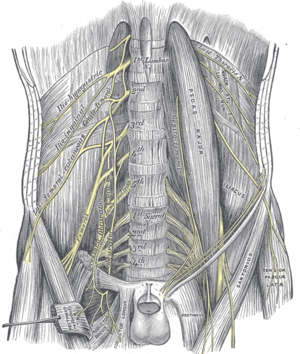
Lumbar Plexus
Original Editor - Carla Benton
Top Contributors - Carla Benton, Kim Jackson, Admin, Laura Ritchie, Libby McConnell, Lucinda hampton, Evan Thomas, WikiSysop and Carina Therese MagtibayIntroduction[edit | edit source]
The lumbar plexus is a complex neural network formed by the lower thoracic and lumbar ventral nerve roots. They are formed where T12 to L5 exit the spinal cord via intervertebral foramina. The supply motor and sensory innervation to the lower limb and pelvic girdle[1].
The nerves arising from the lumbar plexus are important for functioning of the lower extremity function and movement allowing knee extension, hip flexion and adduction of the thigh[2].
Origin and Location[edit | edit source]
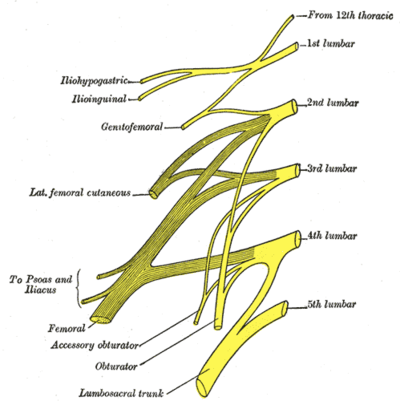
The origin of the lumbar plexus is within the psoas major muscle, anterior to the lumbar transverse processes. The dorsolumbar nerve, which joins the anterior ramus of spinal nerve L1, contributes to the creation of the lumbar plexus via the anterior ramus of spinal nerve T12. The iliohypogastric and ilioinguinal nerves are derived from a single trunk formed by these roots (T12, L1). The anterior rami of L1 and L2 each have a branch that merge to form the genitofemoral nerve.
Nerves[edit | edit source]
The lumbar plexus allows nerves to combine at different levels to create multiple functioning nerves that serve to innervate various structures. The nerves that arise from the lumbar plexus are listed below, from superior to inferior.
- The iliohypogastric nerve is created from spinal levels T12 and L1.
- Sensory input: lateral gluteal area.
- Motor innervation: internal oblique muscle and transverse abdominis.
- The ilioinguinal nerve derives from a branch of the L1 spinal nerve.
- Sensory input: anterior superior and medial parts of the thigh; males, the distal portions of the nerve become the anterior scrotal nerve that inputs sensory fibers to the root of the penis and the superior part of the scrotum; females, the distal portions of the nerve are the anterior labial nerves that help to provide sensory inputs to the skin covering the mons pubis and the labia majora.
- The genitofemoral nerves arise from the superior aspects of L1 and L2 spinal nerves. The nerve divides into the genital and the femoral branch.
- Sensory input (genital branch): Skin of the scrotum in men and the mons pubis and labia majora in women
- Sensory input (femoral branch): innervation to the anterior and superior area of the thigh
- Motor innervation (genital branch): Cremaster muscle in men
- The lateral femoral cutaneous nerve comes from the L2 and L3 spinal nerves.
- Sensory input: It's only function is to supply sensory innervation to most of the lateral portion of the thigh.
- The obturator nerve arises from L2, L3, and L4 spinal nerves.
- Motor innervation: Primary motor supply to the medial (hip adductors) muscle compartment of the thigh. [2].
- The femoral nerve ranks as the largest nerve that arises from the lumbar plexus. It is created from lumbar spinal nerves L2, L3, and L4. It leaves the plexus and enters the femoral triangle, passing just lateral to the femoral artery.
- Sensory input: anterior compartment of the thigh. A portion of the cutaneous branch becomes the saphenous nerve - this provides sensory innervation to the skin over the patella, and portions of the medial and anterior aspects of the distal lower extremity.
- Motor innervation: There are four major branches: muscular (motor), cutaneous, articular, and vascular. They innervate the muscles rectus femoris, sartorius, and articularis genu.
- Its principal function is to supply motor and sensory innervation to the anterior compartment of the thigh.
To remember the major branches of the lumbar plexus why not use this useful Pneumonic?
| Interested | In | Getting | Lunch | On | Friday |
|---|---|---|---|---|---|
| Iliohypogastric | Ilioinguinal | Genitofemoral | Lateral femoral cutaneous | Obturator | Femoral |
Physiotherapy Implications[edit | edit source]
Damage to the lumbar plexus or nerves proximal and distal to it can result in several pathologies. It is important that physical therapists have a good understanding of the lumbar plexus in the treatment of symptomatic patients.
Lumbar disc herniation can cause occlusion of the intervertebral foramen, compressing lumbar spinal nerves near their entry to the lumbar plexus. This syndrome can cause paresthesia and weakening in the lumbar plexus nerves' innervated locations.
The lateral femoral cutaneous nerve, which is a branch of the lumbar plexus, can cause a common and serious nerve compression condition. This is known as meralgia paresthetica, and is caused by the nerve becoming trapped as it passes beneath or through the inguinal ligament.
In order to accurately determine the cause of patients' pain or dysfunction, first it is important to determine which level is affected. This will assist in choosing the right interventions which will lead to better outcomes.
References[edit | edit source]
- ↑ Radiopedia Lumbar Plexus Available from:https://radiopaedia.org/articles/lumbar-plexus (last accessed 14.9.2020)
- ↑ 2.0 2.1 Singh O, Al Khalili Y. Anatomy, Back, Lumbar Plexus. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2019.Available from:https://www.ncbi.nlm.nih.gov/books/NBK545137/ (last accessed 14.9.2020)