Synucleinopathy
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Uchechukwu Chukwuemeka, Kim Jackson and Angeliki Chorti
Introduction[edit | edit source]
Synucleinopathies are a subgroup of neurodegenerative diseases, characterised by impairment of alpha-synuclein (αSyn) metabolism, producing abnormal intracellular deposits (namely progressive aggregation of insoluble fibrillary αSyn in neurons and glia). All of them are chronic, progressive disorders that lack a causal therapy.[1][2]
Although the exact mechanism of initiation of aggregation and misfolding pathway of a-Syn is yet to be discovered; it’s mechanism of spreading through interconnected neuronal networks is a proposed theory. This theory suggests that a-Syn is released from the diseased cell and is then uptaken by normal adjacent cells. [3][4]
Divisions Of Synucleinopathies[edit | edit source]
The synucleinopathies can be divided into those with and those without the formation of Lewy bodies (however some overlap does exist) and include:
- Synucleinopathies with Lewy bodies: Parkinson disease (PD); Lewy body disease (LBD);
- Synucleinopathies without Lewy bodies: Multiple systemic atrophy (MSA); pure autonomic failure; rapid eye movement (REM) sleep behaviour disorder.[1]
This 4 minute video gives a introduction to the synucleinopathies
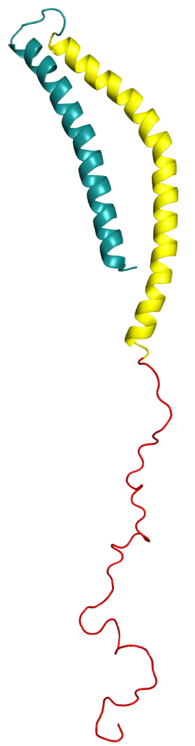
Human Alpha-Synuclein (α-syn)[edit | edit source]
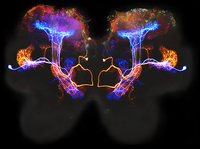
Human alpha-synuclein (α-syn) is predominantly expressed in the brain, accounting for approximately 1% of brain weight. It is found chiefly in the neocortex, hippocampus, substantia nigra, thalamus, and cerebellum, and is found in Lewy bodies (LBs). As well as accumulating in the brain, α-synuclein also accumulates in the gastrointestinal tract resulting in symptoms. [6] [1][3]
Main Symptoms[edit | edit source]
Synucleinopathies are chronic disorders that develop gradually. Symptoms include:
- A decline in motor and cognitive functions
- Behavioral changes.
Symptoms of these diseases significantly overlap with one another, hindering diagnosis. for example parkinsonism is the predominant symptom of PD. Still, it can be indistinguishable from the parkinsonism of LBD and MSA.[7][2]
Diagnosis[edit | edit source]
A new tool developed to reveal abnormal alpha -synuclein in brain and body cells has shown high potential to differentiate people with Parkinson's disease from healthy controls.. [8] In a cross-sectional analysis of 1123 participants, sensitivity for Parkinson's disease was 87·7% (95% CI 84·9–90·5), and specificity for healthy controls was 96·3% (93·4–99·2). The sensitivity of the α-synuclein SAA in sporadic Parkinson's disease with the typical olfactory deficit was 98·6% (96·4–99·4). [8]
Future Management[edit | edit source]
In healthy brain cells, correctly constructed alpha synuclein is typically found just inside the surface of the membrane surrounding the cell body and in the presynaptic terminals (critical to passing messages between neurons).[9]
The abnormal aggregation of α-synuclein has proved to be the “rosetta stone” of PD, DLB, and MSA. There is increasing evidence demonstrating the propagation of pathological α-Syn to be central to the pathogenesis of synucleinopathies, for example in PD and MAS.[2][6]
Comprehending disease aetiology and pathogenesis is a start, but developing safe and effective mechanism-based treatments is the goal. For example, some pharmaceutical companies are focusing on compounds that prevent α-syn from aggregation. When mechanism-based therapies for PD, LBD, and MSA will become available, they will probably interfere with the neurodegeneration caused by the aggregation of α-synuclein.[10]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Radiopedia Synucleinopahy Available from:https://radiopaedia.org/articles/synucleinopathy-1?lang=gb (accessed 15.9.2022)
- ↑ 2.0 2.1 2.2 Sympath Synucleinopathies Available from: http://archive.sympath-project.eu/synucleopathies/?lang=en (accessed 15.9.2022)
- ↑ 3.0 3.1 Kompoliti K, Verhagen L. Encyclopedia of movement disorders. Academic Press; 2010 Feb 26. Available from: https://www.sciencedirect.com/topics/medicine-and-dentistry/synucleinopathies(accessed 15.9.2022)
- ↑ Huang D, Nazarova L. Misfolded α-syn–from release and uptake to contagion of adjacent cell, any links with gut? Available from:http://www.ijsit.com/admin/ijsit_files/MISFOLDED%20SYN%20FROM%20RELEASE%20AND%20UPTAKE%20TO%20CONTAGION%20OF%20ADJACENT%20CELL%20ANY%20LINKS%20WITH%20GUT_IJSIT_10.5.7.pdf (accessed 15.9.2022)
- ↑ Air to air. Synucleinopathy. Available from:https://www.youtube.com/watch?v=fz0lM2-JAo4 [last accessed 15/9/2022]
- ↑ 6.0 6.1 Emamzadeh FN. Alpha-synuclein structure, functions, and interactions. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences. 2016; 21: 29. doi: 10.4103/1735-1995.181989
- ↑ MartÌ MJ, Tolosa E, Campdelacreu J. Clinical overview of the synucleinopathies. Movement disorders. 2003 Sep;18(S6):21-7.
- ↑ 8.0 8.1 Siderowf A, Concha-Marambio L, Lafontant D-E, Farris C. Assessment of heterogeneity among participants in the Parkinson's Progression Markers Initiative cohort using α-synuclein seed amplification: a cross-sectional study. Lancet Neurology 2023 May; 22(5):407-417.
- ↑ The science of PD Alpha Synuclein. Available from: https://scienceofparkinsons.com/alpha-synuclein/ (accessed 15.9.2022)
- ↑ Goedert M, Jakes R, Spillantini MG. The synucleinopathies: twenty years on. Journal of Parkinson's disease. 2017 Jan 1;7(s1):S51-69.