Gait Deviations Associated with Lower Leg and Foot Pain Syndromes: Difference between revisions
No edit summary |
(added three updated references) |
||
| (32 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Stacy Schiurring|Stacy Schiurring]] based on the course by [https://members.physio-pedia.com/instructor/damien-howell | <div class="editorbox"> '''Original Editor '''- [[User:Stacy Schiurring|Stacy Schiurring]] based on the course by [https://members.physio-pedia.com/instructor/damien-howell/ Damien Howell]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
This article discusses gait deviations associated with pain syndromes in the lower leg and foot. While this information focuses on certain regions of the body, remember that the human body functions within a kinetic chain. No one movement is ever completely isolated and | This article discusses gait deviations associated with [[Pain Behaviours|pain]] syndromes in the lower leg and foot. While this information focuses on certain regions of the body, remember that the human body functions within a [[Kinetic Chain|kinetic chain.]] No one movement is ever completely isolated and without effect on another.<ref name=":0">Howell, D, Gait Deviation Associated with Pain Syndromes in the Lower Leg and Foot. Gait Analysis. Plus. 2022</ref> | ||
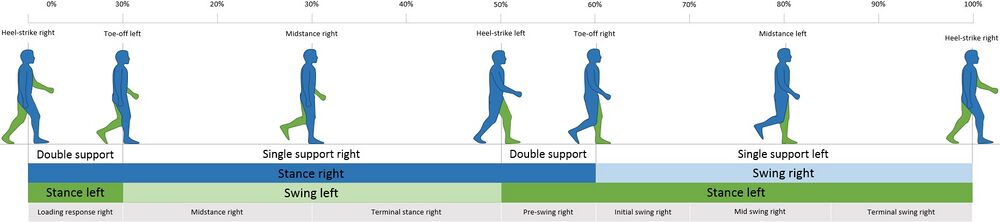
For a review of the gait cycle, please | For a review of the gait cycle, please read [[Gait Cycle|this article]]. For an overview of gait deviations, please review [[Gait Deviations|this article]]. To review common gait terminology and definitions, please see [[Gait Definitions|this article]]. | ||
[[File:Gait cycle.jpg|center|1000x1000px]] | [[File:Gait cycle.jpg|center|1000x1000px]] | ||
== Anatomy Review == | == Anatomy Review == | ||
[[File:Bigstock_Image_-Anatomy_Bones_Of_The_Foot_-ID_404217734.jpg|alt=|right|450x450px]] | [[File:Bigstock_Image_-Anatomy_Bones_Of_The_Foot_-ID_404217734.jpg|alt=|right|450x450px]] | ||
The ankle is the part of the lower limb encompassing the distal portion of the leg and proximal portions of the foot. The ankle encompasses the [[Ankle Joint|ankle joint]], an articulation between the [[tibia]] and [[fibula]] of the leg and the [[talus]] of the foot. | The ankle is the part of the lower limb, encompassing the distal portion of the leg and proximal portions of the foot. The ankle encompasses the [[Ankle Joint|ankle joint]], an articulation between the [[tibia]] and [[fibula]] of the leg and the [[talus]] of the foot. | ||
The [[Foot Anatomy|foot]] is the part of the lower limb distal to the ankle joint. It is covered on its dorsal surface by loosely adherent skin | The [[Foot Anatomy|foot]] is the part of the lower limb distal to the ankle joint. It is covered on its dorsal surface by loosely adherent skin. On its plantar surface, it is covered by thick hairless skin that is tough and strongly adherent to the underlying plantar aponeurosis. The foot contains 26 small bones that are designed for weight bearing and force distribution. The bony alignment creates three arches the provide efficient weight distribution while avoiding compression of plantar neuro-vascular structures. The three arches (medial and lateral longitudinal and the transverse arch) together create an architectural vault, which is one of the strongest load-bearing structures known to mankind.<ref>The Editors of Encyclopaedia Britannica. Foot. Available from: https://www.britannica.com/science/foot (accessed 28/05/2022).</ref><ref>Asghar A, Naaz S. The transverse arch in the human feet: A narrative review of its evolution, anatomy, biomechanics and clinical implications. Morphologie. 2022 Dec 1;106(355):225-34.</ref> | ||
Please read the linked article for a more in-depth anatomical review of the [[Foot Anatomy|Foot and ankle]]. | Please read the linked article for a more in-depth anatomical review of the [[Foot Anatomy|Foot and ankle]]. | ||
== Ground Reaction Forces == | == Ground Reaction Forces == | ||
Ground reaction force is a summation of all the forces transmitted from the ground up into the body.<ref name=":0" /> | [[File:Vert GRF.jpeg|thumb|Example of a vertical ground reaction force. ]] | ||
'''Ground reaction force''' is a summation of all the forces transmitted from the ground up into the body.<ref name=":0" /> Ground reaction force is influenced from all directions: vertical, anterior-posterior, and medial-lateral. These forces are typically measured and recorded using a three-dimensional force plate.<ref name=":1">Yu L, Mei Q, Xiang L, et al. [https://www.frontiersin.org/articles/10.3389/fbioe.2021.629809/full#refer1 Principal Component Analysis of the Running Ground Reaction Forces With Different Speeds]. Front. Bioeng. Biotechnol.. 2021; 9:629809.</ref> | |||
[[File: Braking forces.jpeg|thumb|Example of an anterior-posterior ground reaction force]] | |||
During walking, the '''vertical ground reaction force''' is the largest component of the total ground reaction force. It creates forces greater than a person's total body weight per step. The graphed curve of the vertical ground reaction force consists of two peaks: the passive (weight acceptance as the heel strikes the ground) peak and the active (push off) peak.<ref name=":1" /><ref name=":2">Jiang X, Napier C, Hannigan B, Eng JJ, Menon C. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7436236/ Estimating vertical ground reaction force during walking using a single inertial sensor]. Sensors. 2020 Jan;20(15):4345.</ref> The passive peak is caused by the foot pushing against the ground, whereas the active peak is caused by the active force applied by the foot as it pushes away from the ground. The '''anterior-posterior ground reaction force''' includes braking peak and propulsion peak.<ref name=":1" /> The unique patterns of these peaks illustrate the load forces at the joints and muscles of the lower extremity. These forces felt throughout the limb can influence the development or exacerbation of musculoskeletal overuse or stress injuries.<ref name=":2" /><ref>Ahn J, Simpkins C, Yang F. Ground reaction forces and muscle activities during anteriorly-loaded overground walking: Preliminary results. International Journal of Industrial Ergonomics. 2022 Jul 1;90:103328.</ref> | |||
When interpreting a ground reaction curve, the steeper the curve the more significant the impact forces. The curve on the anterior-posterior curve (the breaking forces) will be negative. In general, the greater the forces, the greater risk for stress or overuse injuries.<ref name=":0" /> | |||
Please view the following video for a quick yet detailed overview of ground reaction forces during the human gait cycle. This video provides an excellent visualisation of how ground reaction forces shift in different directions as the person moves through space. | |||
{{#ev:youtube| Y2RHvicAM2o |500}}<ref>JYouTube. Ground Reaction Force During the Gait Cycle | Alexandra Kopelovich. | |||
Available from: https://www.youtube.com/watch?v=Y2RHvicAM2o [last accessed 29/05/2022]</ref> | |||
== Gait Deviations == | == Gait Deviations<ref name=":0" /> == | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
| Line 32: | Line 36: | ||
!'''Secondary Signs Associated with Deviant Movement''' | !'''Secondary Signs Associated with Deviant Movement''' | ||
|- | |- | ||
|'''Late heel off''' | |'''Late heel off'''<ref name=":3">Kang MH. [https://www.jstage.jst.go.jp/article/jpts/30/5/30_jpts-2018-002/_pdf Influence of ankle dorsiflexion range of motion on heel-rise time during gait]. Journal of Physical Therapy Science. 2018;30(5):694-6.</ref> | ||
ie: prolonged heel contact | ie: prolonged heel contact | ||
|The heel of the trailing foot lifts off the ground just prior to the contact of the leading foot. | |The heel of the trailing foot lifts off the ground just prior to the contact of the leading foot. | ||
| Line 44: | Line 48: | ||
* The appearance of a "geriatric gait" | * The appearance of a "geriatric gait" | ||
|- | |- | ||
|'''Early heel off''' | |'''Early heel off'''<ref name=":3" /> | ||
ie: | ie: premature heel rise | ||
|(Same as above) | |(Same as above) | ||
|The heel of the trailing foot leaves the ground | |The heel of the trailing foot leaves the ground prior to the leading foot heel strike. | ||
* Bouncy gait | * Bouncy gait | ||
| Line 55: | Line 59: | ||
* Hyperextension of the knee during terminal stance | * Hyperextension of the knee during terminal stance | ||
* Hyperflexion of the knee during terminal stance | * Hyperflexion of the knee during terminal stance | ||
* An increase in the up and down motion of centre of mass | * An increase in the up and down motion of [[Centre of Gravity|centre of mass]] | ||
* Loud heel strike | * Loud heel strike | ||
|- | |- | ||
| Line 68: | Line 72: | ||
* Increased knee extension or hyperextension, particularly at heel strike | * Increased knee extension or hyperextension, particularly at heel strike | ||
* Increased hip extension in terminal stance | * Increased hip extension in terminal stance | ||
* Foot may cross midline | * Foot may cross the midline | ||
* Slow walking cadence, less than 120 steps/min; slow running cadence, less than 180 steps/min | * Slow walking cadence, less than 120 steps/min; slow running cadence, less than 180 steps/min | ||
|- | |- | ||
|'''Toe out''' | |'''Toe out'''<ref name=":4">Mousavi SH, van Kouwenhove L, Rajabi R, Zwerver J, Hijmans JM. [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0246425 The effect of changing foot progression angle using real-time visual feedback on rearfoot eversion during running.] PloS one. 2021 Feb 10;16(2):e0246425.</ref> | ||
|During walking when viewed from front or behind, the foot is 5-10 degrees out | |During walking when viewed from the front or behind, the foot is 5-10 degrees out from the line of progression. | ||
* It is common to see two of the lateral toes when viewed from behind. | * It is common to see two of the lateral toes when viewed from behind. | ||
| Line 86: | Line 90: | ||
* When viewed from behind, the lateral malleolus is visible but the medial malleolus is not | * When viewed from behind, the lateral malleolus is visible but the medial malleolus is not | ||
|- | |- | ||
|'''Toe in''' | |'''Toe in'''<ref name=":4" /> | ||
|During walking when viewed from behind, should not be able to view the big toe. | |During walking when viewed from behind, should not be able to view the big toe. | ||
|The big toe is visible during walking when viewed from behind. | |The big toe is visible during walking when viewed from behind. | ||
| Line 99: | Line 103: | ||
|- | |- | ||
|'''Loud foot strike''' | |'''Loud foot strike''' | ||
|It is expected for foot strike to emit a sound. | |It is expected for foot strike to emit a sound. The sound is representative of the ground reaction force. | ||
|If the sound of the foot strike is ''asymmetrical'' between the lower extremities, or between the non-painful and the painful side. | |If the sound of the foot strike is ''asymmetrical'' between the lower extremities, or between the non-painful and the painful side. | ||
| | | | ||
* Loud single or double sounds with the same foot strike | * Loud single or double sounds with the same foot strike | ||
| Line 115: | Line 119: | ||
Also deviant is the heel whip is greater on one side compared to the other side. | |||
Also deviant is when the heel whip is greater on one side compared to the other side. | |||
* Can occur due to an anatomically long leg | * Can occur due to an anatomically long leg | ||
| Line 131: | Line 136: | ||
When viewed from behind: | When viewed from behind: | ||
* | * Can view two or fewer of the lateral toes | ||
* | * The navicular bone is not visible | ||
|When viewed from behind: | |When viewed from behind: | ||
* | * Heel of the shoe is lifted off the ground | ||
* | * Bisection of the calcaneous or shoe heel counter is tilted medial relative to the ground | ||
* | * Can view more than two of the lateral toes | ||
* | * If the navicular bone is plantarflexed and ABDucted | ||
| | | | ||
* Contralateral pelvic drop | * Contralateral pelvic drop | ||
| Line 166: | Line 171: | ||
* Absent windlass effect | * Absent windlass effect | ||
|} | |} | ||
<blockquote>[[File:Windlass Test.png|right|frameless|386x386px|alt=]]'''What is the [[Windlass Test|Windlass effect]] (Windlass mechanism)?'''<ref>Shono H, Matsumoto Y, Kokubun T, Tsuruta A, Miyazawa T, Kobayashi A, Kanemura N. Determination of relationship between foot arch, hindfoot, and hallux motion using Oxford foot model: Comparison between walking and running. Gait & Posture. 2022 Feb 1;92:96-102.</ref> | |||
== Pain Syndromes Associated with Gait Deviations == | According to a 2004 study<ref name=":5" /> published in the Journal of Athletic Training: | ||
* A “windlass” is the tightening of a rope or cable. | |||
* The plantar fascia "simulates a cable" attached between the calcaneus and the metatarsophalangeal (MTP) joints. | |||
* Dorsiflexion during the propulsion phase of gait tightens the plantar fascia around the head of the metatarsal. This tightening of the fascia shortens the distance between the calcaneus and metatarsals to elevate the medial longitudinal arch. This shortening of the plantar fascia is the hallmark of the windlass mechanism principle. | |||
* From heel strike to weight acceptance: foot pronation increases the distance between the calcaneus and metatarsals. This lengthening applies tension stress to the plantar fascia. | |||
* From midstance through the propulsive phase (i.e. the period from the end of midstance when the heel lifts to toe off<ref>Kawalec JS. 12 - Mechanical testing of foot and ankle implants. In Friss E, editor. Mechanical testing of orthopaedic implants. Woodhead Publishing, 2017. p231-53.</ref>): foot supination occurs causing the foot becomes a rigid lever arm using the windlass mechanism to propel gait. As with pronation, forces generated during supination also apply tension to the plantar fascia.<ref name=":5">Bolgla LA, Malone TR. [https://www.ncbi.nlm.nih.gov/pmc/articles/pmc385265/ Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice]. Journal of athletic training. 2004 Jan;39(1):77.</ref></blockquote> | |||
== Pain Syndromes Associated with Gait Deviations<ref name=":0" /> == | |||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
| Line 194: | Line 208: | ||
* Achilles pain (Achilles is relatively short) | * Achilles pain (Achilles is relatively short) | ||
* Ankle pain | * Ankle pain | ||
* Plantar heel pain syndrome | * [[Plantar Heel Pain|Plantar heel pain syndrome]] | ||
* Metatarsalgia | * Metatarsalgia | ||
* Forefoot pain | * Forefoot pain | ||
| Line 204: | Line 218: | ||
* Acetabular labral injury | * Acetabular labral injury | ||
* Anterior and or lateral knee pain | * Anterior and or lateral knee pain | ||
* IT band syndrome | * [[Iliotibial Band Syndrome|IT band syndrome]] | ||
* Patellofemoral arthralgia | * Patellofemoral arthralgia | ||
* Medial tibial stress syndrome | * [[Medial Tibial Stress Syndrome|Medial tibial stress syndrome]] | ||
* Stress fractures | * Stress fractures | ||
* Achilles pain | * Achilles pain | ||
| Line 213: | Line 227: | ||
|'''Toe out''' | |'''Toe out''' | ||
| | | | ||
* Hip osteoarthritis | * Hip [[osteoarthritis]] | ||
* Knee osteoarthritis | * Knee osteoarthritis | ||
* Gait pattern can become habitual | * Gait pattern can become habitual post total joint replacements | ||
* Patellofemoral arthralgia | * Patellofemoral arthralgia | ||
* Medial tibial stress syndrome | * Medial tibial stress syndrome | ||
* Tibial stress fracture | * Tibial [[Stress Fractures|stress fracture]] | ||
* Achilles pain | * Achilles pain | ||
* Plantar heel pain syndrome | * Plantar heel pain syndrome | ||
* Metatarsalgia | * Metatarsalgia | ||
|- | |||
|'''Toe in''' | |||
| | |||
* Anterior knee pain | |||
* Patellofemoral arthralgia | |||
* Medial tibial stress syndrome | |||
* Posterior tibial tendinopathy | |||
* Plantar heel pain | |||
* Metatarsalgia pain | |||
* [[Hallux Valgus|Hallux valgus]] pain | |||
|- | |- | ||
|'''Loud foot strike''' | |'''Loud foot strike''' | ||
| Line 260: | Line 284: | ||
| | | | ||
* Plantar heel pain syndrome | * Plantar heel pain syndrome | ||
* Hallux limitus | * Hallux limitus<ref>Viehofer, A. F., Vich, M., Wirth, S. H., Espinosa, N., & Camenzind, R. S. (2019). [https://pubmed.ncbi.nlm.nih.gov/30738612/ The Role of Plantar Fascia Tightness in Hallux Limitus: A Biomechanical Analysis]. J Foot Ankle Surg, 58(3), 465-469. </ref> | ||
* First MTP joint osteoarthritis | * First MTP joint osteoarthritis | ||
* Osseous chondroma of the great toe | * Osseous chondroma of the great toe | ||
| Line 270: | Line 294: | ||
== Resources == | == Resources == | ||
'''Recommended video of gait deviations:''' | |||
{{#ev:youtube| nekqkxLeGOw |500}}<ref>YouTube. Gait Deviations: Compensations at Ankle & Foot | Alexandra Kopelovich. Available from: https://www.youtube.com/watch?v=nekqkxLeGOw [last accessed 30/05/2022]</ref> | |||
'''Recommended Journal Articles:''' | |||
* Steffen TM, Hacker TA, Mollinger L. [https://academic.oup.com/ptj/article/82/2/128/2836941 Age-and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds]. Physical therapy. 2002 Feb 1;82(2):128-37. | |||
* Naylor BH, Seidman D, Scuderi GR. [https://cme.lww.com/ovidfiles/00124635-202107150-00006.pdf Bridging the Gap: The Influence of Foot and Ankle Pathomechanics in Total Knee Arthroplasty]. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2021 Jul 15;29(14):e693-701. | |||
* | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Course Pages]] | |||
[[Category:Plus Content]] | |||
[[Category:Gait]] | |||
[[Category:Pain]] | |||
Latest revision as of 05:57, 30 January 2023
Top Contributors - Stacy Schiurring, Jess Bell, Kim Jackson and Lucinda hampton
Introduction[edit | edit source]
This article discusses gait deviations associated with pain syndromes in the lower leg and foot. While this information focuses on certain regions of the body, remember that the human body functions within a kinetic chain. No one movement is ever completely isolated and without effect on another.[1]
For a review of the gait cycle, please read this article. For an overview of gait deviations, please review this article. To review common gait terminology and definitions, please see this article.
Anatomy Review[edit | edit source]
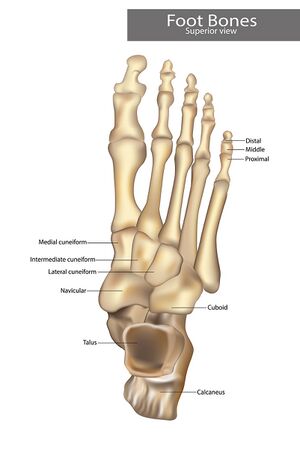
The ankle is the part of the lower limb, encompassing the distal portion of the leg and proximal portions of the foot. The ankle encompasses the ankle joint, an articulation between the tibia and fibula of the leg and the talus of the foot.
The foot is the part of the lower limb distal to the ankle joint. It is covered on its dorsal surface by loosely adherent skin. On its plantar surface, it is covered by thick hairless skin that is tough and strongly adherent to the underlying plantar aponeurosis. The foot contains 26 small bones that are designed for weight bearing and force distribution. The bony alignment creates three arches the provide efficient weight distribution while avoiding compression of plantar neuro-vascular structures. The three arches (medial and lateral longitudinal and the transverse arch) together create an architectural vault, which is one of the strongest load-bearing structures known to mankind.[2][3]
Please read the linked article for a more in-depth anatomical review of the Foot and ankle.
Ground Reaction Forces[edit | edit source]
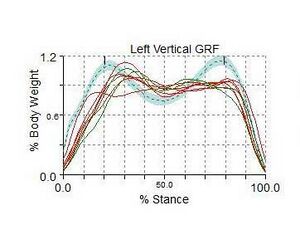
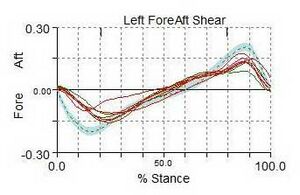
Ground reaction force is a summation of all the forces transmitted from the ground up into the body.[1] Ground reaction force is influenced from all directions: vertical, anterior-posterior, and medial-lateral. These forces are typically measured and recorded using a three-dimensional force plate.[4]
During walking, the vertical ground reaction force is the largest component of the total ground reaction force. It creates forces greater than a person's total body weight per step. The graphed curve of the vertical ground reaction force consists of two peaks: the passive (weight acceptance as the heel strikes the ground) peak and the active (push off) peak.[4][5] The passive peak is caused by the foot pushing against the ground, whereas the active peak is caused by the active force applied by the foot as it pushes away from the ground. The anterior-posterior ground reaction force includes braking peak and propulsion peak.[4] The unique patterns of these peaks illustrate the load forces at the joints and muscles of the lower extremity. These forces felt throughout the limb can influence the development or exacerbation of musculoskeletal overuse or stress injuries.[5][6]
When interpreting a ground reaction curve, the steeper the curve the more significant the impact forces. The curve on the anterior-posterior curve (the breaking forces) will be negative. In general, the greater the forces, the greater risk for stress or overuse injuries.[1]
Please view the following video for a quick yet detailed overview of ground reaction forces during the human gait cycle. This video provides an excellent visualisation of how ground reaction forces shift in different directions as the person moves through space.
Gait Deviations[1][edit | edit source]
| Gait Deviation | Expected Movement Pattern | Deviant Movement Pattern | Secondary Signs Associated with Deviant Movement |
|---|---|---|---|
| Late heel off[8]
ie: prolonged heel contact |
The heel of the trailing foot lifts off the ground just prior to the contact of the leading foot. | The heel of the trailing foot stays on the ground beyond the moment of the leading foot heel strike.
|
|
| Early heel off[8]
ie: premature heel rise |
(Same as above) | The heel of the trailing foot leaves the ground prior to the leading foot heel strike.
|
|
| Stride length too long | During walking when viewed from the side, the linear distance from the foot strike to the person's centre of mass is relatively short. | During walking when viewed from the side, the linear distance from the foot strike to the person's centre of mass is too long. |
|
| Toe out[9] | During walking when viewed from the front or behind, the foot is 5-10 degrees out from the line of progression.
|
Greater than 10 degrees of toe out relative to the line of progression.
|
|
| Toe in[9] | During walking when viewed from behind, should not be able to view the big toe. | The big toe is visible during walking when viewed from behind.
|
|
| Loud foot strike | It is expected for foot strike to emit a sound. The sound is representative of the ground reaction force. | If the sound of the foot strike is asymmetrical between the lower extremities, or between the non-painful and the painful side. |
|
| Heel whip | This is the one gait deviation that occurs between the transition from stance to swing phase.
|
If the heel whip angle of rotation is greater than 10 degrees.
Also deviant is when the heel whip is greater on one side compared to the other side.
|
|
| Excessive pronation | A bisected calcaneus or shoe heel counter is perpendicular relative to the ground.
|
When viewed from behind:
|
|
| Absent windlass effect
ie: increased dorsiflexion of the first MTP joint |
During forefoot contact/terminal stance, there is normally 35-65 degrees of first MTP joint dorsiflexion.
|
|
|
| Decreased dorsiflexion of the first MTP joint | During forefoot contact/terminal stance when viewed from the side, there is normally 35-65 degrees of first MTP joint dorsiflexion. | During forefoot contact/terminal stance, there is less than 35 degrees of first MTP joint dorsiflexion. |
|
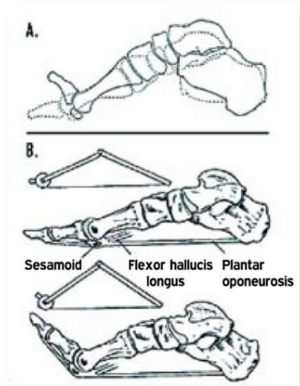
What is the Windlass effect (Windlass mechanism)?[10]
According to a 2004 study[11] published in the Journal of Athletic Training:
- A “windlass” is the tightening of a rope or cable.
- The plantar fascia "simulates a cable" attached between the calcaneus and the metatarsophalangeal (MTP) joints.
- Dorsiflexion during the propulsion phase of gait tightens the plantar fascia around the head of the metatarsal. This tightening of the fascia shortens the distance between the calcaneus and metatarsals to elevate the medial longitudinal arch. This shortening of the plantar fascia is the hallmark of the windlass mechanism principle.
- From heel strike to weight acceptance: foot pronation increases the distance between the calcaneus and metatarsals. This lengthening applies tension stress to the plantar fascia.
- From midstance through the propulsive phase (i.e. the period from the end of midstance when the heel lifts to toe off[12]): foot supination occurs causing the foot becomes a rigid lever arm using the windlass mechanism to propel gait. As with pronation, forces generated during supination also apply tension to the plantar fascia.[11]
Pain Syndromes Associated with Gait Deviations[1][edit | edit source]
| Gait Deviation | Associated Pain
and Pain Syndromes |
|---|---|
| Late heel off
ie: prolonged heel contact |
|
| Early heel off
ie: premature heel rise |
|
| Stride length too long |
|
| Toe out |
|
| Toe in |
|
| Loud foot strike |
|
| Heel whip |
|
| Excessive pronation |
|
| Absent windlass effect |
|
| Decreased dorsiflexion of the first MTP joint |
|
Resources[edit | edit source]
Recommended video of gait deviations:
Recommended Journal Articles:
- Steffen TM, Hacker TA, Mollinger L. Age-and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Physical therapy. 2002 Feb 1;82(2):128-37.
- Naylor BH, Seidman D, Scuderi GR. Bridging the Gap: The Influence of Foot and Ankle Pathomechanics in Total Knee Arthroplasty. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2021 Jul 15;29(14):e693-701.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Howell, D, Gait Deviation Associated with Pain Syndromes in the Lower Leg and Foot. Gait Analysis. Plus. 2022
- ↑ The Editors of Encyclopaedia Britannica. Foot. Available from: https://www.britannica.com/science/foot (accessed 28/05/2022).
- ↑ Asghar A, Naaz S. The transverse arch in the human feet: A narrative review of its evolution, anatomy, biomechanics and clinical implications. Morphologie. 2022 Dec 1;106(355):225-34.
- ↑ 4.0 4.1 4.2 Yu L, Mei Q, Xiang L, et al. Principal Component Analysis of the Running Ground Reaction Forces With Different Speeds. Front. Bioeng. Biotechnol.. 2021; 9:629809.
- ↑ 5.0 5.1 Jiang X, Napier C, Hannigan B, Eng JJ, Menon C. Estimating vertical ground reaction force during walking using a single inertial sensor. Sensors. 2020 Jan;20(15):4345.
- ↑ Ahn J, Simpkins C, Yang F. Ground reaction forces and muscle activities during anteriorly-loaded overground walking: Preliminary results. International Journal of Industrial Ergonomics. 2022 Jul 1;90:103328.
- ↑ JYouTube. Ground Reaction Force During the Gait Cycle | Alexandra Kopelovich. Available from: https://www.youtube.com/watch?v=Y2RHvicAM2o [last accessed 29/05/2022]
- ↑ 8.0 8.1 Kang MH. Influence of ankle dorsiflexion range of motion on heel-rise time during gait. Journal of Physical Therapy Science. 2018;30(5):694-6.
- ↑ 9.0 9.1 Mousavi SH, van Kouwenhove L, Rajabi R, Zwerver J, Hijmans JM. The effect of changing foot progression angle using real-time visual feedback on rearfoot eversion during running. PloS one. 2021 Feb 10;16(2):e0246425.
- ↑ Shono H, Matsumoto Y, Kokubun T, Tsuruta A, Miyazawa T, Kobayashi A, Kanemura N. Determination of relationship between foot arch, hindfoot, and hallux motion using Oxford foot model: Comparison between walking and running. Gait & Posture. 2022 Feb 1;92:96-102.
- ↑ 11.0 11.1 Bolgla LA, Malone TR. Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice. Journal of athletic training. 2004 Jan;39(1):77.
- ↑ Kawalec JS. 12 - Mechanical testing of foot and ankle implants. In Friss E, editor. Mechanical testing of orthopaedic implants. Woodhead Publishing, 2017. p231-53.
- ↑ Viehofer, A. F., Vich, M., Wirth, S. H., Espinosa, N., & Camenzind, R. S. (2019). The Role of Plantar Fascia Tightness in Hallux Limitus: A Biomechanical Analysis. J Foot Ankle Surg, 58(3), 465-469.
- ↑ YouTube. Gait Deviations: Compensations at Ankle & Foot | Alexandra Kopelovich. Available from: https://www.youtube.com/watch?v=nekqkxLeGOw [last accessed 30/05/2022]