Proximal Hamstring Tendinopathy
Original Editor - Ward DeBremme
Top Contributors - Wanda van Niekerk, Kim Jackson, Vidya Acharya, Mandeepa Kumawat, Mariam Hashem, Lisa De Donder, Melissa De Maeyer, Vanessa Rhule, Admin, Lotte De Clerck, 127.0.0.1, WikiSysop, Oyemi Sillo, Rachael Lowe, HaniaElGibaly, Evan Thomas, Naomi O'Reilly, George Prudden and Kai A. Sigel
Description[edit | edit source]
Proximal hamstring tendinopathy (PHT) is commonly seen in long distance runners and athletes taking part in sprinting or hurdles. It is also common among athletes taking part in sports such as football and hockey, which involves a change of direction activities.[1] Proximal hamstring tendinopathy is also referred to as hamstring origin tendinopathy or high hamstring tendinopathy. It can also affect people who do not participate in sport.[2][3] It is characterised by deep, localised pain in the region of the ischial tuberosity.[4] Pain is usually worse during or after activities such as running, lunging, squatting and sitting.[4] This condition can include tendon degeneration, partial tearing and peritendinous inflammatory reactions.[5] Proximal Hamstring Tendinopathy-related Sciatic Nerve Entrapment (PHTrSNE) is a neuropathy caused by fibrosis interposed between the semimembranosus tendon and the sciatic nerve, at the level of the ischial tuberosity.
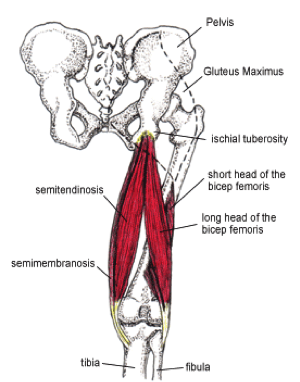
Clinically Relevant Anatomy[edit | edit source]
One of the most important muscle groups in running is the hamstrings muscle group. The hamstrings are active at various stages in the gait cycle, particularly in knee flexion and hip extension. The hamstrings muscles share a common origin on the lateral aspect of the ischial tuberosity. Semitendinosus and the long head of biceps femoris share a conjoined tendon originating from the lateral facet.[6] The origin of Semimembranosus is deeper.[6] Various locations of hamstring tendon pathology have been reported. The semimembranosus is one of the most commonly affected parts of the hamstring muscles in proximal hamstring tendinopathy.[3] Other studies found a variety of locations such as the common hamstring tendon, biceps femoris, semimembranosus and semitendinosus.[7]
The junction between the tendons of the hamstrings and the ischial tuberosity is the area affected by high hamstring tendinopathy. The tendon’s thickness, fibrousness and poor blood supply are the causes of difficult healing.[8]. The muscles contain a higher proportion of type 2 muscle fibres than the other muscles of the lower extremity; suggesting high intrinsic force generation.
During running, the hamstrings have three main functions. First, they decelerate knee extension at the end of the forward swing phase of the gait cycle. Through an eccentric contraction, the hamstrings decelerate the forward momentum (i.e, leg swing) at approximately 30° short of full knee extension. This action helps provide dynamic stabilization to the weight bearing knee. Second, at foot strike, the hamstrings elongate to facilitate hip extension through an eccentric contraction, thus further stabilizing the leg for weight bearing. Third, the hamstrings assist the gastrocnemius in paradoxically extending the knee during the take-off phase of the running cycle.[1]
Proximal hamstring tendinopathy is regarded as insertional tendinopathy.[9]. Compression of the tendon at its attachment during hip flexion/adduction is hypothesized to be an important etiological factor,[9]but the evidence is limited. Other contributing factors may be the presence of a shearing force between the hamstring attachment and the ischial tuberosity[10] and the increased displacement of the proximal hamstring tendon with an increased hip flexion angle.[11]
(For extra information about pathology mechanisms also see Tendinopathy)
Functional Anatomy[edit | edit source]
Proximal hamstring tendinopathy (PHT) rehabilitation requires a good understanding of hamstring muscle function.[4] In athletes, upright running may be an aggravating factor. During upright running, the function of the hamstrings is to eccentrically decelerate the knee in terminal swing phase. Peak forces are reported in the late swing phase, and a second peak is reported in the early stance phase.[12][13] Another contributing factor to proximal hamstring overuse injuries is the storage of energy in the late swing to early stance stretch-shortening cycle. Eccentric to concentric transition is linked to higher hamstring loads.[14]The storage of elastic energy in tendons and aponeuroses have been shown to increase the efficiency of locomotion.[15] With greater hip and trunk flexion, as in running with the trunk leaning forward, or with over-striding as well as uphill running, the proximal hamstring is subjected to higher energy storage loads.[4] Considering these functional requirements, certain suggestions have been made to improve muscle hypertrophy, strength and length-tension differences as well as facilitate the return to sport. These suggestions include an eccentric type of rehabilitation exercises as well as stretch-shorten exercises.[16]
Epidemiology / Etiology[edit | edit source]
With tendinopathy there is a multitude of factors that can contribute to the aetiology. These factors are usually load related. Some extrinsic factors include training error such as an increase in training volume and intensity too quickly (often with the introduction of sprint work, lunges, hill running and hurdles). These type of training errors have been reported in the research as training errors preceding PHT.[17] With this type of activities, the hamstring needs to contract or lengthen when the hip is in flexion. This can lead to a higher tensile and compressive load at the tendon insertion.[18] Another cause of symptoms may be excessive static stretching, i.e in yoga or Pilates. These type of exercises involve sustained end range hip flexion postures.[4] Long periods of sitting can also be a cause in some patients.[19]
Risk Factors:[edit | edit source]
Intrinsic factors:[edit | edit source]
- Malalignments
- Leg length discrepancy
- Imbalance
- Decreased flexibility
- Joint laxity
- Female gender
- Age - Reduction in muscle fibre size and number are associated with advancing in age, this leads to losses of mass and strength.[20]
- Overweight
- Proprioceptive deficiency[21]
- Ischial tuberosity tenderness
- Core weakness[22]
- Pelvic dysfunction[22]
- Previous injury - the strength is reduced by previous hamstrings, knee or groin injuries.[20]
- Neuromyofascial involvement- increased neural tension and posterior thigh pain due to myofascial trigger points; often associated with decreased flexibility.[20]
- Hip stiffness
- Tightness/Weakness of the hamstrings and quadriceps
- Poor lumbopelvic/core stability.[23]
- History of another lower extremity injury - previous injury to the other lower limb, or injuries to other muscles or tendons in the same lower limb.
- Sciatic nerve irritation.
Extrinsic factors:[edit | edit source]
- Excessive, repetitive overloads and overtraining.
- Poor training
- Environmental conditions
- Poor equipment
- Insufficient warm up - A warm-up with isometric contractions increases strength and length of the muscle.[20] A study found an association between hamstrings injuries and lack of stretch prior to sports participation.[20]
- Fatigue - causes a decline in muscle energy, decreased concentration and coordination and poor technique.[20]
Intrinsic and Extrinsic factors contribute to the formation of injury.[8]The tendinopathy usually starts with micro-damage without a remarkable trauma. Normally the tendon is capable to intrinsically repair itself, meaning that the consequences of this injury are little. Sometimes, an imbalance can cause further damage and failed healing. All of this leads to the formation of tendinopathy.
Clinical Picture[edit | edit source]
- Subjectively typical tendon pain behaviour (localised ischial tuberosity pain that becomes less symptomatic after a few minutes of activity, but is worse afterwards)[4]
- Deep buttock pain and pain in the posterior thigh.
- The pain is often felt on the lower gluteal region, radiating along the hamstings[22].
- Provocative activities include activities requiring deeper hip flexion i.e. squats, lunging. long periods of sitting (especially on harder surfaces)[4]
- The pain increases with repetitive activities (such as long-distance running).In some cases pain flares with sitting or driving.
- Rarely painful with activities such as slow walking on a level surface, standing and lying as these type of activities do not involve energy storage or compression[4]
- Occasional stiffness in the morning may be present or when starting to move after a period of prolonged rest[4]
- The onset is mostly gradual, not with acute trauma.[24].
- Continued exercises and stretching can cause even more pain[1]
Pain down the back of the thigh can be caused by irritation of the sciatic nerve. This nerve passes very close to the ischial tuberosity.[8] Due to its degenerative nature, this injury is classified as tendinopathy rather than tendonitis, an inflammatory pathology.[5]
Differential Diagnosis[edit | edit source]
- It is essential to determine if the pain is local or referred. Referred pain is characterized by complaints of pain in various locations. Pain in the buttock combined with pain in the lower back may refer to the lumbar spine. This may be caused by muscles, ligaments or discs dysfunctions.
- Localized constant pain in the buttock, around the ischial tuberosity could be triggered by hamstring origin tendinopathy or ischiogluteal bursitis.
- If the patient complains of pain higher up (upper gluteal region) there might be a problem with the piriformis muscle.
- Pain over the sacrum or near the Sacroiliac Joint refers to a pelvic stress fracture or inflammation or malalignment of the sacroiliac joint.
- There are also some uncommon cases where buttock and posterior thigh pain refer to chronic compartment syndrome of the posterior thigh. Due to the resemblance of some symptoms of this injury with other hip injuries, it’s important to get a proper diagnosis; this will likely entail a physical examination and an MRI.[1]
- Sciatic nerve irritation at piriformis muscle or near the ischial tuberosity[4]
- Ischiofemoral impingement[4]
- Unfused ischial growth plate in a post-adolescent athlete[4]
- Apophysitis or avulsion fracture among adolescents[4]
- Deep gluteal muscle tear[4]
- Posterior pubic or ischial ramus stress fracture[4]
- Partial or complete rupture of the proximal hamstring tendon[4]
Diagnostic Procedures[edit | edit source]
Imaging[edit | edit source]
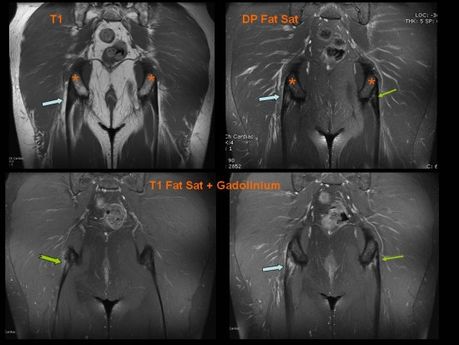
MRI is required to confirm the diagnosis and to take a look at the severity of the injury. MRI can detect tendon thickening, tearing, inflammation and swelling at the ischial tuberosity.
Ultrasound is also used, but this technique isn’t able to give precise visualisation of bone marrow oedema.[25] Normally a high hamstring injury may be combined with stress reaction or bone oedema in the ischial tuberosity and findings of the tendon. In case of a tendinopathy, an increased signal is noticeable on T1-weighted images with no abnormalities on fat-suppressed T2-weighted images.[1][5]
A series of provocation tests have been developed in order to help for the diagnosis of this injury.
Passive Stretch Tests[edit | edit source]
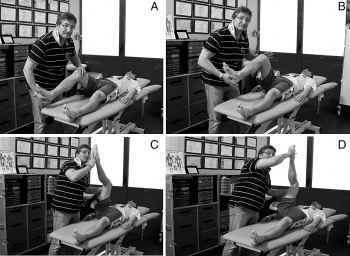
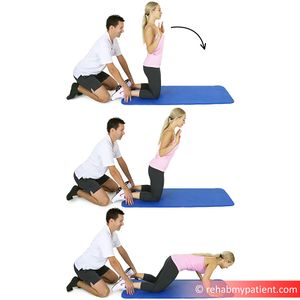
The bent-knee stretch, the modified bent-knee stretch and the Puraven-Orava test are used as passive stretch tests in the diagnosis of PHT. These tests have moderate to high validity and high sensitivity and specificity for the diagnosis of PHT.[26]
Bent-knee stretch test:[edit | edit source]
The test is performed while the patient is lying supine. The hip and knee are maximally flexed. Slowly the therapist will straighten the knee till its maximally extended; the hip must remain in 90° of flexion. The test is also doable without the assistance of a therapist. The patient can use a rope or a belt to straighten his knee like depicted on the picture.
Modified bent-knee stretch test[edit | edit source]
The test is performed while the patient is lying supine, the hip and knee are in extension. The therapist takes the heel in one hand and holds the knee with the other hand. He brings the hip and knee in maximal flexion and then rapidly straightens the knee.
These tests are used to identify a hamstrings origin tendinopathy, but do not replace an MRI.[8]
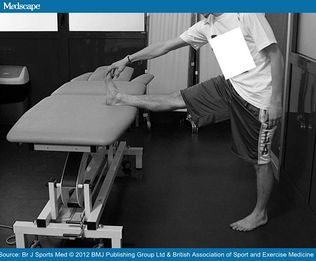
The Puranen-Orava test[edit | edit source]
The Puranen-Orava test is a standing test that actively stretches the hamstring when the hip is flexed to 90° and the knee is extended fully and the foot is on a support 90° to the standing body.
Goom et al[4] reports that in their clinical experience, these tests may be negative in less symptomatic cases, It is also important to consider other clinical conditions that may be present and responsible for the symptoms. The use of MRI in diagnosis of PHT is recommended.[26]
Furthermore, the pain response to palpation vary and may have low specificity in the diagnosis of tendinopathies.[27]
Palpation of the ischial tuberosity[edit | edit source]
Higher quality research studies are needed to investigate the use of special tests in the diagnosis of hamstring injuries.[28] The lack of high-quality evidence reiterates the importance of combining various tests results with a comprehensive and detailed history to determine tendon pain behaviour in diagnosing proximal hamstring tendinopathy.[4]
Loading Tests[edit | edit source]
The reproduction of pain with various loading tests can aid in the diagnosis of proximal hamstring tendinopathy (PHT), but the accuracy of these tests still needs to be investigated more extensively. The principle is to reproduce the pain by loading the proximal hamstring tendons. This is done by progressively increasing the compressive and tensile load, by increasing the angle of hip flexion.[4][29]
An example of a load test assessment for patients with proximal hamstring tendinopathy may consist of progression from the single leg bent knee bridge (low load clinical test) to the long lever bridge (moderate load) and arabesque movements to single leg deadlift (high-load clinical test).[4][29] The movements are initiated slowly at first and only adding speed if patient is asymptomatic. The pain score should increase with the load across all these tests.[4]
Higher quality research are needed to investigate the clinical use of special tests in the diagnosis of hamstring injuries.[4][28] It remains essential to combine test results with a comprehensive and detailed history to determine tendon behaviour in diagnosing proximal hamstring tendinopathy.[4]
Physical Therapy Management[edit | edit source]
During rehabilitation, patients may experience pain. Pain provocation after energy storage activities is acceptable, provided that the pain does not last longer than 24 hours.[4][30][31] Pain provocation lasting longer than 24 hours can be classified as "irritable". Pain that settles within 24 hours of energy storage loading can be classified as "stable".[32] After the initial warm-up (pain becoming less after a few minutes of activity), stable tendon pain may return towards or afterwards the activity.[32]
Symptom management - Load modification[edit | edit source]
Training load management or modification is essential in the management of tendon-related pain, even more so in patients with irritable symptoms.[4] It is advisable to limit pain producing compressive and energy storage load activities (i.e. increased hip flexion) until the pain irritability settles to stable pain[4]. Stable pain is mild (VAS 0 to 3 out of 10) and usually settles with 24 hours of moderate to high tendon load interventions (e.g. repeated lunging). Determine subjectively what activities increase the patients' symptoms and the time frame (for how long?). This will help the clinician determine the irritability level as well as what type of load management strategy will be effective. Often the patient will be able to continue with certain activities such as steady state running within the pain/aggravation guidelines. More compressive and energy storage activities such as hill running, quick starts and hurdles should be avoided initially and only implemented at later stages[4].
In tendinopathy rehabilitation research there are varying outcomes in the different tendons. In Achilles tendinopathy rehabilitation it has been reported that continuing sports activities did not lead to worse outcomes compared to stopping sports activities in the first 6 weeks of rehabilitation.[33] This is in contrast to patellar tendinopathy though.[34] Patients or runners with PHT may often report certain distances that they are able to run without any symptoms or report activities where symptoms are only present during certain types of training(e.g. squats). If symptoms persist for longer than 24 hours after the activity, despite partial load management, it is advisable to stop with the aggravating activities. If symptoms are really reactive and irritable, it is best to stop with all painful compression and energy storage activities until the symptoms settle and become stable[4].
Aggravating sporting activities may be replaced with cross-training to maintain cardiovascular fitness, or these activities can be adapted to reduce the load. Examples of such activities are[4]:
- Cycling may be better tolerated if a patient is performing it standing
- Swimming and water running are good options
- Posture modification may reduce symptoms (e.g. reduce hamstring origin compression by reducing anterior pelvic tilt and hip flexion in standing)
- When sitting is symptomatic, shaped cushions are useful to reduce the compression. It allows for more weight bearing on the posterior thigh rather than the ischium
- Avoid repeated stretching of the hamstrings in the early, reactive phase
- Avoid hip flexion dominant movements such as trunk flexion and repeated lifting in the early, reactive stages
Rehabilitation[edit | edit source]
Load management is the key to tendinopathy management. Progressive loading, performed within a pain-monitoring framework, is essential to reduce pain and ultimately restore function.[4] Rehabilitation should incorporate the whole kinetic chain[35].
Exercise prescription[edit | edit source]
Goom et al[4] recommend the following rehabilitation stages in proximal hamstring tendinopathy, based on the current evidence available.
In general, the following should apply:
- Resistance training principles should be applied to ensure optimal loading, contraction speed and time under tension[36]
- Monitor pain at the same time on a daily basis with a load test during rehabilitation[4]
- Some pain is allowed during and after exercise (Stable pain - VAS 0 to 3 out of 10)[30]
- Symptoms should settle within 24 hours
- Symptoms should not progressively worsen over the course of the loading program[33]
- Treat every patient individually and focus on particular phases of rehabilitation or kinetic chain factors specific to the individual[4]
- Progression through the exercise stages should be based on the symptoms and the response when progressing the exercise load and not on specific time frames[4]
- The 4 stage program may take 3 -6 months to complete, but the variation will most likely be present[4]
Stage 1: Isometric hamstring load[4][edit | edit source]
Isometric exercises in positions without tendon compression is proposed as an effective method of loading the muscle-tendon unit as well as reduce pain in proximal hamstring tendinopathy with irritable symptoms.[29] It has been reported that isometric exercises have a pain inhibitory response.[37] It is recommended that isometric exercises should be repeated several times per day[38]. Symptom severity and irritability are used to determine the dosage. The dosage can be adjusted to shorter/less intense contractions or vice versa based on the symptoms.
In the early stages of proximal hamstring tendinopathy (PHT) the position of the hip should be near neutral hip flexion-extension or in minimal hip flexion (20°- 30° for a straight leg pulldowns).[4] A favourable sign for isometric hamstring loading is an immediate reduction in pain with hamstring loading tests after exercise.[4]
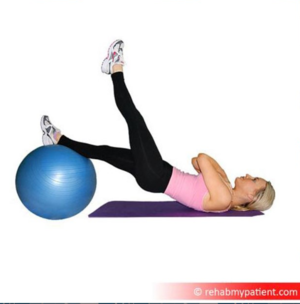
Appropriate exercises for stage I rehabilitation[4][edit | edit source]
- Isometric leg curl
- Bridge holds - hip in neutral
- Isometric straight leg pulldowns
- Trunk extensions
- Isometric long leg bridging on two, progressing to one leg holds
Stage 2: Isotonic hamstring load with minimal hip flexion[4][edit | edit source]
Important aspects of proximal hamstring tendinopathy rehabilitation is:
- to restore hamstring strength[39]
- to restore hamstring muscle bulk and capacity in a functional range of movement[39]
Isotonic hamstring loading may be started when there is minimal or no pain (VAS 0 -3 out of 10) during hamstring loading in early ranges of hip flexion. Although eccentric exercises are widely accepted as the treatment of choice for tendinopathies[40], there is not sufficient evidence for isolating the eccentric component[41]. Therefore, Heavy Slow Resistance training (HSR) is advocated. Heavy Slow Resistance training includes eccentric and concentric elements. It has also been shown to compare favourably with isolated eccentric loading in tendinopathy rehabilitation.[30][40]
With HSR, the aim is to perform a slow fatiguing resisted isotonic exercise. Commence with 15 RM (the maximum load that can be lifted 15 times in a single set) and progress to 8 RM. Perform 3-4 sets every second/other days (1) Hold contractions for 3 seconds for each phase of the exercise (concentric and eccentric)[30].
Minimise loaded hip flexion to in the early stages. This is advised to protect the enthesis against too much compression.[9] It is important to concentrate on single-leg work to address asymmetrical strength loss. Continue with stage 1 isometric exercises on the "off" days. This will help with symptom (pain) management, especially if there are still symptoms present[4].
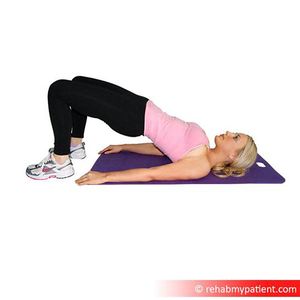
Appropriate exercises for stage 2[4][edit | edit source]
- Single leg bridge
- prone hip extension
- prone leg curl
- Nordic hamstring exercise
- Bridging progressions
- Supine leg curl
Stage 3: Isotonic exercises in increased hip flexion (70° - 90°)[4][edit | edit source]
The aim of rehabilitation in this stage is
- to continue with hamstring muscle strengthening in greater hip flexion
- to continue with muscle hypertrophy in greater hip flexion
- to continue with functional training in greater hip flexion
Once there is minimal pain or no pain (VAS 0 - 3 out of 10) with higher loading hip flexion tests such as lunging and arabesques, isotonic strengthening in increased hip flexion can be implemented. The dosage and frequency of exercises remain the same as in stage 2. The technique is important and exercises should be performed slow and controlled. The progression into greater hip flexion often cause pain and irritability and is important to monitor the 24-hour response post exercise with loading tests into hip flexion (hamstring bridge, deadlift, single leg arabesque).[29]
Appropriate exercises for stage 3[4][edit | edit source]
- slow hip thrusts
- forward step-ups
- walking lunges
- deadlifts
- Romanian deadlifts
At the end of phase 3, patients with PHT should be able to load the proximal hamstring comfortably through sport-specific ranges with little aggravation of symptoms[4].
Stage 4: Energy storage loading[4][edit | edit source]
This stage is only necessary for patients and athletes returning to sports that involve lower limb energy storage or impact loading[4]. Introduction of power/elastic stimulus for the myotendinous unit can start when there is minimal pain during load tests (VAS 0-3 out of 10). It is also essential to have adequate bilateral strength in single leg exercises from stage 2 and 3. Good movement control is also needed. In the early phase of stage 4, it is advised to limit the amount of hip flexion, to protect the proximal hamstring tendon from compression. Note that this is the most provocative stage in the rehabilitation process and a conservative approach is needed for dosage and frequency of the exercises prescribed. Start with performing exercises only every third day. Follow with a stage 1 day, to settle the tendon. The following day will then include strengthening exercises from stage 2-3. This adds up to a 3-day high-low-medium tendon load cycle, twice a week, with a rest day between cycles.[42]
Appropriate exercises for stage 4[4][edit | edit source]
- Sprinter leg curl
- A-skips
- Fast sled push or pull
- Alternate leg split squats
- Bounding
- Stair or hill bounding
- Kettlebell swings
- Lateral, rotational cutting movements
Return to sport[edit | edit source]
Return to sports can be gradually introduced when the athlete is able to cope with the loading requirements of the sport with minimal symptom aggravation (i.e. VAS 0 -3 of 10 with pain settling within 24 hours on load tests). The exercise progressions form stepping stones for return to sport, but it is important to not just add these exercises to the normal training volume on resumption, as this can lead to overloading and aggravation of symptoms.[4][34] Be careful with the introduction of hill training as well as speed training sessions, as these can easily exacerbate symptoms. In team sports, there may be more complex loading requirements. This needs a more detailed assessment and a graded return to sport will usually consist of gradual exposure to activity prior to return to full competition[4].
Other Physical Therapy management considerations[edit | edit source]
- Limited evidence is available on the effectiveness of dry needling and soft tissue techniques in the treatment of PTH, but supporting evidence is available in published case series[17]
- Massage and manual therapy can be useful in PHT when these are used to address tone and restriction in the kinetic chain[4]
- Take note that these passive interventions will not improve tissue load capacity, which is the key element of tendinopathy rehabilitation[4][35]
- When conservative treatment fails, the patient may need surgery to decrease the pressure on the nerve and to divide the fibrous and damaged tendon.[20]
Adjunct treatment methods[edit | edit source]
- Anti-inflammatory medication[8]- It is suggested that NSAID's may settle irritable tendon pain. It may also inhibit tenocyte overstimulation and signalling[44]. It is not clear if NSAID's compromise tendon healing, but research has indicated that ibuprofen administration does not seem to hinder normal tendon adaptation in response to resistance training.[4]
- Peritendinous corticosteroid injection-In more severe cases, when physical therapy does not help, a corticosteroid injection into the peritendinous soft tissues is recommended in combination with physical therapy. Injecting the substance in the tendon itself can be dangerous. Frederickson et al[1] found that patients whose MRIs showed more swelling around the ischial tuberosity and less thickening of the tendon got more relief from a cortisone injection than patients with more pronounced tendon thickening. However, corticosteroid injections can also have a negative impact on the tendons inter alia the weakening of tendons, the rupture of tendons, particularly in load-bearing tendons. Furthermore, it may bring short term relief, but there is a tendency for symptoms to recur.[3]
- Platelet-rich plasma injection-A novel treatment is platelet-rich plasma injection at the origin of the muscle.[8] Platelet-rich plasma (PRP) seems to be a promising alternative to corticosteroid injections. The alpha and dense granulates that are present in the platelets, release multiple growth factors and cytokines that promote wound healing[45]. An enhancement of the recruitment, proliferation and differentiation of the cells involved in soft-tissue regeneration has been reported by the authors of in vitro studies.[46] At present, there is however not enough evidence to support the use of platelet-rich therapies in the treatment of musculoskeletal soft tissue injuries[47]
- Extracorporeal shockwave therapy (ESWT).[5] Cacchio et al[48] reported a superior result with ESWT compared to traditional conservative treatment in the treatment for proximal hamstring tendinopathy. The results of this study, however, is limited by the relatively small sample size compromising the external validity of this study.[49] Furthermore, the traditional conservative treatment in the study by Cacchio et al[48] consisted of NSAID's in the first week. physiotherapy treatment included ultrasound daily for two weeks, transverse friction massage 3 days a week for the first 2 weeks, and an exercise program consisting of conventional hamstring stretches and isotonic strengthening exercises for 3 weeks. The dosage and frequency, as well as the progression of the exercises given to participants in this study, differs from what is currently advocated in tendinopathy research. Further research is needed into the efficacy of ESWT for the treatment of proximal hamstring tendinopathy as well as research into the use of ESWT compared to more appropriate and current tendinopathy treatment options[49].
For more detailed information see Tendinopathy Treatments Adjuncts
Outcome Measures[edit | edit source]
- VISA-H[50]
Resources[edit | edit source]
Also have a look at the infographic here: https://www.running-physio.com/phtvids/
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Fredericson M, Moore W, Guillet M, Beaulieu C. High hamstring tendinopathy in runners: meeting the challenges of diagnosis, treatment, and rehabilitation. The Physician and sports medicine. 2005 Jan 1;33(5):32-43.
- ↑ Jesus JF, Bryk FF, Moreira VC, Nakaoka GB, Reis AC, Lucareli PR. Gluteus Maximus inhibition in proximal hamstring tendinopathy. MedicalExpress. 2015 Aug;2(4)..
- ↑ 3.0 3.1 3.2 Lempainen L, Johansson K, Banke IJ et al. Expert opinion: diagnosis and treatment of proximal hamstring tendinopathy. Muscles Ligaments Tendons J. 2015;5: 23 - 28
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 4.23 4.24 4.25 4.26 4.27 4.28 4.29 4.30 4.31 4.32 4.33 4.34 4.35 4.36 4.37 4.38 4.39 4.40 4.41 4.42 4.43 4.44 4.45 4.46 4.47 4.48 4.49 4.50 4.51 4.52 Goom TS, Malliaras P, Reiman MP, Purdam CR. Proximal Hamstring Tendinopathy: Clinical Aspects of Assessment and Management. J Orthop Sports Phys Ther. 2016 Jun;46(6):483-93
- ↑ 5.0 5.1 5.2 5.3 Zissen MH, Wallace G, Stevens KJ, Fredericson M, Beaulieu CF. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. American Journal of Roentgenology. 2010 Oct;195(4):993-8.
- ↑ 6.0 6.1 Philippon MJ1, Ferro FP, Campbell KJ, Michalski MP, Goldsmith MT, Devitt BM, Wijdicks CA, LaPrade RF. A qualitative and quantitative analysis of the attachment sites of the proximal hamstrings. Knee Surg Sports Traumatol Arthrosc. 2015 Sep;23(9):2554-61.
- ↑ Benazzo F, Marullo M, Zanon G, Indino C,Pelillo F. Surgical management of chronic proximal hamstring tendinopathy in athletes: a 2 to 11 years of follow-up. J Orthop Traumatol. 2013 Jun; 14(2): 83–89.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 High hamstring tendinopathy injuries – Signs, symptoms and research-backed treatment solutions for a literal pain in the butt. Available from:accessed from http://runnersconnect.net/running-injury-prevention/high-hamstring-tendinopathy-injuries-a-pain-in-the-butt/ on 27/04/2019.
- ↑ 9.0 9.1 9.2 Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. British journal of sports medicine. 2009 Jun 1;43(6):409-16.
- ↑ Hamming MG, Philippon MJ, Rasmussen MT, Ferro FP, Turnbull TL, Trindade CA, LaPrade RF, Wijdicks CA. Structural properties of the intact proximal hamstring origin and evaluation of varying avulsion repair techniques: an in vitro biomechanical analysis. The American journal of sports medicine. 2015 Mar;43(3):721-8.
- ↑ Harvey MA, Singh H, Obopilwe E, Charette R, Miller S. Proximal Hamstring Repair Strength: A Biomechanical Analysis at 3 Hip Flexion Angles. Orthop J Sports Med. 2015;3(4):2325967115576910
- ↑ Chumanov ES, Heiderscheit BC, Thelen DG. Hamstring musculotendon dynamics during stance and swing phases of high-speed running. Med Sci Sports Exerc. 2011;43(3):525-32.
- ↑ Guex K, Millet GP. Conceptual framework for strengthening exercises to prevent hamstring strains. Sports medicine. 2013 Dec 1;43(12):1207-15.
- ↑ Schache AG, Dorn TW, Blanch PD, Brown NA, Pandy MG. Mechanics of the human hamstring muscles during sprinting. Med Sci Sports Exerc. 2012 Apr;44(4):647-58.
- ↑ Alexander RM. Tendon elasticity and muscle function. Comp Biochem Physiol A Mol Integr Physiol. 2002 Dec;133(4):1001-11.
- ↑ Malliaropoulos N, Mendiguchia J, Pehlivanidis H, et al Hamstring exercises for track and field athletes: injury and exercise biomechanics, and possible implications for exercise selection and primary prevention Br J Sports Med 2012;46:846-851.
- ↑ 17.0 17.1 Jayaseelan DJ, Moats N, Ricardo CR. Rehabilitation of proximal hamstring tendinopathy utilizing eccentric training, lumbopelvic stabilization, and trigger point dry needling: 2 case reports. J Orthop Sports Phys Ther. 2014 Mar;44(3):198-205.
- ↑ Docking S1, Samiric T, Scase E, Purdam C, Cook J. Relationship between compressive loading and ECM changes in tendons. Muscles Ligaments Tendons J. 2013 May 21;3(1):7-11.
- ↑ Lempainen L, Sarimo J, Matilla K, Orava S. Proximal hamstring tendinopathy- overview of the problem with emphasis on the surgical treatment. Operative Techniques in Sports Medicine. 2009; 17: 225 -228
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 20.6 P.BRUKNER & K. KAHN, clinical sports medicine, McGraw-Hill, Australia, 2005 (third edition), P388-390
- ↑ White, K. E., High hamstring tendinopathy in 3 female long distance runners. Journal of Chiropractic Medicine 2011, 10 (2), 93-99
- ↑ 22.0 22.1 22.2 Fredericson M, Moore W, Guillet M, Beaulieu C. High hamstring tendinopathy in runners: meeting the challenges of diagnosis, treatment, and rehabilitation. The Physician and sportsmedicine. 2005 Jan 1;33(5):32-43.
- ↑ Tele Demetrious and Brett Harrop. Hamstring Origin Tendonitis. PhysioAdvisor 2008. https://www.physioadvisor.com.au/injuries/buttock/hamstring-origin-tendonitis/
- ↑ Puranen J, Orava S. The hamstring syndrome: a new diagnosis of gluteal sciatic pain. The American journal of sports medicine. 1988 Sep;16(5):517-21.
- ↑ McCormack JR. The management of bilateral high hamstring tendinopathy with ASTYM® treatment and eccentric exercise: a case report. Journal of Manual & Manipulative Therapy. 2012 Aug 1;20(3):142-6.
- ↑ 26.0 26.1 Cacchio A, Borra F, Severini G, Foglia A, Musarra F, Taddio N, De Paulis F. Reliability and validity of three pain provocation tests used for the diagnosis of chronic proximal hamstring tendinopathy. Br J Sports Med. 2012 Sep 1;46(12):883-7.
- ↑ Cook JL, Khan KM, Kiss ZS, Purdam CR, Griffiths L. Reproducibility and clinical utility of tendon palpation to detect patellar tendinopathy in young basketball players. Victorian Institute of Sport tendon study group. Br J Sports Med. 2001 Feb;35(1):65-9
- ↑ 28.0 28.1 Reiman MP1, Loudon JK, Goode AP. Diagnostic accuracy of clinical tests for assessment of hamstring injury: a systematic review. J Orthop Sports Phys Ther. 2013 Apr;43(4):223-31.
- ↑ 29.0 29.1 29.2 29.3 Cook JL, Purdam CR. The challenge of managing tendinopathy in competing athletes. Br J Sports Med. 2014 Apr;48(7):506-9.
- ↑ 30.0 30.1 30.2 30.3 Kongsgaard M, Kovanen V, Aagaard P, Doessing S, Hansen P, Laursen AH, Kaldau NC, Kjaer M, Magnusson SP. Corticosteroid injections, eccentric decline squat training and heavy slow resistance training in patellar tendinopathy.Scand J Med Sci Sports. 2009 Dec;19(6):790-802.
- ↑ Silbernagel KG, Thomeé R, Thomeé P, Karlsson J. Eccentric overload training for patients with chronic Achilles tendon pain--a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports. 2001 Aug;11(4):197-206.
- ↑ 32.0 32.1 Malliaras P, Cook J, Purdam C, Rio E. Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. J Orthop Sports Phys Ther. 2015 Nov;45(11):887-98.
- ↑ 33.0 33.1 Silbernagel KG1, Thomeé R, Eriksson BI, Karlsson J. Continued sports activity, using a pain-monitoring model, during rehabilitation in patients with Achilles tendinopathy: a randomized controlled study. Am J Sports Med. 2007 Jun;35(6):897-906
- ↑ 34.0 34.1 Visnes H, Hoksrud A, Cook J, Bahr R. No effect of eccentric training on jumper's knee in volleyball players during the competitive season: a randomized clinical trial. Clin J Sport Med. 2005 Jul;15(4):227-34
- ↑ 35.0 35.1 Cook JL, Docking SI. "Rehabilitation will increase the 'capacity' of your …insert musculoskeletal tissue here…." Defining 'tissue capacity': a core concept for clinicians. Br J Sports Med. 2015 Dec;49(23):1484-5
- ↑ American College of Sports Medicine. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009 Mar;41(3):687-708
- ↑ Naugle KM, Fillingim RB, Riley JL 3rd. A meta-analytic review of the hypoalgesic effects of exercise. J Pain. 2012 Dec;13(12):1139-50
- ↑ Cook JL, Rio E, Purdam CR, et al Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research? Br J Sports Med 2016;50:1187-1191
- ↑ 39.0 39.1 Scott A, Docking S, Vicenzino B, Alfredson H, Murphy RJ, Carr AJ, Zwerver J, Lundgreen K, Finlay O, Pollock N, Cook JL, Fearon A, Purdam CR, Hoens A, Rees JD, Goetz TJ, Danielson P. Sports and exercise-related tendinopathies: a review of selected topical issues by participants of the second International Scientific Tendinopathy Symposium (ISTS) Vancouver 2012. Br J Sports Med. 2013 Jun;47(9):536-44.
- ↑ 40.0 40.1 Beyer R, Kongsgaard M, Hougs Kjær B, Øhlenschlæger T, Kjær M, Magnusson SP. Heavy Slow Resistance Versus Eccentric Training as Treatment for Achilles Tendinopathy: A Randomized Controlled Trial. Am J Sports Med. 2015 Jul;43(7):1704-11.
- ↑ Malliaras P, Barton CJ, Reeves ND, Langberg H. Achilles and patellar tendinopathy loading programmes : a systematic review comparing clinical outcomes and identifying potential mechanisms for effectiveness. Sports Med. 2013 Apr;43(4):267-86
- ↑ Rudavsky A, Cook J. Physiotherapy management of patellar tendinopathy (jumper's knee). J Physiother. 2014 Sep;60(3):122-9
- ↑ Rebalance Sports Medicine Physiotherapy & Chiropractic. Available from https://www.youtube.com/channel/UC7DHpv8N6PKsQYvkR4KsTlA
- ↑ Tsai WC1, Tang FT, Hsu CC, Hsu YH, Pang JH, Shiue CC. Ibuprofen inhibition of tendon cell proliferation and up-regulation of the cyclin kinase inhibitor p21CIP1.J Orthop Res. 2004 May;22(3):586-91.
- ↑ Alsousou J, Ali A, Willett K, Harrison P. The role of platelet-rich plasma in tissue regeneration. Platelets. 2013;24(3):173-82
- ↑ Hall MP, Band PA, Meislin RJ, Jazrawi LM, Cardone DA. Platelet-rich plasma: current concepts and application in sports medicine. J Am Acad Orthop Surg. 2009 Oct;17(10):602-8
- ↑ Moraes VY, Lenza M, Tamaoki MJ, Faloppa F, Belloti JC. Platelet-rich therapies for musculoskeletal soft tissue injuries. Cochrane Database Syst Rev. 2013 Dec 23;(12):CD010071
- ↑ 48.0 48.1 Cacchio A, Rompe JD, Furia JP, Susi P, Santilli V, De Paulis F. Shockwave therapy for the treatment of chronic proximal hamstring tendinopathy in professional athletes. Am J Sports Med. 2011 Jan;39(1):146-53
- ↑ 49.0 49.1 Korakakis V, Whiteley R, Tzavara A, et al The effectiveness of extracorporeal shockwave therapy in common lower limb conditions: a systematic review including quantification of patient-rated pain reduction Br J Sports Med 2018;52:387-407.
- ↑ Cacchio A, De Paulis F, Maffulli N. Development and validation of a new visa questionnaire (VISA-H) for patients with proximal hamstring tendinopathy. Br J Sports Med. 2014 Mar;48(6):448-52
- ↑ Craig Purdam - What about hamstring tendinopathy?!Available from https://www.youtube.com/watch?v=FkOCoYq9iQQ