Hormone Replacement Therapy: Difference between revisions
Niha Mulla (talk | contribs) No edit summary |
No edit summary |
||
| (18 intermediate revisions by 2 users not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
[[ | [[File:HRT med.jpeg|thumb|HRT ]] | ||
[[ | [[Hormones|Hormone]] replacement therapy (HRT) is a treatment that relieves symptoms of [[menopause]], by supplementing the hormones that are at a lower level.<ref name=":1">Hickey M, Elliott J, Davison SL. Hormone replacement therapy. Bmj. 2012 Feb 16;344.</ref><ref name=":0">Sullivan SD, Sarrel PM, Nelson LM. Hormone replacement therapy in young women with primary ovarian insufficiency and early menopause. Fertility and sterility. 2016 Dec 1;106(7):1588-99.</ref> Conventional HRT includes an [[estrogen]] and progesterone component to mimic hormones created by the human ovary.<ref name=":2">Harper-Harrison G, Shanahan MM. Hormone Replacement Therapy. InStatPearls [Internet] 2022 Feb 17. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK493191/ (accessed 21.12.2022)</ref> | ||
Since the 2002 Women’s Health Initiative (WHI) trials, the risks of HRT are low for healthy women less than age 60 or within ten years from menopause, has been found to be low. For women experiencing troublesome vasomotor symptoms, it can be a good solution. HRT also has a role in preventing [[osteoporosis]] in appropriate populations.<ref name=":3">Mehta J, Kling JM, Manson JE. Risks, benefits, and treatment modalities of menopausal hormone therapy: current concepts. Frontiers in Endocrinology. 2021 Mar 26;12:564781. Available: https://www.frontiersin.org/articles/10.3389/fendo.2021.564781/full<nowiki/>(accessed 21.12.2022)</ref> | |||
HRT should only be for a few years, and close monitoring is required. When symptoms of menopause are mild, then education should be provided about the benefits and harm of these hormones.<ref name=":2" /> | |||
== Administration == | |||
There are many estrogen and progestogen choices that can be administrated orally or transdermally either through cream, patch, vaginal inserts, or subdermal pellets. Each route of administration has unique benefits and risks. | |||
* Oral Estrogen: Any estrogen administered orally increases the risk of a [[Thrombosis|blood clot]]. | |||
* Transdermal Estrogen: Bypasses the hepatic metabolism and the risk for blood clotting is negated. | |||
* Progestin administration: usually via the oral route.<ref name=":2" /> | |||
==== | == Indications == | ||
The presence of bothersome vasomotor symptoms is the main indication for HRT. Vasomotor symptoms are common during the menopause transition and affect about 80% of women, and are severe in about 20% of these women. The duration of these symptoms varies, with a median of 4 to 7 years, but may continue for as many as 12 to 14 years in about 10% of women. HRT may be indicated when menopausal symptoms are adversely affecting [[Quality of Life|quality of life]].<ref name=":1" /> For Symptoms of menopause see [[Menopause|here]] | |||
== Safety Issues == | |||
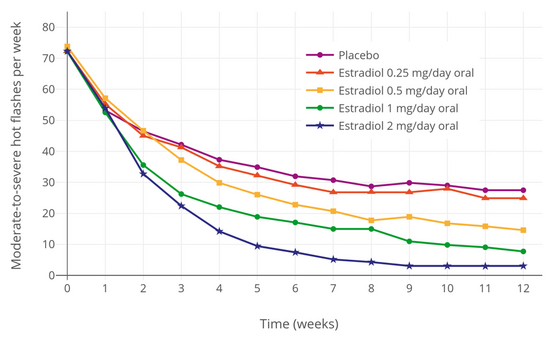
[[File:Hot flashes with placebo and different doses of oral estradiol in menopausal women.png|thumb|556x556px|Hot flashes with placebo or drug|alt=]] | |||
We know now that the safety of HRT depends on a woman’s age and length of time since menopause. As such the benefits tend to outweigh the risks in healthy women less than age 60 or within ten years from menopause. There are various types, formulations and routes of HRT available to women so that their healthcare practitioner can fashion their treatment to manage their symptoms.<ref name=":3" /> | |||
== Benefits == | |||
HRT is often helpful in relieving hot flushes and night sweats. Mood, [[Sleep Deprivation and Sleep Disorders|sleep]] and sex drive problems may also improve, as may joint aches, vaginal dryness and [[Urinary Incontinence|incontinence]] that some women experience.<ref name=":5">Health direct HRT Available:https://www.healthdirect.gov.au/hormone-replacement-therapy (accessed 22.12.2022)</ref> | |||
== | == Risks == | ||
The main risk with MHT is that some types lead to a slightly increased risk of developing [[Breast Cancer|breast cancer]] or [[thrombosis]]. On the other hand, it can be preventative for other conditions such as osteoporosis, [[Coronary Artery Disease (CAD)|heart disease]], [[diabetes]] and some types of cancers.<ref name=":5" /> | |||
Variables to take into consideration include: | |||
# Age: Women who start treatment earlier as symptoms appear are at low risk of side effects where as women who start HRT later for example 10 years after menopause are at the higher risk of developing side effects. | |||
# Type of hormone therapy: HRT with both estrogen and progesterone is a safer choice, rather than only estrogen. | |||
# May not be appropriate if medical history of: breast cancer; [[Endometrial Cancer|endometrial cancer]]; other cancers that are dependent on hormones; undiagnosed vaginal bleeding; untreated uterine lining thickening; raised risk of thrombosis; coronary artery disease, [[stroke]] or [[dementia]]; [[Deep Vein Thrombosis|DVT]]<nowiki/>s; untreated [[Hypertension|high blood pressure]].<ref name=":5" /> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Womens Health]] | [[Category:Womens Health]] | ||
Latest revision as of 13:17, 21 December 2022
Original Editor - Habibu salisu Badamasi
Top Contributors - Habibu Salisu Badamasi, Lucinda hampton and Niha Mulla
Introduction[edit | edit source]
Hormone replacement therapy (HRT) is a treatment that relieves symptoms of menopause, by supplementing the hormones that are at a lower level.[1][2] Conventional HRT includes an estrogen and progesterone component to mimic hormones created by the human ovary.[3]
Since the 2002 Women’s Health Initiative (WHI) trials, the risks of HRT are low for healthy women less than age 60 or within ten years from menopause, has been found to be low. For women experiencing troublesome vasomotor symptoms, it can be a good solution. HRT also has a role in preventing osteoporosis in appropriate populations.[4]
HRT should only be for a few years, and close monitoring is required. When symptoms of menopause are mild, then education should be provided about the benefits and harm of these hormones.[3]
Administration[edit | edit source]
There are many estrogen and progestogen choices that can be administrated orally or transdermally either through cream, patch, vaginal inserts, or subdermal pellets. Each route of administration has unique benefits and risks.
- Oral Estrogen: Any estrogen administered orally increases the risk of a blood clot.
- Transdermal Estrogen: Bypasses the hepatic metabolism and the risk for blood clotting is negated.
- Progestin administration: usually via the oral route.[3]
Indications[edit | edit source]
The presence of bothersome vasomotor symptoms is the main indication for HRT. Vasomotor symptoms are common during the menopause transition and affect about 80% of women, and are severe in about 20% of these women. The duration of these symptoms varies, with a median of 4 to 7 years, but may continue for as many as 12 to 14 years in about 10% of women. HRT may be indicated when menopausal symptoms are adversely affecting quality of life.[1] For Symptoms of menopause see here
Safety Issues[edit | edit source]
We know now that the safety of HRT depends on a woman’s age and length of time since menopause. As such the benefits tend to outweigh the risks in healthy women less than age 60 or within ten years from menopause. There are various types, formulations and routes of HRT available to women so that their healthcare practitioner can fashion their treatment to manage their symptoms.[4]
Benefits[edit | edit source]
HRT is often helpful in relieving hot flushes and night sweats. Mood, sleep and sex drive problems may also improve, as may joint aches, vaginal dryness and incontinence that some women experience.[5]
Risks[edit | edit source]
The main risk with MHT is that some types lead to a slightly increased risk of developing breast cancer or thrombosis. On the other hand, it can be preventative for other conditions such as osteoporosis, heart disease, diabetes and some types of cancers.[5]
Variables to take into consideration include:
- Age: Women who start treatment earlier as symptoms appear are at low risk of side effects where as women who start HRT later for example 10 years after menopause are at the higher risk of developing side effects.
- Type of hormone therapy: HRT with both estrogen and progesterone is a safer choice, rather than only estrogen.
- May not be appropriate if medical history of: breast cancer; endometrial cancer; other cancers that are dependent on hormones; undiagnosed vaginal bleeding; untreated uterine lining thickening; raised risk of thrombosis; coronary artery disease, stroke or dementia; DVTs; untreated high blood pressure.[5]
References[edit | edit source]
- ↑ 1.0 1.1 Hickey M, Elliott J, Davison SL. Hormone replacement therapy. Bmj. 2012 Feb 16;344.
- ↑ Sullivan SD, Sarrel PM, Nelson LM. Hormone replacement therapy in young women with primary ovarian insufficiency and early menopause. Fertility and sterility. 2016 Dec 1;106(7):1588-99.
- ↑ 3.0 3.1 3.2 Harper-Harrison G, Shanahan MM. Hormone Replacement Therapy. InStatPearls [Internet] 2022 Feb 17. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK493191/ (accessed 21.12.2022)
- ↑ 4.0 4.1 Mehta J, Kling JM, Manson JE. Risks, benefits, and treatment modalities of menopausal hormone therapy: current concepts. Frontiers in Endocrinology. 2021 Mar 26;12:564781. Available: https://www.frontiersin.org/articles/10.3389/fendo.2021.564781/full(accessed 21.12.2022)
- ↑ 5.0 5.1 5.2 Health direct HRT Available:https://www.healthdirect.gov.au/hormone-replacement-therapy (accessed 22.12.2022)