Synovium & Synovial Fluid: Difference between revisions
No edit summary |
No edit summary |
||
| Line 11: | Line 11: | ||
# Synovium (also called the synovial membrane) is a specialized connective soft-tissue membrane that lines the inner surface of synovial [[Joint Classification|joint]] capsules. Together with [[bone]], articular [[cartilage]], [[Tendon Anatomy|tendon]], [[ligament]], and fibrous capsule, it is an important component of the tissues that form an integrated joint. As such, it not only has its own specific functions but also interacts with other tissues in the joint both structurally and functionally<ref name=":3">Musculoskeletal Key [https://musculoskeletalkey.com/synovium-and-joint-biology/ Synovium] Available: https://musculoskeletalkey.com/synovium-and-joint-biology/<nowiki/>(accessed 18.6.2021)</ref>. | # Synovium (also called the synovial membrane) is a specialized connective soft-tissue membrane that lines the inner surface of synovial [[Joint Classification|joint]] capsules. Together with [[bone]], articular [[cartilage]], [[Tendon Anatomy|tendon]], [[ligament]], and fibrous capsule, it is an important component of the tissues that form an integrated joint. As such, it not only has its own specific functions but also interacts with other tissues in the joint both structurally and functionally<ref name=":3">Musculoskeletal Key [https://musculoskeletalkey.com/synovium-and-joint-biology/ Synovium] Available: https://musculoskeletalkey.com/synovium-and-joint-biology/<nowiki/>(accessed 18.6.2021)</ref>. | ||
# Synovial fluid lubricates articular cartilage and provides nourishment through diffusion. It made from a ultrafiltrate of blood plasma, produced and regulated by the synovium.<ref name=":0">Orthobullets [https://www.orthobullets.com/basic-science/9018/synovium-and-synovial-fluid Synovium] Available from:https://www.orthobullets.com/basic-science/9018/synovium-and-synovial-fluid (accessed 18.6.2021)</ref> | # Synovial fluid lubricates articular cartilage and provides nourishment through diffusion. It made from a ultrafiltrate of [[blood]] plasma, produced and regulated by the synovium.<ref name=":0">Orthobullets [https://www.orthobullets.com/basic-science/9018/synovium-and-synovial-fluid Synovium] Available from:https://www.orthobullets.com/basic-science/9018/synovium-and-synovial-fluid (accessed 18.6.2021)</ref> | ||
== Anatomy == | == Anatomy == | ||
| Line 21: | Line 21: | ||
Intimal layer: | Intimal layer: | ||
* Well innervated and vascularised containing different types of cells including fibroblasts, macrophages, adipocytes, nerve fibres, vascular endothelial cells as well as lymphocytes. | * Well innervated and vascularised containing different types of cells including fibroblasts, [[macrophages]], adipocytes, [[Neurone|nerve]] fibres, vascular endothelial cells as well as [[lymphocytes]]. | ||
* Features two types of synoviocytes: type A - derived from macrophages; non-fixed cells with antigen presenting ability located in superficial layer; important in phagocytosis and fibroblastic. Type B cells - fibroblast like cells; rich rough endoplasmic reticulum and dendritic processes that reach out to the joint surface; located at various depths, frequently in deeper layer; produce synovial fluid<ref name=":0" />. | * Features two types of synoviocytes: type A - derived from macrophages; non-fixed cells with antigen presenting ability located in superficial layer; important in phagocytosis and fibroblastic. Type B cells - fibroblast like cells; rich rough endoplasmic reticulum and dendritic processes that reach out to the joint surface; located at various depths, frequently in deeper layer; produce synovial fluid<ref name=":0" />. | ||
Subintima layer | Subintima layer | ||
* Thicker layer of loose connective tissue which contains fewer cells | * Thicker layer of loose [[Connective Tissue Disorders|connective tissue]] which contains fewer cells | ||
* Composed of fatty, fibrous or loose areolar tissue.<ref name=":1">Radiopedia Synovium Available from:https://radiopaedia.org/articles/synovium?lang=gb (accessed 18.6.2021)</ref> | * Composed of fatty, fibrous or loose areolar tissue.<ref name=":1">Radiopedia Synovium Available from:https://radiopaedia.org/articles/synovium?lang=gb (accessed 18.6.2021)</ref> | ||
* Able to reshape itself to avoid any collision between the muscles and acting as the line-up between the bursae, tendon sheaths, and joints<ref name=":2">Go medii Synovium Available:https://gomedii.com/blogs/english/health-a2z/synovial-membrane-structure-functions-and-pathology/ (accessed 18.6.2021)</ref>. | * Able to reshape itself to avoid any collision between the [[Muscle|muscles]] and acting as the line-up between the bursae, [[Tendon Anatomy|tendon]] sheaths, and joints<ref name=":2">Go medii Synovium Available:https://gomedii.com/blogs/english/health-a2z/synovial-membrane-structure-functions-and-pathology/ (accessed 18.6.2021)</ref>. | ||
In addition, the type B cells possess some mesenchymal stem cell properties and can be used as source cells for cartilage repair<ref name=":3" />. | In addition, the type B cells possess some mesenchymal stem cell properties and can be used as source cells for cartilage repair<ref name=":3" />. | ||
== Synovial Fluid == | == Synovial Fluid == | ||
[[File:Joint Hydration Supplement.jpeg|right|frameless]] | [[File:Joint Hydration Supplement.jpeg|right|frameless]] | ||
This fluid is generated from an ultrafiltrate of [[Blood Physiology|blood]] plasma which is regulated by synovium. The purpose of this fluid is to lubricate the cartilage of the bone joint and provide nourishment through diffusion. It is made from a ultrafiltrate of blood plasma and is regulated by the synovium. eg healthy knee contains ~2mL of synovial fluid. | This fluid is generated from an ultrafiltrate of [[Blood Physiology|blood]] plasma which is regulated by synovium. The purpose of this fluid is to lubricate the cartilage of the bone joint and provide nourishment through diffusion. It is made from a ultrafiltrate of blood plasma and is regulated by the synovium. eg healthy [[Knee Bursitis|knee]] contains ~2mL of synovial fluid. | ||
Consists of: | Consists of: | ||
| Line 43: | Line 43: | ||
* Prostaglandins: produced in nearly all cells and are part of the body's way of dealing with injury and illness.. They both sustain homeostatic functions and mediate pathogenic mechanisms, including the [[Inflammation Acute and Chronic|inflammatory]] response<ref>Ricciotti E, FitzGerald GA. Prostaglandins and inflammation. Arteriosclerosis, thrombosis, and vascular biology. 2011 May;31(5):986-1000.Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3081099/ (accessed 18.6.2021)</ref>. | * Prostaglandins: produced in nearly all cells and are part of the body's way of dealing with injury and illness.. They both sustain homeostatic functions and mediate pathogenic mechanisms, including the [[Inflammation Acute and Chronic|inflammatory]] response<ref>Ricciotti E, FitzGerald GA. Prostaglandins and inflammation. Arteriosclerosis, thrombosis, and vascular biology. 2011 May;31(5):986-1000.Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3081099/ (accessed 18.6.2021)</ref>. | ||
Biomechanics: | [[Biomechanics]]: | ||
* Synovial fluid exhibits non-Newtonian flow characteristics ie Viscosity coefficient is not a constant; Fluid is not linearly viscous; Viscosity increases as the [[shear]] rate decreases).<ref name=":0" /> | * Synovial fluid exhibits non-Newtonian flow characteristics ie Viscosity coefficient is not a constant; Fluid is not linearly viscous; Viscosity increases as the [[shear]] rate decreases).<ref name=":0" /> | ||
| Line 49: | Line 49: | ||
== Radiographic features == | == Radiographic features == | ||
The synovium will be mostly imaged and assessed with MRI and ultrasound in the setting of inflammatory conditions such as arthritis, tenosynovitis and bursitis in which it becomes thickened and increased amounts of synovial fluid will be present. | The synovium will be mostly imaged and assessed with [[MRI Scans|MRI]] and [[Ultrasound Scans|ultrasound]] in the setting of inflammatory conditions such as [[arthritis]], tenosynovitis and [[bursitis]] in which it becomes thickened and increased amounts of synovial fluid will be present. | ||
== Related pathology == | == Related pathology == | ||
| Line 58: | Line 58: | ||
* Synovitis | * Synovitis | ||
* Osteoarthritis | * Osteoarthritis | ||
* Rheumatoid arthritis, juvenile idiopathic arthritis, septic arthritis | * [[Rheumatoid Arthritis|Rheumatoid arthritis]], juvenile idiopathic arthritis, [[Septic (Infectious) Arthritis|septic arthritis]] | ||
* Crystal deposition disease | * Crystal deposition disease | ||
* Synovial sarcoma | * Synovial sarcoma | ||
| Line 64: | Line 64: | ||
== Resources == | == Resources == | ||
== References == | == References == | ||
Revision as of 11:37, 18 June 2021
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (18/06/2021)
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Kim Jackson and Kirenga Bamurange Liliane
Introduction[edit | edit source]
The synovial membrane is soft and thin membrane yet has various significant roles that are very essentials for our body movements that are dependent on the synovium joints.
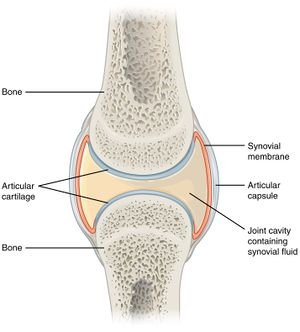
- Synovium (also called the synovial membrane) is a specialized connective soft-tissue membrane that lines the inner surface of synovial joint capsules. Together with bone, articular cartilage, tendon, ligament, and fibrous capsule, it is an important component of the tissues that form an integrated joint. As such, it not only has its own specific functions but also interacts with other tissues in the joint both structurally and functionally[1].
- Synovial fluid lubricates articular cartilage and provides nourishment through diffusion. It made from a ultrafiltrate of blood plasma, produced and regulated by the synovium.[2]
Anatomy[edit | edit source]
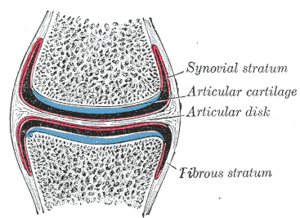
Image 2: Synovial membrane showing the fibrous and the intimal layer.
The synovial membrane consists of an
Intimal layer:
- Well innervated and vascularised containing different types of cells including fibroblasts, macrophages, adipocytes, nerve fibres, vascular endothelial cells as well as lymphocytes.
- Features two types of synoviocytes: type A - derived from macrophages; non-fixed cells with antigen presenting ability located in superficial layer; important in phagocytosis and fibroblastic. Type B cells - fibroblast like cells; rich rough endoplasmic reticulum and dendritic processes that reach out to the joint surface; located at various depths, frequently in deeper layer; produce synovial fluid[2].
Subintima layer
- Thicker layer of loose connective tissue which contains fewer cells
- Composed of fatty, fibrous or loose areolar tissue.[3]
- Able to reshape itself to avoid any collision between the muscles and acting as the line-up between the bursae, tendon sheaths, and joints[4].
In addition, the type B cells possess some mesenchymal stem cell properties and can be used as source cells for cartilage repair[1].
Synovial Fluid[edit | edit source]
This fluid is generated from an ultrafiltrate of blood plasma which is regulated by synovium. The purpose of this fluid is to lubricate the cartilage of the bone joint and provide nourishment through diffusion. It is made from a ultrafiltrate of blood plasma and is regulated by the synovium. eg healthy knee contains ~2mL of synovial fluid.
Consists of:
- Hyaluronic acid: a viscous glycosaminoglycan serves as a structural element and lubricant.[5] Image 3: A joint hydration supplement that uses hyaluronic acid
- Lubricin: the most lubricating and anti-ahesive molecule in the human body. It is a surface-active mucinous glycoprotein secreted in the synovial joint and plays an important role in cartilage integrity. Lubricin molecules coat the cartilage surface, providing boundary lubrication and preventing cell and protein adhesion[6]
- Proteinase: an enzyme that catalyzes proteolysis, the breakdown of proteins into smaller polypeptides or single amino acids.
- Collagenases: enzymes that break the peptide bonds in collagen.
- Prostaglandins: produced in nearly all cells and are part of the body's way of dealing with injury and illness.. They both sustain homeostatic functions and mediate pathogenic mechanisms, including the inflammatory response[7].
- Synovial fluid exhibits non-Newtonian flow characteristics ie Viscosity coefficient is not a constant; Fluid is not linearly viscous; Viscosity increases as the shear rate decreases).[2]
In case of joint inflammation, swelling or redness, a synovial fluid analysis may be done. This sample is used to detect any traces of lactic dehydrogenase, uric acid, and protein which can be held responsible for inflammation[4].
Radiographic features[edit | edit source]
The synovium will be mostly imaged and assessed with MRI and ultrasound in the setting of inflammatory conditions such as arthritis, tenosynovitis and bursitis in which it becomes thickened and increased amounts of synovial fluid will be present.
Related pathology[edit | edit source]
Communication between synovium and structural tissues including cartilage, bone, capsule, and ligaments is important for maintaining normal joint physiology, but also contributes to several joint disease processes.
There are risk factors, conditions, and diseases that are evolved in situations when the membrane is irritated or thickened. Some conditions and disease are enlisted below.
- Synovitis
- Osteoarthritis
- Rheumatoid arthritis, juvenile idiopathic arthritis, septic arthritis
- Crystal deposition disease
- Synovial sarcoma
- Synovial hyperplasia[3]
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Musculoskeletal Key Synovium Available: https://musculoskeletalkey.com/synovium-and-joint-biology/(accessed 18.6.2021)
- ↑ 2.0 2.1 2.2 Orthobullets Synovium Available from:https://www.orthobullets.com/basic-science/9018/synovium-and-synovial-fluid (accessed 18.6.2021)
- ↑ 3.0 3.1 Radiopedia Synovium Available from:https://radiopaedia.org/articles/synovium?lang=gb (accessed 18.6.2021)
- ↑ 4.0 4.1 Go medii Synovium Available:https://gomedii.com/blogs/english/health-a2z/synovial-membrane-structure-functions-and-pathology/ (accessed 18.6.2021)
- ↑ MW dictionary hyaluronic acid Available: https://www.merriam-webster.com/dictionary/hyaluronic%20acid (accessed 18.6.2021)
- ↑ Jay GD, Waller KA. The biology of lubricin: near frictionless joint motion. Matrix Biology. 2014 Oct 1;39:17-24.Available:https://www.sciencedirect.com/science/article/pii/S0945053X14001619 (accessed 18.6.2021)
- ↑ Ricciotti E, FitzGerald GA. Prostaglandins and inflammation. Arteriosclerosis, thrombosis, and vascular biology. 2011 May;31(5):986-1000.Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3081099/ (accessed 18.6.2021)