Hyperkalemia: Difference between revisions
No edit summary |
(page link update) |
||
| (36 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''-Courtney Ahlers & Jessica Ketterer [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | '''Original Editors '''-Courtney Ahlers & Jessica Ketterer [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
[[File:Membrane potential ions (id).jpg|right|frameless]] | |||
Potassium is an important nutrient and [[Electrolytes|electrolyte]], it helps muscles work, including those [[Muscles of Respiration|involved in breathing]] and keeping the [[Anatomy of the Human Heart|heart]] beating. But too much potassium in our system, known as hyperkalemia, can cause serious health problems. And people with [[Chronic Kidney Disease|kidney disease]] are more prone to developing hyperkalemia.<ref>Healthline [https://www.healthline.com/health/high-potassium/hyperkalemia-facts 5 Things to Know About Hyperkalemia for National Kidney Month] Available: https://www.healthline.com/health/high-potassium/hyperkalemia-facts<nowiki/>(accessed 18.9.2021)</ref> | |||
Hyperkalemia is | Hyperkalemia is defined as a serum or plasma potassium level above the upper limits of normal, usually greater than 5.0 mEq/L to 5.5 mEq/L. While mild hyperkalemia is usually asymptomatic, high levels of potassium may cause life-threatening [[Heart Arrhythmias: Assessment|cardiac arrhythmias]], muscle weakness or paralysis. Symptoms usually develop at levels higher levels, 6.5 mEq/L to 7 mEq/<ref name=":0">Simon LV, Hashmi MF, Farrell MW. [https://www.ncbi.nlm.nih.gov/books/NBK470284/ Hyperkalemia]. StatPearls [Internet]. 2020 Dec 1.Available:https://www.ncbi.nlm.nih.gov/books/NBK470284/ (accessed 18.9.2021)</ref> | ||
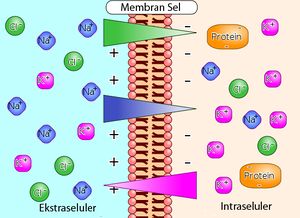
Image 1: Illustration of the way that differences in ion concentration on opposite sides of a cell membrane produce a voltage difference. Potassium is usually an intracellular cation. | |||
For patients with mild transient hyperkalemia, the prognosis is excellent if the inciting cause is addressed and treated. Sudden onset, extreme hyperkalemia can cause cardiac arrhythmias that can be lethal in up to two-thirds of cases if not rapidly treated. Hyperkalemia is an independent risk factor for death in hospitalized patients.<ref name=":0" /> | |||
The | == Etiology == | ||
Often a report of high blood potassium isn't true hyperkalemia. Instead, it may be caused by the rupture of [[Blood Physiology|blood cells]] in the blood sample during or shortly after the blood draw. The ruptured cells leak their potassium into the sample. This falsely raises the amount of potassium in the [[Blood Tests|blood sample]], even though the potassium level in your body is actually normal. When this is suspected, a repeat blood sample is done. | |||
[[File:Dialysis.jpg|right|frameless]] | |||
The most common cause of genuinely hyperkalemia is related to the kidneys, eg: | |||
< | * Acute kidney failure | ||
* [[Chronic Kidney Disease|Chronic kidney disease]] | |||
Other causes of hyperkalemia include: | |||
* [[Addison's Disease|Addison's disease]] (adrenal insufficiency) | |||
* Angiotensin II receptor blockers | |||
* Angiotensin-converting enzyme ([[ACE Inhibitors: Congestive Heart Failure|ACE]]) inhibitors | |||
* [[Beta-Blockers|Beta blockers]] | |||
* [[Dehydration]] | |||
* Destruction of red blood cells due to severe injury or [[Burns Overview|burns]] | |||
* Excessive use of potassium supplements | |||
* [[Diabetes Mellitus Type 1|Type 1 diabetes]]<ref>Mayo clinic [https://www.mayoclinic.org/symptoms/hyperkalemia/basics/causes/sym-20050776 Hyperkalemia] Available: https://www.mayoclinic.org/symptoms/hyperkalemia/basics/causes/sym-20050776 (accessed 18.9.2021)</ref> | |||
Image 2: Dialysis for Chronic Kidney Disease. | |||
== Epidemiology == | |||
Hyperkalemia is unusual in the general population, reported in less than 5% of the population, worldwide. | |||
* Affects up to 10% of all hospitalized patients, most cases in hospitalized patients are due to medications and renal insufficiency. | |||
* Diabetes, malignancy, extremes of age, and acidosis are other important causes in inpatients. | |||
* Hyperkalemia is rare in children but may occur in up to 50% of premature infants. | |||
* Hyperkalemia is more commonly reported in men than women perhaps due to increased muscle mass and higher rates of [[rhabdomyolysis]] and increased prevalence of [[Neuromuscular Disorders|neuromuscular disease]]. | |||
Today there is a risk that empirical use of ACE inhibitors may cause hyperkalemia, which can be of concern in high risk populations eg diabetics, those with heart failure, and peripheral vascular disease<ref name=":0" />. | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
[[File:Ecg_thing.gif|alt=|right|frameless|524x524px]]Hyperkalemia most commonly occurs in patients with [[Chronic Kidney Disease|chronic renal failure]] and is also correlated with [[diabetes]]. <ref name="Hollander-Rodriguez and Calvert">Hollander-Rodriguez JC, Calvert, Jr. JF. Hyperkalemia. American Family Physician 2006; 73(2):283-290. Available from: PubMed. http://www.ncbi.nlm.nih.gov/pubmed/16445274 )22 March 2013)</ref> <ref name="Spiro">Tamirisa KP, Aaronson KD, Koelling TM. Spironolactone-induced renal insufficiency and hyperkalemia in patients with heart failure, American Heart J 2004; 148(6):971-978. Available from: Europe Pubmed Central. http://www.sciencedirect.com/science/article/pii/S0002870304007501 (Accessed 4 April 2013)</ref> | |||
Image 3: [[Electrocardiogram|ECG]] is monitored in patients with hyperkalemia: | |||
Signs and Symptoms | Signs and Symptoms | ||
| Line 33: | Line 60: | ||
#palpitations | #palpitations | ||
Potassium is regulated through excretion via the renal system. When this system's function declines, the extracellular potassium concentration increases and can lead to membrane excitability. Some signs and symptoms listed above are a result of the impaired nerve conduction and muscle contraction dysfunction. Muscular dysfunction includes the cardiac system and can lead to life threatening ventricular arrhythmias. Electrocardiogram (ECG) dysfunction is more common in patients with acute hyperkalemia.<ref name="Raymond et al." | Potassium is regulated through excretion via the renal system. When this system's function declines, the extracellular potassium concentration increases and can lead to membrane excitability. Some signs and symptoms listed above are a result of the impaired nerve conduction and muscle contraction dysfunction. Muscular dysfunction includes the cardiac system and can lead to life threatening ventricular arrhythmias. Electrocardiogram ([[Electrocardiogram|ECG]]) dysfunction is more common in patients with acute hyperkalemia.<ref name="Raymond et al.">Raymond C, Sood A, Wazny L. Treatment of hyperkalemia in patients with chronic kidney disease--a focus on medications. CANNT Journal [serial on the Internet]. (2010, July), [cited March 22, 2013]; 20(3): 49-54. Available from: CINAHL with Full Text. http://search.ebscohost.com/login.aspx?direct=true&db=c8h&AN=2010782358&site=ehost-live (accessed 22 Mar 2013)</ref> | ||
- | |||
== Diagnostic Tests/Lab Tests/Lab Values == | == Diagnostic Tests/Lab Tests/Lab Values == | ||
| Line 145: | Line 66: | ||
Initial diagnosis is initiated with patient history, medication review, and physical examination. | Initial diagnosis is initiated with patient history, medication review, and physical examination. | ||
Laboratory tests include: | [[Blood Tests|Laboratory tests]] include: | ||
#serum electrolytes (especially potassium and glucose <ref name="Raymond et al." />) | #serum electrolytes (especially potassium and glucose <ref name="Raymond et al." />) | ||
| Line 154: | Line 75: | ||
#trial of oral fludrocortisone (Florinef)<ref name="Hollander-Rodriguez and Calvert" /> | #trial of oral fludrocortisone (Florinef)<ref name="Hollander-Rodriguez and Calvert" /> | ||
Patients will likely not present with symptoms of hyperkalemia until potassium levels have exceeded 7 mmol/L. | Patients will likely not present with symptoms of hyperkalemia until potassium levels have exceeded 7 mmol/L. However, immediate medical attention is required when potassium level exceed 6.5 mmol/L or exceed 6.0 mmol/L with ECG changes consistent with hyperkalemia.<ref name="Raymond et al." /> | ||
== Systemic Involvement == | == Systemic Involvement == | ||
| Line 271: | Line 104: | ||
|} | |} | ||
== | == Treatment == | ||
The urgency with which hyperkalemia should be managed depends on how rapidly the condition developed, the absolute serum potassium level, the degree of symptoms, and the cause.<ref name=":0" /> | |||
The presence of ECG changes, a rapid rise of serum potassium, indications of decreased kidney function, or significant acidosis require immediate medical treatment for hyperkalemia. Although ECG changes are common indicators for severe hyperkalemia, the patient may still have life threatening hyperkalemia even if ECG readings are normal. The intent of immediate medical intervention is to stabilize the myocardium to prevent arrhythmias. In addition to the medications listed in Table 5, total body potassium levels can be lowered through kidney excretion, gastrointestinal (GI) elimination, or dialysis. Lowering via kidney excretion is achieved by the use of diuretics, while lowering via GI elimination occurs with the use of Kayexalate | * The presence of ECG changes, a rapid rise of serum potassium, indications of decreased kidney function, or significant acidosis require immediate medical treatment for hyperkalemia. | ||
* Although ECG changes are common indicators for severe hyperkalemia, the patient may still have life threatening hyperkalemia even if ECG readings are normal. | |||
* The intent of immediate medical intervention is to stabilize the myocardium to prevent arrhythmias. | |||
In addition to the medications listed in Table 5, total body potassium levels can be lowered through kidney excretion, gastrointestinal (GI) elimination, or dialysis. Lowering via kidney excretion is achieved by the use of [[diuretics]], while lowering via GI elimination occurs with the use of Kayexalate. Long term management is focused on addressing the underlying cause, which can be achieved by discontinuing medications or consuming low potassium diets.<ref name="Hollander-Rodriguez and Calvert" /> | |||
[[Image:Afp20060115p283-f2.gif]] | [[Image:Afp20060115p283-f2.gif]] | ||
| Line 279: | Line 117: | ||
Figure 2: Algorithm for the management of hyperkalemia.<ref name="Hollander-Rodriguez and Calvert" /> | Figure 2: Algorithm for the management of hyperkalemia.<ref name="Hollander-Rodriguez and Calvert" /> | ||
Foods high in potassium can also be implicated in the development of hyperkalemia. | |||
{| style="width: 698px; height: 326px" border="1" cellspacing="1" cellpadding="1" width="698" | |||
|- | |||
| | |||
Table 2. High-potassium foods<ref name="Raymond et al." /> | |||
(National Kidney foundation, 2010) | |||
|- | |||
| | |||
- salt substitutes and salt free broth | |||
- yogurt, milk | |||
- molasses | |||
- seaweed | |||
- chocolate | |||
- bran cereal, wheat germ, granola | |||
- vegetables (acorn squash, artichoke, bamboo shoots, beets, broccoli, brussel sprouts, chinese cabbage, carrots, greens (except kale), kohlrabi, mushrooms (canned), parsnips, potatoes, pumpkin, rutabagas, spinach, tomatoes, vegetable juices) | |||
- dried fruit (apricot, dates, figs, raisins, prunes) | |||
- nuts and seeds, (peanut butter) | |||
- dried peas and beans (lima beans, black beans, refried beans, lentils, legumes) | |||
- fruit and juice (apricot, avocado, banana, cantaloupe, grapefruit, honeydew, kiwi fruit, mango, nectarine, orange, papaya, pomegranate, prune) | |||
<br> | |||
|} | |||
== | == Physical Therapy Management == | ||
Hyperkalemia is a disorder that is not managed primarily by a physical therapist, however physical therapists should be aware of signs and symptoms of this disorder and should refer the patient to a medical doctor when indicated. | |||
* Potassium levels < 3.2 mEq/L or > 5.1 mEq/L are contraindicated for physical therapy intervention due to the potential for arrhythmia and tetany. | |||
* When potassium levels are not within the normal range (3.5-5.0 mEq/L) exercise is not effective due to decreased muscle pH and action potentials as well as inhibition of motor neurons. | |||
* With a patient who has marginal potassium levels, [[Vital Signs|vital signs]] (including pulse rhythm) and any signs of dizziness, muscle weakness or cramping, numbness or tingling, and changes in balance should be closely monitored. | |||
< | At this time, no research addresses the change in potassium level that occurs with exercise. However, it is known that patients with hyperkalemia are at risk for ventricular arrhythmias which can result in reduced exercise tolerance.<ref name="Goodman">Goodman CC & Fuller KS. In K Falk editor. Pathology: Implications for the Physical Therapist. St. Louis: Saunders Elsevier; 2009. pp.150, 157, 187-189, 480, 558, 927, 1243, 1640-1641</ref> | ||
== References == | |||
== References | |||
see [[Adding References|adding references tutorial]]. | see [[Adding References|adding references tutorial]]. | ||
| Line 327: | Line 168: | ||
<references /> | <references /> | ||
[[Category: | [[Category:Bellarmine Student Project]] | ||
[[Category:Conditions]] | |||
Latest revision as of 06:42, 8 February 2023
Original Editors -Courtney Ahlers & Jessica Ketterer from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Jessica Ketterer, Lucinda hampton, Elaine Lonnemann, Admin, Kim Jackson, WikiSysop, 127.0.0.1, Wendy Walker and Aminat Abolade
Definition/Description[edit | edit source]
Potassium is an important nutrient and electrolyte, it helps muscles work, including those involved in breathing and keeping the heart beating. But too much potassium in our system, known as hyperkalemia, can cause serious health problems. And people with kidney disease are more prone to developing hyperkalemia.[1]
Hyperkalemia is defined as a serum or plasma potassium level above the upper limits of normal, usually greater than 5.0 mEq/L to 5.5 mEq/L. While mild hyperkalemia is usually asymptomatic, high levels of potassium may cause life-threatening cardiac arrhythmias, muscle weakness or paralysis. Symptoms usually develop at levels higher levels, 6.5 mEq/L to 7 mEq/[2]
Image 1: Illustration of the way that differences in ion concentration on opposite sides of a cell membrane produce a voltage difference. Potassium is usually an intracellular cation.
For patients with mild transient hyperkalemia, the prognosis is excellent if the inciting cause is addressed and treated. Sudden onset, extreme hyperkalemia can cause cardiac arrhythmias that can be lethal in up to two-thirds of cases if not rapidly treated. Hyperkalemia is an independent risk factor for death in hospitalized patients.[2]
Etiology[edit | edit source]
Often a report of high blood potassium isn't true hyperkalemia. Instead, it may be caused by the rupture of blood cells in the blood sample during or shortly after the blood draw. The ruptured cells leak their potassium into the sample. This falsely raises the amount of potassium in the blood sample, even though the potassium level in your body is actually normal. When this is suspected, a repeat blood sample is done.
The most common cause of genuinely hyperkalemia is related to the kidneys, eg:
- Acute kidney failure
- Chronic kidney disease
Other causes of hyperkalemia include:
- Addison's disease (adrenal insufficiency)
- Angiotensin II receptor blockers
- Angiotensin-converting enzyme (ACE) inhibitors
- Beta blockers
- Dehydration
- Destruction of red blood cells due to severe injury or burns
- Excessive use of potassium supplements
- Type 1 diabetes[3]
Image 2: Dialysis for Chronic Kidney Disease.
Epidemiology[edit | edit source]
Hyperkalemia is unusual in the general population, reported in less than 5% of the population, worldwide.
- Affects up to 10% of all hospitalized patients, most cases in hospitalized patients are due to medications and renal insufficiency.
- Diabetes, malignancy, extremes of age, and acidosis are other important causes in inpatients.
- Hyperkalemia is rare in children but may occur in up to 50% of premature infants.
- Hyperkalemia is more commonly reported in men than women perhaps due to increased muscle mass and higher rates of rhabdomyolysis and increased prevalence of neuromuscular disease.
Today there is a risk that empirical use of ACE inhibitors may cause hyperkalemia, which can be of concern in high risk populations eg diabetics, those with heart failure, and peripheral vascular disease[2].
Characteristics/Clinical Presentation[edit | edit source]
Hyperkalemia most commonly occurs in patients with chronic renal failure and is also correlated with diabetes. [4] [5]
Image 3: ECG is monitored in patients with hyperkalemia:
Signs and Symptoms
- muscular weakness
- flaccid paralysis
- ileus
- ECG changes[4]
- nausea
- slow, weak or irregular pulse
- sudden collapse (heart rate too slow or stops)[6]
- paraestesias
- fatigue
- palpitations
Potassium is regulated through excretion via the renal system. When this system's function declines, the extracellular potassium concentration increases and can lead to membrane excitability. Some signs and symptoms listed above are a result of the impaired nerve conduction and muscle contraction dysfunction. Muscular dysfunction includes the cardiac system and can lead to life threatening ventricular arrhythmias. Electrocardiogram (ECG) dysfunction is more common in patients with acute hyperkalemia.[7]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Initial diagnosis is initiated with patient history, medication review, and physical examination.
Laboratory tests include:
- serum electrolytes (especially potassium and glucose [7])
- creatinine
- blood urea nitrogen (BUN)
- spot urine test (potassium, creatinine, and osmoles)
- transtubular potassium gradient (assessment of renal potassium handling)
- trial of oral fludrocortisone (Florinef)[4]
Patients will likely not present with symptoms of hyperkalemia until potassium levels have exceeded 7 mmol/L. However, immediate medical attention is required when potassium level exceed 6.5 mmol/L or exceed 6.0 mmol/L with ECG changes consistent with hyperkalemia.[7]
Systemic Involvement [edit | edit source]
Table 5-10 Clinical Features of Various Electrolyte Imbalances[8]
| Potassium Imbalance (hyperkalemia) | System Dysfunction |
| Cardiovascular | tachycardia and later bradycardia, ECG changes, cardiac arrest (with levels .7.0 mEq/L) |
| GI | nausea, diarrhea, abdominal cramps |
| Musculoskeletal | muscle weakness, flaccid paralysis |
| Genitourinary | oliguria, anuria |
| Central nervous system | areflexia progressing to weakness, numbness, tingling, and flaccid paralysis |
| Acid-base balance | metabolic acidosis |
Treatment[edit | edit source]
The urgency with which hyperkalemia should be managed depends on how rapidly the condition developed, the absolute serum potassium level, the degree of symptoms, and the cause.[2]
- The presence of ECG changes, a rapid rise of serum potassium, indications of decreased kidney function, or significant acidosis require immediate medical treatment for hyperkalemia.
- Although ECG changes are common indicators for severe hyperkalemia, the patient may still have life threatening hyperkalemia even if ECG readings are normal.
- The intent of immediate medical intervention is to stabilize the myocardium to prevent arrhythmias.
In addition to the medications listed in Table 5, total body potassium levels can be lowered through kidney excretion, gastrointestinal (GI) elimination, or dialysis. Lowering via kidney excretion is achieved by the use of diuretics, while lowering via GI elimination occurs with the use of Kayexalate. Long term management is focused on addressing the underlying cause, which can be achieved by discontinuing medications or consuming low potassium diets.[4]
Figure 2: Algorithm for the management of hyperkalemia.[4]
Foods high in potassium can also be implicated in the development of hyperkalemia.
|
Table 2. High-potassium foods[7] (National Kidney foundation, 2010) |
|
- salt substitutes and salt free broth - yogurt, milk - molasses - seaweed - chocolate - bran cereal, wheat germ, granola - vegetables (acorn squash, artichoke, bamboo shoots, beets, broccoli, brussel sprouts, chinese cabbage, carrots, greens (except kale), kohlrabi, mushrooms (canned), parsnips, potatoes, pumpkin, rutabagas, spinach, tomatoes, vegetable juices) - dried fruit (apricot, dates, figs, raisins, prunes) - nuts and seeds, (peanut butter) - dried peas and beans (lima beans, black beans, refried beans, lentils, legumes) - fruit and juice (apricot, avocado, banana, cantaloupe, grapefruit, honeydew, kiwi fruit, mango, nectarine, orange, papaya, pomegranate, prune)
|
Physical Therapy Management[edit | edit source]
Hyperkalemia is a disorder that is not managed primarily by a physical therapist, however physical therapists should be aware of signs and symptoms of this disorder and should refer the patient to a medical doctor when indicated.
- Potassium levels < 3.2 mEq/L or > 5.1 mEq/L are contraindicated for physical therapy intervention due to the potential for arrhythmia and tetany.
- When potassium levels are not within the normal range (3.5-5.0 mEq/L) exercise is not effective due to decreased muscle pH and action potentials as well as inhibition of motor neurons.
- With a patient who has marginal potassium levels, vital signs (including pulse rhythm) and any signs of dizziness, muscle weakness or cramping, numbness or tingling, and changes in balance should be closely monitored.
At this time, no research addresses the change in potassium level that occurs with exercise. However, it is known that patients with hyperkalemia are at risk for ventricular arrhythmias which can result in reduced exercise tolerance.[8]
References[edit | edit source]
see adding references tutorial.
- ↑ Healthline 5 Things to Know About Hyperkalemia for National Kidney Month Available: https://www.healthline.com/health/high-potassium/hyperkalemia-facts(accessed 18.9.2021)
- ↑ 2.0 2.1 2.2 2.3 Simon LV, Hashmi MF, Farrell MW. Hyperkalemia. StatPearls [Internet]. 2020 Dec 1.Available:https://www.ncbi.nlm.nih.gov/books/NBK470284/ (accessed 18.9.2021)
- ↑ Mayo clinic Hyperkalemia Available: https://www.mayoclinic.org/symptoms/hyperkalemia/basics/causes/sym-20050776 (accessed 18.9.2021)
- ↑ 4.0 4.1 4.2 4.3 4.4 Hollander-Rodriguez JC, Calvert, Jr. JF. Hyperkalemia. American Family Physician 2006; 73(2):283-290. Available from: PubMed. http://www.ncbi.nlm.nih.gov/pubmed/16445274 )22 March 2013)
- ↑ Tamirisa KP, Aaronson KD, Koelling TM. Spironolactone-induced renal insufficiency and hyperkalemia in patients with heart failure, American Heart J 2004; 148(6):971-978. Available from: Europe Pubmed Central. http://www.sciencedirect.com/science/article/pii/S0002870304007501 (Accessed 4 April 2013)
- ↑ Dugdale DC, Zieve D. MedlinePlus. [homepage on the Internet]. 2011 [cited 2013 Mar 22]. Available from: U.S. National Library of Medicine, National Institutes of Health Web site: http://www.nlm.nih.gov/medlineplus/ency/article/001179.htm
- ↑ 7.0 7.1 7.2 7.3 Raymond C, Sood A, Wazny L. Treatment of hyperkalemia in patients with chronic kidney disease--a focus on medications. CANNT Journal [serial on the Internet]. (2010, July), [cited March 22, 2013]; 20(3): 49-54. Available from: CINAHL with Full Text. http://search.ebscohost.com/login.aspx?direct=true&db=c8h&AN=2010782358&site=ehost-live (accessed 22 Mar 2013)
- ↑ 8.0 8.1 Goodman CC & Fuller KS. In K Falk editor. Pathology: Implications for the Physical Therapist. St. Louis: Saunders Elsevier; 2009. pp.150, 157, 187-189, 480, 558, 927, 1243, 1640-1641