Kyphoplasty: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Removed case study) |
||
| (24 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- | '''Original Editor '''- [[User:Margaret Chislett|Margaret Chislett]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
''' | </div> | ||
</div> | == Introduction == | ||
== | [[File:Bianca-jordan-IPjWtxPJUQc-unsplash.jpg|thumb|282x282px]] | ||
Kyphoplasty KP is a relatively new procedure that was first performed in California in 1998. <ref>Wong X, Reiley MA, Garfin S. Vertebroplasty/Kyphoplasty. J women’s imaging 2000;2: 117-24</ref> It is a minimally invasive percutaneous procedure that involves the insertion of an inflatable bone tamp into the [[Fracture|fractured]] vertebral body under [http://emedicine.medscape.com/article/325872-media fluoroscopic guidance]<ref name=":0">Heini PF, Orler R. Kyphoplasty for treatment of osteoporotic vertebral fractures. European spine journal. 2004 May 1;13(3):184-92.</ref>. The [[bone]] tamp is then inflated, elevating the endplates and restoring the vertebral body toward its original height<ref name=":0" />. The procedure has been shown to speed up the treatment and recovery period of vertebral compression fractures<ref>Pflugmacher R, Kandziora F, Schroeder RJ, Melcher I, Haas NP, Klostermann CK. Percutaneous balloon kyphoplasty in the treatment of pathological vertebral body fracture and deformity in multiple myeloma: a one-year follow-up. Acta Radiologica. 2006 Jan 1;47(4):369-76.</ref>. It has the added benefit of addressing [[Thoracic Hyperkyphosis|kyphotic deformity]] as well as pain<ref name=":6">Papanastassiou ID, Phillips FM, Van Meirhaeghe J, Berenson JR, Andersson GB, Chung G, Small BJ, Aghayev K, Vrionis FD. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3459114/ Comparing effects of kyphoplasty, vertebroplasty, and non-surgical management in a systematic review of randomized and non-randomized controlled studies]. European Spine Journal. 2012 Sep 1;21(9):1826-43.</ref>, unlike vertebroplasty that only addresses pain.<ref name=":2">Garfin S, Bono C. Kyphoplasty and Vertebroplasty for the Treatment of Painful Osteoporotic Vertebral Compression Fractures. In Advances in Spinal Fusion 2003 Oct 21 (pp. 43-60). CRC Press.</ref> Indications for kyphoplasty include painful or progressive [[Osteoporosis|osteoporotic]] and osteolytic vertebral compression fractures that do not compromise the [[Spinal cord anatomy|spinal canal]] based on the level of pain and the percentage of vertebral collapse<ref name=":2" /><ref name=":3">Hardouin, P., Fayada, P., Leclet, H., & Chopin, D. (2002). ''Kyphoplasty. Joint Bone Spine, 69(3), 256–261.''</ref>. If a patient rates his/her [[Pain Assessment|pain]] as being greater than 5 out of 10<ref>Röllinghoff, M., Zarghooni, K., Schlüter-Brust, K., Sobottke, R., Schlegel, U., Eysel, P., & Delank, K.-S. (2010). ''Indications and contraindications for vertebroplasty and kyphoplasty. Archives of Orthopaedic and Trauma Surgery, 130(6), 765–774.''</ref> (when 10 equals worst pain imaginable and 0 equals no pain) or the vertebral bodies are collapsed more than 40%, then kyphoplasty or vertebroplasty is indicated as an initial intervention.<ref name="null" /> Conservative treatment has been questioned as it can take months to resolve and requires an extended period of rest which can lead to a further decrease in bone density.<ref name=":0" /> In most cases, kyphoplasty can eliminate the need for complex surgical fixation<ref>Hsieh PC, Koski TR, Sciubba DM, Moller DJ, O'shaughnessy BA, Li KW, Gokaslan ZL, Ondra SL, Fessler RG, Liu JC. Maximizing the potential of minimally invasive spine surgery in complex spinal disorders. Neurosurgical focus. 2008 Aug 1;25(2):E19.</ref>, especially where the bones are osteoporotic. However, if there is compromise neurological compromise kyphoplasty is not indicated.<ref name=":0" /> | |||
Kyphoplasty is a | |||
Indications for kyphoplasty include painful or progressive osteoporotic and osteolytic vertebral compression fractures that do not compromise the spinal canal | |||
< | |||
== Procedure == | |||
Unlike vertebroplasty VP, a balloon is inserted percutaneously into the vertebral body and inflated before the thick polymethylmethacrylate (PMMA) is injected in under low pressure into the cavity of the body<ref name=":3" />. The bone tamp is then deflated and removed. Kyphoplasty has been shown to provide significant pain relief as well as a substantial improvement in the height of the collapsed vertebral body and has been found to reduce the spinal kyphosis<ref name="null">EMedicine Nonop treatment of vertebral compression fractures.http://emedicine.medscape.com/article/325872-treatment#TreatmentOtherTreatment</ref>.This video below shows the difference between the KP and VP. | |||
{{#ev:youtube|_lUhQLFHriw|300}}<ref>Fortis Healthcare. Vertebroplasty & Kyphoplasty ( Spine Surgery) Neuro Surgery; Fortis Healthcare,India. Available from: http://www.youtube.com/watch?v=_lUhQLFHriw[last accessed 25/6/2009]</ref> | |||
== Clinical Presentation == | == Clinical Presentation == | ||
[[File:Vertebral augmentation.png|thumb|235x235px|x-ray after injecting the PMMA]]The onset of sudden, severe back pain, that worsens on standing or walking but relieves when lying down can often be mistaken for [[muscle]] strain but if there is a loss of movement and pain when bending or twisting coupled with a loss of height, deformity of the spine - "hunchback" shape then a fracture may be suspected. In most cases the mechanism of injury is the same as a back strain and can be caused by doing every day tasks such as lifting, bending to pick something up from the floor, or a simple slip or missing a step. Another warning sign that it could be something more serious is the age of the client, people over the age of 50 and in particular women are at risk of osteoporosis and therefore more susceptible to a serious injury like a [[fracture]].<ref>WebMD,Symptoms of Compression fracture;http://www.webmd.com/osteoporosis/guide/spinal-compression-fractures-symptoms</ref> | |||
== Diagnostic Tests == | == Diagnostic Tests == | ||
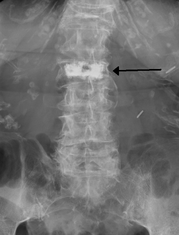
[[File:L4 compression fracture.jpg|thumb|265x265px|compression fracture]] | |||
It is important to correctly assess a patient who presents with spinal pain of traumatic or atraumatic origin that is not responding to conservative treatment, particularly if the patient falls under the risk category for osteoporosis. The most common tests are: | |||
Radiography | * Radiography - [[X-Rays|X-rays]] are usually the first diagnostic test performed as they are inexpensive. A lateral X-ray of the [[Thoracic Anatomy|thoracic]] or [[Lumbar Anatomy|lumbar spine]] can often identify a fracture and reveal any loss of height or misalignment of the spine.<ref name=":1">McGirt, M., & Wong. (2013). ''Vertebral compression fractures: a review of current management and multimodal therapy. Journal of Multidisciplinary Healthcare, 205.''</ref> | ||
* [[CT Scans|Computed Tomography (CT) scan]] - provides greater detail of bony anatomy and can reveal loss of height, fragment retropulsion, and any compromise of the spinal<ref name=":1" /> | |||
* [[MRI Scans|Magnetic Resonance Imaging (MRI)]] - This is more expensive but can reveal whether the fracture is acute (by the presence of bony oedema) and also if there is compromise of the neurological system.<ref name=":1" /> | |||
* Bone Scintigraphy - a nuclear medicine imaging technique of the bone that is used to diagnose bone conditions and disorders such as fracture, infection, and cancer<ref>Van den Wyngaert, T., Strobel, K., Kampen, W. U., Kuwert, T., van der Bruggen, W., … Paycha, F. (2016). ''The EANM practice guidelines for bone scintigraphy. European Journal of Nuclear Medicine and Molecular Imaging, 43(9), 1723–1738.''</ref> | |||
== | == Complications == | ||
Kyphoplasty is the least invasive intervention that is effective in the treatment of VCF that didn't respond to conservative intervention, it shows a rapid pain relief<ref name=":7">Yaltirik K, Ashour AM, Reis CR, Özdoğan S, Atalay B. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4994147/#ref19 Vertebral augmentation by kyphoplasty and vertebroplasty: 8 years experience outcomes and complications]. Journal of craniovertebral junction & spine. 2016 Jul;7(3):153.</ref> and improvement in pain on VAS, quality of life, and pulmonary function<ref name=":8">Robinson Y, Tschöke SK, Stahel PF, Kayser R, Heyde CE. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2248169/ Complications and safety aspects of kyphoplasty for osteoporotic vertebral fractures: a prospective follow-up study in 102 consecutive patients]. Patient Safety in Surgery. 2008 Dec 1;2(1):2.</ref>. | |||
Despite it is minimally invasive technique but still has complications<ref name=":7" /><ref name=":8" /> and these complications should be taken into consideration | |||
* Extravertebral leakage of the cement, the leakage may happen through the cracks of the vertebrae. this leakage of cement may into the spinal canal causing spinal canal stenosis which isn't common to happen and less common on kyphoplasty than vertebroplasty<ref>Zhao G, Liu X, Li F. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6196425/ Balloon kyphoplasty versus percutaneous vertebroplasty for treatment of osteoporotic vertebral compression fractures (OVCFs)]. Osteoporosis International. 2016 Sep 1;27(9):2823-34.</ref><ref name=":6" /> or may cause pulmonary embolism that rarely requires immediate intervention its symptoms vary from mild dyspnoea which is usually asymptomatic to serious symptomatic complications that will need urgent surgery to remove the cement. Cement leakage is less common in kyphoplasty about 9% than in vertebroplasty about 41%. | |||
* Secondary fracture to the vertebrae above and below and maybe secondary due to the leakage of cement in the intervertebral disc, secondary most common in kyphoplasty. | |||
* It has a higher risk of cardiac mortality than vertebroplasty<ref name=":8" />. | |||
* Infected spondylitis with epidural abscess at the operated vertebrae site. | |||
* Superficial wound infection as in any surgical intervention was reported in a study within 1 0 days after KP. | |||
== | == Physiotherapy Management == | ||
Physiotherapy is indicated both pre and post-op. Prior to kyphoplasty the emphasis is on pain relief and preventing secondary complications such as progressive immobility and weakness. The following interventions are recommended for pain relief prior to the procedure: | |||
* Analgesic medication | |||
* Heat | |||
* Massage | |||
* Gentle exercises and advice on activities of daily living | |||
* Rest | |||
Physiotherapists should also give advice to prevent further injury, especially when recommending exercises. Patients should be advised to avoid flexion exercises such as crunches and situps<ref name=":1" />. However, Axial back extension strengthening exercises should be included in the programme, in accordance with the patient's pain tolerance<ref name=":1" />. Weight bearing exercises should be included to minimize the effects of osteoporosis, however, [[Aquatherapy|aquatic exercises]]<ref>Devereux K, Robertson D and Briffa NK: Effects of a water-based program on women 65 years and over: A randomised controlled trial. Australian Journal of Physiotherapy 2005; 51: 102–108</ref> and balance training are also beneficial<ref>Koichi K, Daisuke S, Hitoshi W, Atsuko H, and Takeo N; A Comparison of the Effects of Different Water Exercise Programs on Balance Ability in Elderly People, Journal of Aging and Physical Activity, 2008, 16, 381-392</ref>. | |||
Any patient with diagnosed osteopenia or osteoporosis should be on anti-osteoporotic medications, including second-generation bisphosphonates, as well as (daily) with 1500 mg of elemental calcium and 400 IU of vitamin D. | |||
Most Kyphoplasty procedures are performed on an outpatient basis unless the patient has comorbidities requiring a short inpatient stay. Post-op treatment should be geared towards home safety training if the patient is at high risk for fall ([[Berg Balance Scale]]>40), pain management, and transfer training. Rehabilitation at this stage should focus not only on recovery but must also prevention. The following modalities should be included in the programme with a gradual increase in intensity depending on the patient's tolerance. | |||
* Strengthening Exercises - particularly of the back extensors can assist not only with pain management and with improving posture | |||
* Weightbearing Exercises - should be included into the programme as mechanical loading will stimulate osteogenesis (Wolff’s law)<ref>Chen JH, Liu C, You L, Simmons CA. Boning up on Wolff’s Law: mechanical regulation of the cells that make and maintain bone. J Biomech. 2010; 43(1):108–18</ref>, improving bone quality and reducing the risk of (or worsening) osteoporosis. | |||
* Stretching - Care needs to be taken not to overstretch, especially spinal flexion, as this may alter the protective mechanisms against back pain.<ref>Sinaki M. Yoga spinal flexion positions and vertebral compression fracture in osteopenia or osteoporosis of spine: case series. Pain Pract. 2013;13(1):68–75</ref> | |||
* Pain Management - advice on the use of heat and ice | |||
* Advice and transfer practice - teaching the client how to move from one position to another may help to minimise unnecessary load on the spine | |||
* Manual handling training and activities of daily living - correct techniques on lifting and daily tasks can help reduce the load on the spine and other joints | |||
* Balance and Proprioception Training - This is especially beneficial for clients who are at risk of falling | |||
* Posture Re-education - adopting correct posture at rest and when active can help to reduce the stress on the spine, muscles, and ligaments. | |||
At each step of the programme the patient should be treated like an individual and their level of pain, function and lifestyle should be taken into account. Close monitoring is necessary to ensure that the programme is progressed in accordance with the patient's status and needs. | |||
== Outcome Measures == | |||
[[Outcome Measures|Outcome measures]] can help assess a patient's current status and function and monitor their progress. Below are some of the most common used to determine the need for this procedure and also to predict and review outcomes of the surgery and subsequent interventions. | |||
= | * [[Visual Analogue Scale|Pain Visual Analogue Scale (VAS)]]<ref name=":4">Kasperk, C., Grafe, I. A., Schmitt, S., Nöldge, G., Weiss, C., Da Fonseca, K., … Nawroth, P. (2010). ''Three-year Outcomes after Kyphoplasty in Patients with Osteoporosis with Painful Vertebral Fractures. Journal of Vascular and Interventional Radiology, 21(5), 701–709''</ref> - Measures Pain intensity | ||
< | * European Vertebral Osteoporosis Study Questionnaire (EVOS)<ref name=":4" /> - Measures health impact, back pain and functional capacity of vertebral compression fractures<ref name=":5">Schoenfeld, A. J., & Bono, C. M. (2011). ''Measuring spine fracture outcomes: Common scales and checklists. Injury, 42(3), 265–270.''</ref> | ||
* [[Oswestry Disability Index|Oswestry Disability Index (ODI)]] - Measures back function, physical ability, mobility, pain, sexual function<ref name=":5" /> | |||
</ | * [[36-Item Short Form Survey (SF-36)|Short Form Survvey (SF-36)]] -Measures Overall quality of health: (including physical and mental health)<ref name=":5" /> | ||
* [[Rolland‐Morris Disability Questionnaire|Roland Morris Disability Questionnaire (RMDQ]]) - Measures back function, physical ability, mobility, pain<ref name=":5" /> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Fractures]] | |||
[[Category:Older People/Geriatrics]] | |||
Latest revision as of 01:11, 29 June 2020
Original Editor - Margaret Chislett Top Contributors - Margaret Chislett, Kim Jackson, Admin, Khloud Shreif, 127.0.0.1 and WikiSysop
Introduction[edit | edit source]
Kyphoplasty KP is a relatively new procedure that was first performed in California in 1998. [1] It is a minimally invasive percutaneous procedure that involves the insertion of an inflatable bone tamp into the fractured vertebral body under fluoroscopic guidance[2]. The bone tamp is then inflated, elevating the endplates and restoring the vertebral body toward its original height[2]. The procedure has been shown to speed up the treatment and recovery period of vertebral compression fractures[3]. It has the added benefit of addressing kyphotic deformity as well as pain[4], unlike vertebroplasty that only addresses pain.[5] Indications for kyphoplasty include painful or progressive osteoporotic and osteolytic vertebral compression fractures that do not compromise the spinal canal based on the level of pain and the percentage of vertebral collapse[5][6]. If a patient rates his/her pain as being greater than 5 out of 10[7] (when 10 equals worst pain imaginable and 0 equals no pain) or the vertebral bodies are collapsed more than 40%, then kyphoplasty or vertebroplasty is indicated as an initial intervention.[8] Conservative treatment has been questioned as it can take months to resolve and requires an extended period of rest which can lead to a further decrease in bone density.[2] In most cases, kyphoplasty can eliminate the need for complex surgical fixation[9], especially where the bones are osteoporotic. However, if there is compromise neurological compromise kyphoplasty is not indicated.[2]
Procedure[edit | edit source]
Unlike vertebroplasty VP, a balloon is inserted percutaneously into the vertebral body and inflated before the thick polymethylmethacrylate (PMMA) is injected in under low pressure into the cavity of the body[6]. The bone tamp is then deflated and removed. Kyphoplasty has been shown to provide significant pain relief as well as a substantial improvement in the height of the collapsed vertebral body and has been found to reduce the spinal kyphosis[8].This video below shows the difference between the KP and VP.
Clinical Presentation[edit | edit source]
The onset of sudden, severe back pain, that worsens on standing or walking but relieves when lying down can often be mistaken for muscle strain but if there is a loss of movement and pain when bending or twisting coupled with a loss of height, deformity of the spine - "hunchback" shape then a fracture may be suspected. In most cases the mechanism of injury is the same as a back strain and can be caused by doing every day tasks such as lifting, bending to pick something up from the floor, or a simple slip or missing a step. Another warning sign that it could be something more serious is the age of the client, people over the age of 50 and in particular women are at risk of osteoporosis and therefore more susceptible to a serious injury like a fracture.[11]
Diagnostic Tests[edit | edit source]
It is important to correctly assess a patient who presents with spinal pain of traumatic or atraumatic origin that is not responding to conservative treatment, particularly if the patient falls under the risk category for osteoporosis. The most common tests are:
- Radiography - X-rays are usually the first diagnostic test performed as they are inexpensive. A lateral X-ray of the thoracic or lumbar spine can often identify a fracture and reveal any loss of height or misalignment of the spine.[12]
- Computed Tomography (CT) scan - provides greater detail of bony anatomy and can reveal loss of height, fragment retropulsion, and any compromise of the spinal[12]
- Magnetic Resonance Imaging (MRI) - This is more expensive but can reveal whether the fracture is acute (by the presence of bony oedema) and also if there is compromise of the neurological system.[12]
- Bone Scintigraphy - a nuclear medicine imaging technique of the bone that is used to diagnose bone conditions and disorders such as fracture, infection, and cancer[13]
Complications[edit | edit source]
Kyphoplasty is the least invasive intervention that is effective in the treatment of VCF that didn't respond to conservative intervention, it shows a rapid pain relief[14] and improvement in pain on VAS, quality of life, and pulmonary function[15].
Despite it is minimally invasive technique but still has complications[14][15] and these complications should be taken into consideration
- Extravertebral leakage of the cement, the leakage may happen through the cracks of the vertebrae. this leakage of cement may into the spinal canal causing spinal canal stenosis which isn't common to happen and less common on kyphoplasty than vertebroplasty[16][4] or may cause pulmonary embolism that rarely requires immediate intervention its symptoms vary from mild dyspnoea which is usually asymptomatic to serious symptomatic complications that will need urgent surgery to remove the cement. Cement leakage is less common in kyphoplasty about 9% than in vertebroplasty about 41%.
- Secondary fracture to the vertebrae above and below and maybe secondary due to the leakage of cement in the intervertebral disc, secondary most common in kyphoplasty.
- It has a higher risk of cardiac mortality than vertebroplasty[15].
- Infected spondylitis with epidural abscess at the operated vertebrae site.
- Superficial wound infection as in any surgical intervention was reported in a study within 1 0 days after KP.
Physiotherapy Management[edit | edit source]
Physiotherapy is indicated both pre and post-op. Prior to kyphoplasty the emphasis is on pain relief and preventing secondary complications such as progressive immobility and weakness. The following interventions are recommended for pain relief prior to the procedure:
- Analgesic medication
- Heat
- Massage
- Gentle exercises and advice on activities of daily living
- Rest
Physiotherapists should also give advice to prevent further injury, especially when recommending exercises. Patients should be advised to avoid flexion exercises such as crunches and situps[12]. However, Axial back extension strengthening exercises should be included in the programme, in accordance with the patient's pain tolerance[12]. Weight bearing exercises should be included to minimize the effects of osteoporosis, however, aquatic exercises[17] and balance training are also beneficial[18].
Any patient with diagnosed osteopenia or osteoporosis should be on anti-osteoporotic medications, including second-generation bisphosphonates, as well as (daily) with 1500 mg of elemental calcium and 400 IU of vitamin D.
Most Kyphoplasty procedures are performed on an outpatient basis unless the patient has comorbidities requiring a short inpatient stay. Post-op treatment should be geared towards home safety training if the patient is at high risk for fall (Berg Balance Scale>40), pain management, and transfer training. Rehabilitation at this stage should focus not only on recovery but must also prevention. The following modalities should be included in the programme with a gradual increase in intensity depending on the patient's tolerance.
- Strengthening Exercises - particularly of the back extensors can assist not only with pain management and with improving posture
- Weightbearing Exercises - should be included into the programme as mechanical loading will stimulate osteogenesis (Wolff’s law)[19], improving bone quality and reducing the risk of (or worsening) osteoporosis.
- Stretching - Care needs to be taken not to overstretch, especially spinal flexion, as this may alter the protective mechanisms against back pain.[20]
- Pain Management - advice on the use of heat and ice
- Advice and transfer practice - teaching the client how to move from one position to another may help to minimise unnecessary load on the spine
- Manual handling training and activities of daily living - correct techniques on lifting and daily tasks can help reduce the load on the spine and other joints
- Balance and Proprioception Training - This is especially beneficial for clients who are at risk of falling
- Posture Re-education - adopting correct posture at rest and when active can help to reduce the stress on the spine, muscles, and ligaments.
At each step of the programme the patient should be treated like an individual and their level of pain, function and lifestyle should be taken into account. Close monitoring is necessary to ensure that the programme is progressed in accordance with the patient's status and needs.
Outcome Measures[edit | edit source]
Outcome measures can help assess a patient's current status and function and monitor their progress. Below are some of the most common used to determine the need for this procedure and also to predict and review outcomes of the surgery and subsequent interventions.
- Pain Visual Analogue Scale (VAS)[21] - Measures Pain intensity
- European Vertebral Osteoporosis Study Questionnaire (EVOS)[21] - Measures health impact, back pain and functional capacity of vertebral compression fractures[22]
- Oswestry Disability Index (ODI) - Measures back function, physical ability, mobility, pain, sexual function[22]
- Short Form Survvey (SF-36) -Measures Overall quality of health: (including physical and mental health)[22]
- Roland Morris Disability Questionnaire (RMDQ) - Measures back function, physical ability, mobility, pain[22]
References[edit | edit source]
- ↑ Wong X, Reiley MA, Garfin S. Vertebroplasty/Kyphoplasty. J women’s imaging 2000;2: 117-24
- ↑ 2.0 2.1 2.2 2.3 Heini PF, Orler R. Kyphoplasty for treatment of osteoporotic vertebral fractures. European spine journal. 2004 May 1;13(3):184-92.
- ↑ Pflugmacher R, Kandziora F, Schroeder RJ, Melcher I, Haas NP, Klostermann CK. Percutaneous balloon kyphoplasty in the treatment of pathological vertebral body fracture and deformity in multiple myeloma: a one-year follow-up. Acta Radiologica. 2006 Jan 1;47(4):369-76.
- ↑ 4.0 4.1 Papanastassiou ID, Phillips FM, Van Meirhaeghe J, Berenson JR, Andersson GB, Chung G, Small BJ, Aghayev K, Vrionis FD. Comparing effects of kyphoplasty, vertebroplasty, and non-surgical management in a systematic review of randomized and non-randomized controlled studies. European Spine Journal. 2012 Sep 1;21(9):1826-43.
- ↑ 5.0 5.1 Garfin S, Bono C. Kyphoplasty and Vertebroplasty for the Treatment of Painful Osteoporotic Vertebral Compression Fractures. In Advances in Spinal Fusion 2003 Oct 21 (pp. 43-60). CRC Press.
- ↑ 6.0 6.1 Hardouin, P., Fayada, P., Leclet, H., & Chopin, D. (2002). Kyphoplasty. Joint Bone Spine, 69(3), 256–261.
- ↑ Röllinghoff, M., Zarghooni, K., Schlüter-Brust, K., Sobottke, R., Schlegel, U., Eysel, P., & Delank, K.-S. (2010). Indications and contraindications for vertebroplasty and kyphoplasty. Archives of Orthopaedic and Trauma Surgery, 130(6), 765–774.
- ↑ 8.0 8.1 EMedicine Nonop treatment of vertebral compression fractures.http://emedicine.medscape.com/article/325872-treatment#TreatmentOtherTreatment
- ↑ Hsieh PC, Koski TR, Sciubba DM, Moller DJ, O'shaughnessy BA, Li KW, Gokaslan ZL, Ondra SL, Fessler RG, Liu JC. Maximizing the potential of minimally invasive spine surgery in complex spinal disorders. Neurosurgical focus. 2008 Aug 1;25(2):E19.
- ↑ Fortis Healthcare. Vertebroplasty & Kyphoplasty ( Spine Surgery) Neuro Surgery; Fortis Healthcare,India. Available from: http://www.youtube.com/watch?v=_lUhQLFHriw[last accessed 25/6/2009]
- ↑ WebMD,Symptoms of Compression fracture;http://www.webmd.com/osteoporosis/guide/spinal-compression-fractures-symptoms
- ↑ 12.0 12.1 12.2 12.3 12.4 McGirt, M., & Wong. (2013). Vertebral compression fractures: a review of current management and multimodal therapy. Journal of Multidisciplinary Healthcare, 205.
- ↑ Van den Wyngaert, T., Strobel, K., Kampen, W. U., Kuwert, T., van der Bruggen, W., … Paycha, F. (2016). The EANM practice guidelines for bone scintigraphy. European Journal of Nuclear Medicine and Molecular Imaging, 43(9), 1723–1738.
- ↑ 14.0 14.1 Yaltirik K, Ashour AM, Reis CR, Özdoğan S, Atalay B. Vertebral augmentation by kyphoplasty and vertebroplasty: 8 years experience outcomes and complications. Journal of craniovertebral junction & spine. 2016 Jul;7(3):153.
- ↑ 15.0 15.1 15.2 Robinson Y, Tschöke SK, Stahel PF, Kayser R, Heyde CE. Complications and safety aspects of kyphoplasty for osteoporotic vertebral fractures: a prospective follow-up study in 102 consecutive patients. Patient Safety in Surgery. 2008 Dec 1;2(1):2.
- ↑ Zhao G, Liu X, Li F. Balloon kyphoplasty versus percutaneous vertebroplasty for treatment of osteoporotic vertebral compression fractures (OVCFs). Osteoporosis International. 2016 Sep 1;27(9):2823-34.
- ↑ Devereux K, Robertson D and Briffa NK: Effects of a water-based program on women 65 years and over: A randomised controlled trial. Australian Journal of Physiotherapy 2005; 51: 102–108
- ↑ Koichi K, Daisuke S, Hitoshi W, Atsuko H, and Takeo N; A Comparison of the Effects of Different Water Exercise Programs on Balance Ability in Elderly People, Journal of Aging and Physical Activity, 2008, 16, 381-392
- ↑ Chen JH, Liu C, You L, Simmons CA. Boning up on Wolff’s Law: mechanical regulation of the cells that make and maintain bone. J Biomech. 2010; 43(1):108–18
- ↑ Sinaki M. Yoga spinal flexion positions and vertebral compression fracture in osteopenia or osteoporosis of spine: case series. Pain Pract. 2013;13(1):68–75
- ↑ 21.0 21.1 Kasperk, C., Grafe, I. A., Schmitt, S., Nöldge, G., Weiss, C., Da Fonseca, K., … Nawroth, P. (2010). Three-year Outcomes after Kyphoplasty in Patients with Osteoporosis with Painful Vertebral Fractures. Journal of Vascular and Interventional Radiology, 21(5), 701–709
- ↑ 22.0 22.1 22.2 22.3 Schoenfeld, A. J., & Bono, C. M. (2011). Measuring spine fracture outcomes: Common scales and checklists. Injury, 42(3), 265–270.