of [[Heart Failure|CHF]]. These drugs provide their beneficial effect by decreasing the excessive activity of the sympathetic nervous system which is characteristic of CHF. | Beta blockers are considered the primary drugs for the pharmacological management of [[Heart Failure|CHF]]. These drugs provide their beneficial effect by decreasing the excessive activity of the [[Sympathetic Nervous System|sympathetic nervous system]] which is characteristic of CHF. Clinically useful beta-1 cardioselective blockers bind to beta-adrenergic receptors on the myocardium, blocking the effects of norepinephrine and epinephrine. By this mechanism, beta blockers normalize sympathetic activity reducing heart rate, cardiac contraction force, and angina. | ||
Sympathetic activation leading to raised levels of catecholamines is one of the earliest responses to the fall in cardiac output that occurs in chronic heart failure (CHF). Raised catecholamine levels have numerous adverse effects that can be counteracted by beta-blockers. eg. The increased heart rate associated with sympathetic activation is associated with a poor prognosis in CHF. Beta-blockers also reduce remodelling in CHF, increase LV ejection fraction, reduce end-systolic volume, and improve ventricular filling time. They are also believed to have a direct anti- arrhythmic action that protects against sudden cardiac death and to have additional effects at the cellular level on myocyte hypertrophy and [[apoptosis]].<ref>Silke B. Beta-blockade in CHF: pathophysiological considerations. European Heart Journal Supplements. 2006 Jun 1;8(suppl_C):C13-8.Available from: (accessed 6.4.2021)</ref> | * [[Vagus Nerve|Sympathetic activation]] leading to raised levels of catecholamines is one of the earliest responses to the fall in cardiac output that occurs in chronic heart failure (CHF). Raised catecholamine levels have numerous adverse effects that can be counteracted by beta-blockers. eg. The increased [[Pulse rate|heart rate]] associated with sympathetic activation is associated with a poor prognosis in CHF. | ||
* Beta-blockers also reduce remodelling in CHF, increase LV ejection fraction, reduce end-systolic volume, and improve ventricular filling time. They are also believed to have a direct anti- arrhythmic action that protects against [[Acute Coronary Syndrome|sudden cardiac death]] and to have additional effects at the cellular level on [[Muscle Cells (Myocyte)|myocyte]] hypertrophy and [[apoptosis]].<ref>Silke B. Beta-blockade in CHF: pathophysiological considerations. European Heart Journal Supplements. 2006 Jun 1;8(suppl_C):C13-8.Available from: https://watermark.silverchair.com/sul009.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAArswggK3BgkqhkiG9w0BBwagggKoMIICpAIBADCCAp0GCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQM9x7woDrYehfbXSx7AgEQgIICbiBy_6CQRWdHpR4Zb_mJiYYmjgCeeB3HJ0LHaunl3Gmz59-WHSSAltoOEWElt1Nbo52pxXM_C1cuwbJdKdyS5hbziuIvGP84hLU-b4VaH6Xek0FVcCZcEUL_rYf5-4TaLbFtUZ8Wh4LgUwOCIlGJFBdxiEyvAiLdrC385iAwYn1EFhPzgJ-EsDt3OWo_hlPUqcRIjxK6xSMJS2TQEhtSqcHjRODJdVDijupSyvfNo5Lz5hkt6EvLRqgMaiCyHxegCjdqIkjH-YlKbiKqRpYTF2aHqUC6Ou6k9RrQr1sOBwWgU6suI4seEDp9zPZc7DqhpoILslrCwjRTwHvgqobkcaGgF7fikrMJf0gkcfrNi2z9HFRk-_r_crjJ37X_gn2AXgJzh7UYjwR43OyiLVK25-ML3QIU4nBl7xdQ27R7izZj7rg7RJPN0grrsoJ7pObg9KrI8tGiu97ykjca1LZdveQn8QtNBuRqvTlNN3geENNYUX5rOlbner5X7VebOOqX1jYkMMbkrNFmgKsGJsSe4sEtUaipZ6aDXKVdaaQ45Kgwv6aE83kLp8hfLK30k937qNWGIxHJNRU8Tqi_9mvi2eyppQws0WFoW5oUuOvn8TN7fRUOTJ8yOUEYolwYnqkK5VU8WJarlmJCQu8KIcQPfqygl-7kNdVZ7X4pzEqOvVTjwxJb54ndkDyK87UA3wULXiMMdhBk44qqcbPxuMUKAOHoYQ_13PpL6i6dDMcO5wEbPzTdzgK9a3L3q5OTLO96mUEn5S24CxPeZELjVx3-tV_xGYb0_3BqnQOPWJHyR5iFuBVfpKrWkVCstGqN55o<nowiki/>(accessed 6.4.2021)</ref> | |||
== Side effects == | |||
Beta receptors are found all over the body and induce a broad range of physiologic effects. The blockade of these receptors with beta-blocker medications can lead to many adverse effects. | |||
* [[Bradycardia]] and [[hypotension]] are two adverse effects that may commonly occur. | |||
* Fatigue, dizziness, nausea, and constipation are also widely reported. | |||
* Some patients report [[Sexual Dysfunction After Prostate Cancer|sexual]] dysfunction and erectile dysfunction. | |||
* Less commonly, bronchospasm presents in patients on beta-blockers. [[Asthma|Asthmatic]] patients are at a higher risk. Patients with [[Raynaud's Phenomenon|Raynaud syndrome]] are also at risk of exacerbation<ref name=":1" />. | |||
== Physiotherapy implications == | |||
While beta blockers may allow patients to participate in therapy less inhibited by angina and with reduced stress on the heart, [[Cardiopulmonary Exercise Testing (CPET) In Adults|exercise programs]] must be prescribed with extreme caution and monitored carefully. | |||
*[[File:Fatigued.jpeg|right|frameless]]Beta blockers may render conventional [[Aerobic Exercise|aerobic]] workload guidelines inappropriate as they typically decrease maximal heart rate, and consequently have the potential to mislead the therapist prescribing an [[Cardiac Rehabilitation|exercise program]]. | |||
* Beta blockers block conduction at the AV Node, decrease heart rate and lower blood pressure. Watch your patient for bradycardia and hypotension<ref name=":3" /> | |||
* Heart rate and blood pressure should be monitored frequently, and the patient should be assessed for signs of fatigue, dizziness, and weakness prior to the initiation of the therapy session and monitored throughout. | |||
== | == Video == | ||
The 4 minute presentation below outlines the role of beta Blockers in CHF{{#ev:youtube|https://www.youtube.com/watch?v=jpvB5aVF5Nk&t=124s|width}}<ref>mmlearn.org Living with Heart Failure - Beta Blockers Available from: https://www.youtube.com/watch?v=jpvB5aVF5Nk&t=124s (last accessed 17.6.2019)</ref> | |||
== Delve deeper into the Stress Response == | |||
[[File:Response to stress.jpeg|right|frameless|442x442px]] | |||
'''Image 5: Stress Response''' | |||
Whether the [[Stress and Health|stress]] is physical or emotional, the response is the same. The [[Kidney|adrenal cortex]] increases secretion of the [[Hormones|hormone]] Cortisol, and the activity of the [[Sympathetic Nervous System|sympathetic nervous system]] is increased, resulting in increased epinephrine/adrenaline secretion from the adrenal medulla. Other hormones are also released during stress, and [[Insulin in the Treatment of Diabetes Mellitus|insulin]] production is usually decreased. | |||
The response of the sympathetic nervous system is commonly called the "fight-or-flight" response because the physical affects allow us to physically fight or flee<ref>IHS Stress response Available : https://www.innerhealthstudio.com/definition-of-stress.html<nowiki/>(accessed 5.6.2021)</ref>. | |||
* | |||
== Resources == | == Resources == | ||
Latest revision as of 06:48, 8 February 2023
Introduction[edit | edit source]
Beta-blockers are a broad class of medications that are used for various clinical benefits but also carry the potential for adverse effects[1].
Beta blockers uses range from lowering blood pressure to improving heart failure (once a mainstay for treating high blood pressure, beta blockers have been elbowed aside by newer drugs, such as ACE inhibitors, and older ones, such as thiazide diuretics).
Beta receptors (tiny proteins) sit on the outer surface of many cells. There are three main types.
- Beta-1 receptors are found almost exclusively in heart cells.
- Beta-2 receptors reside mostly in lung and blood vessel cells, though heart cells also have some.
- Beta-3 receptors are located on fat cells.[2]
Beta receptors latch onto chemical messengers released by the nervous system and initiate sympathetic activation eg the heart beats faster, blood vessels constrict, the airways relax, and the kidneys increase production of a protein that boosts blood pressure. Beta blockers subvert these processes by settling onto beta receptors and preventing the chemical messengers from binding to their receptors eg slows the heart, improves the conduction of electrical signals in the heart, relaxes blood vessels, and lowers blood pressure[2].
Image 1: Beta-blockers cause a competitive inhibition of the β-receptor, which counters the effects of catecholamines. Catecholamines are hormones made by your adrenal glands eg adrenalin. The adrenal glands send catecholamines into the blood when a person is physically or emotionally stressed[3].
Function[edit | edit source]
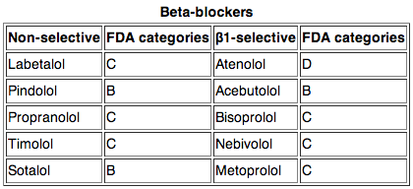
Beta-blockers, as a class of medications, are essential drugs and are first-line treatments in many acute and chronic conditions.[1] There are two types of beta receptors in the body drugs are target:
- Beta-1 receptors, which are present in the heart
- Beta-2 receptors, which are present in vascular smooth muscle and the muscle lining the airways.
More than a dozen beta blockers have been approved for use in the United States (see table). They fall into three main groups.
- Nonselective. These are first-generation beta blockers. They will block some of both beta 1 and beta 2 receptors. They can slow not only cardiac output, but also the renal and other systems. You may lower blood pressure but risk kidney or breathing problems[4].
- Cardioselective. A number of beta blockers are designed to block only beta-1 receptors in heart cells. Since they don't affect beta-2 receptors in blood vessels and the lungs, cardioselective beta blockers are safer for people with lung disorders.
- Third-generation. Some beta blockers do more than block beta receptors. eg. Labetalol blocks alpha receptors, too. This further helps relax blood vessels. Nebivolol stimulates the inner lining of blood vessels (the endothelium) to generate nitric oxide, which helps the vessels relax. Carvedilol does both[2].
Uses[edit | edit source]
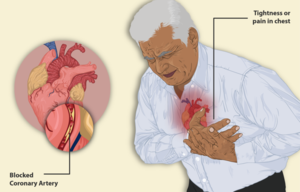
- Hypertension: Beta blockers are commonly prescribed to treat hypertension.
- Angina: Decreasing the rate lowers myocardial oxygen demand. Decreasing blood pressure leads to a decrease in afterload, which decreases the workload of the heart, which also lowers myocardial oxygen demand.
- Dysrhythmias: Beta blockers are often used to control the rate in atrial fibrillation.
- Myocardial infarction: When given within 24-hours of onset, beta blockers reduce cardiac workload and improve likelihood of survival.
- Heart failure: Beta blockers are used in coordination with other medications to slow the progression of heart failure. Metoprolol and carvedilol are the main ones used to slow the heart rate (giving the heart time to “rest” between beats) and lower blood pressure, which decreases afterload and, therefore, the workload of the heart.
- Migraines: Some beta blockers (such as atenolol, metoprolol, timolol and propranolol) are used to help prevent migraines by inhibiting arterial dilation in the brain.
- Glaucoma: Ophthalmic solutions are used to decrease eye pressures, though the mechanisms are not fully understood[5].
Beta Blockers And CHF[edit | edit source]
Beta blockers are considered the primary drugs for the pharmacological management of CHF. These drugs provide their beneficial effect by decreasing the excessive activity of the sympathetic nervous system which is characteristic of CHF. Clinically useful beta-1 cardioselective blockers bind to beta-adrenergic receptors on the myocardium, blocking the effects of norepinephrine and epinephrine. By this mechanism, beta blockers normalize sympathetic activity reducing heart rate, cardiac contraction force, and angina.
- Sympathetic activation leading to raised levels of catecholamines is one of the earliest responses to the fall in cardiac output that occurs in chronic heart failure (CHF). Raised catecholamine levels have numerous adverse effects that can be counteracted by beta-blockers. eg. The increased heart rate associated with sympathetic activation is associated with a poor prognosis in CHF.
- Beta-blockers also reduce remodelling in CHF, increase LV ejection fraction, reduce end-systolic volume, and improve ventricular filling time. They are also believed to have a direct anti- arrhythmic action that protects against sudden cardiac death and to have additional effects at the cellular level on myocyte hypertrophy and apoptosis.[6]
Side effects[edit | edit source]
Beta receptors are found all over the body and induce a broad range of physiologic effects. The blockade of these receptors with beta-blocker medications can lead to many adverse effects.
- Bradycardia and hypotension are two adverse effects that may commonly occur.
- Fatigue, dizziness, nausea, and constipation are also widely reported.
- Some patients report sexual dysfunction and erectile dysfunction.
- Less commonly, bronchospasm presents in patients on beta-blockers. Asthmatic patients are at a higher risk. Patients with Raynaud syndrome are also at risk of exacerbation[1].
Physiotherapy implications [edit | edit source]
While beta blockers may allow patients to participate in therapy less inhibited by angina and with reduced stress on the heart, exercise programs must be prescribed with extreme caution and monitored carefully.
- Beta blockers may render conventional aerobic workload guidelines inappropriate as they typically decrease maximal heart rate, and consequently have the potential to mislead the therapist prescribing an exercise program.
- Beta blockers block conduction at the AV Node, decrease heart rate and lower blood pressure. Watch your patient for bradycardia and hypotension[5]
- Heart rate and blood pressure should be monitored frequently, and the patient should be assessed for signs of fatigue, dizziness, and weakness prior to the initiation of the therapy session and monitored throughout.
Video[edit | edit source]
The 4 minute presentation below outlines the role of beta Blockers in CHF
Delve deeper into the Stress Response[edit | edit source]
Image 5: Stress Response
Whether the stress is physical or emotional, the response is the same. The adrenal cortex increases secretion of the hormone Cortisol, and the activity of the sympathetic nervous system is increased, resulting in increased epinephrine/adrenaline secretion from the adrenal medulla. Other hormones are also released during stress, and insulin production is usually decreased.
The response of the sympathetic nervous system is commonly called the "fight-or-flight" response because the physical affects allow us to physically fight or flee[8].
Resources[edit | edit source]
- ↑ 1.0 1.1 1.2 Farzam K, Jan A. Beta blockers. StatPearls [Internet]. 2020 Jul 8.Available:https://www.ncbi.nlm.nih.gov/books/NBK532906/ (accessed 6.4.2021)
- ↑ 2.0 2.1 2.2 Harvard Edu. Beta Blockers: Jack of all trades Available from: https://www.health.harvard.edu/heart-health/beta-blockers-cardiac-jacks-of-all-trades(accessed 4.6.2021)
- ↑ Web med Catecholamines Available:https://www.webmd.com/heart-disease/catecholamines-test-facts (accessed 6.4.2021)
- ↑ Health FAQ beta 1 vs Beta 2 Available from:https://health-faq.com/heart-disease/beta-1-blockers-vs-beta-2-blockers/ (accessed 6.4.2021)
- ↑ 5.0 5.1 Straight a nursing Beta blockers Available:https://www.straightanursingstudent.com/beta-blockers/ (accessed 4.6.2021)
- ↑ Silke B. Beta-blockade in CHF: pathophysiological considerations. European Heart Journal Supplements. 2006 Jun 1;8(suppl_C):C13-8.Available from: https://watermark.silverchair.com/sul009.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAArswggK3BgkqhkiG9w0BBwagggKoMIICpAIBADCCAp0GCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQM9x7woDrYehfbXSx7AgEQgIICbiBy_6CQRWdHpR4Zb_mJiYYmjgCeeB3HJ0LHaunl3Gmz59-WHSSAltoOEWElt1Nbo52pxXM_C1cuwbJdKdyS5hbziuIvGP84hLU-b4VaH6Xek0FVcCZcEUL_rYf5-4TaLbFtUZ8Wh4LgUwOCIlGJFBdxiEyvAiLdrC385iAwYn1EFhPzgJ-EsDt3OWo_hlPUqcRIjxK6xSMJS2TQEhtSqcHjRODJdVDijupSyvfNo5Lz5hkt6EvLRqgMaiCyHxegCjdqIkjH-YlKbiKqRpYTF2aHqUC6Ou6k9RrQr1sOBwWgU6suI4seEDp9zPZc7DqhpoILslrCwjRTwHvgqobkcaGgF7fikrMJf0gkcfrNi2z9HFRk-_r_crjJ37X_gn2AXgJzh7UYjwR43OyiLVK25-ML3QIU4nBl7xdQ27R7izZj7rg7RJPN0grrsoJ7pObg9KrI8tGiu97ykjca1LZdveQn8QtNBuRqvTlNN3geENNYUX5rOlbner5X7VebOOqX1jYkMMbkrNFmgKsGJsSe4sEtUaipZ6aDXKVdaaQ45Kgwv6aE83kLp8hfLK30k937qNWGIxHJNRU8Tqi_9mvi2eyppQws0WFoW5oUuOvn8TN7fRUOTJ8yOUEYolwYnqkK5VU8WJarlmJCQu8KIcQPfqygl-7kNdVZ7X4pzEqOvVTjwxJb54ndkDyK87UA3wULXiMMdhBk44qqcbPxuMUKAOHoYQ_13PpL6i6dDMcO5wEbPzTdzgK9a3L3q5OTLO96mUEn5S24CxPeZELjVx3-tV_xGYb0_3BqnQOPWJHyR5iFuBVfpKrWkVCstGqN55o(accessed 6.4.2021)
- ↑ mmlearn.org Living with Heart Failure - Beta Blockers Available from: https://www.youtube.com/watch?v=jpvB5aVF5Nk&t=124s (last accessed 17.6.2019)
- ↑ IHS Stress response Available : https://www.innerhealthstudio.com/definition-of-stress.html(accessed 5.6.2021)