Sleep Apnea: Difference between revisions
No edit summary |
(Added breathing exercise section) |
||
| (6 intermediate revisions by 2 users not shown) | |||
| Line 7: | Line 7: | ||
== Definition/Description == | == Definition/Description == | ||
Sleep apnea is a disorder in which [[How We Breathe|breathing]] is interrupted or paused during sleep. The pauses in breathing can last a few seconds to minutes and are long enough to: | Sleep apnea is a disorder in which [[How We Breathe|breathing]] is interrupted or paused during sleep. The pauses in breathing can last a few seconds to minutes and are long enough to: | ||
*Disrupt sleep | *Disrupt sleep | ||
| Line 17: | Line 17: | ||
# '''Mixed sleep apnea''' is a combination of both obstructive and central sleep apnea episodes.<ref name="Strohl1" /> | # '''Mixed sleep apnea''' is a combination of both obstructive and central sleep apnea episodes.<ref name="Strohl1" /> | ||
== | == Aetiology == | ||
[[File:OSA2.jpg|right|frameless|424x424px]] | [[File:OSA2.jpg|right|frameless|424x424px]] | ||
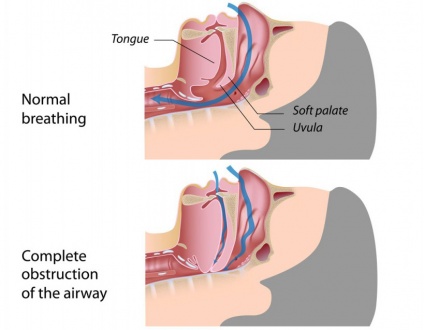
Sleep apnea occurs when there is not enough space to accommodate sufficient airflow in a portion of the upper airway during sleep. | Sleep apnea occurs when there is not enough space to accommodate sufficient airflow in a portion of the upper airway during sleep. | ||
| Line 23: | Line 23: | ||
* In children, the most common cause of obstructive sleep apnea is enlarged tonsils and/or adenoids. | * In children, the most common cause of obstructive sleep apnea is enlarged tonsils and/or adenoids. | ||
* In adults, it is most commonly associated with [[obesity]], male sex, and [[Older People - An Introduction|advancing age]].<ref name=":0">Slowik JM, Collen JF. [https://www.ncbi.nlm.nih.gov/books/NBK459252/ Obstructive Sleep Apnea].(2019)Available from:https://www.ncbi.nlm.nih.gov/books/NBK459252/ (last accessed 5.10.2020)</ref> | * In adults, it is most commonly associated with [[obesity]], male sex, and [[Older People - An Introduction|advancing age]].<ref name=":0">Slowik JM, Collen JF. [https://www.ncbi.nlm.nih.gov/books/NBK459252/ Obstructive Sleep Apnea].(2019)Available from:https://www.ncbi.nlm.nih.gov/books/NBK459252/ (last accessed 5.10.2020)</ref> | ||
Factors that contribute to airway obstruction are:<ref name="diagnose5" /> | Factors that contribute to airway obstruction are:<ref name="diagnose5">Downey III R, Rowley J, Wickramasinghe H, Gold P. Obstructive Sleep Apnea Differential Diagnoses. Emedicinemedscapecom. 2016. Available at: http://emedicine.medscape.com/article/295807-differential. Accessed April 9, 2016.</ref> | ||
*Obesity | *Obesity | ||
*Large neck circumference | *Large neck circumference | ||
| Line 45: | Line 45: | ||
* Prevalence also increases with age, and when individuals reach 50 years of age or more, there are as many women as men who develop the disorder.<span style="line-height: 1.5em;"> </span> | * Prevalence also increases with age, and when individuals reach 50 years of age or more, there are as many women as men who develop the disorder.<span style="line-height: 1.5em;"> </span> | ||
* <span style="line-height: 1.5em;">Genetics and abnormalities or conditions of the craniofacial morphology also increase the likelihood of OSA. Individuals with a first-degree relative with OSA were at a 1.5-2x increased risk of developing OSA</span><ref name=":0" /><span style="line-height: 1.5em;">.</span><ref name="prevalence2">Lam J, Sharma S, Lam B. Obstructive sleep apnea: Definitions, epidemiology & natural history. Indian J Med Res 2010;131:165-170. http://pharexmedics.com/wp-content/uploads/2015/11/sleepapnea_ebook.pdf (accessed 3 April 2016).</ref> | * <span style="line-height: 1.5em;">Genetics and abnormalities or conditions of the craniofacial morphology also increase the likelihood of OSA. Individuals with a first-degree relative with OSA were at a 1.5-2x increased risk of developing OSA</span><ref name=":0" /><span style="line-height: 1.5em;">.</span><ref name="prevalence2">Lam J, Sharma S, Lam B. Obstructive sleep apnea: Definitions, epidemiology & natural history. Indian J Med Res 2010;131:165-170. http://pharexmedics.com/wp-content/uploads/2015/11/sleepapnea_ebook.pdf (accessed 3 April 2016).</ref> | ||
* <span style="line-height: 1.5em;">OSA is common in individuals who spend long periods of time sitting and driving, such as commercial truck drivers.</span><ref name="Management" /> | * <span style="line-height: 1.5em;">OSA is common in individuals who spend long periods of time sitting and driving, such as commercial truck drivers.</span><ref name="Management">Epstein L, Kristo D, Strollo Jr. P, Friedman N, Malhotra A, Patil S, et al. Clinical Guideline for the Evaluation, Management and Long-term Care of Obstructive Sleep Apnea in Adults. Journal of Clinical Sleep Medication 2009; 5(3): 263-276. http://pharexmedics.com/wp-content/uploads/2015/11/sleepapnea_ebook.pdf (accessed 3 April 2016).</ref><sup></sup> | ||
<sup></sup> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
[[Image:SnS.jpg|border|590x600px|right|frameless]]Typical adult obstructive sleep apnea patient | |||
* Overweight or obese middle-aged male or postmenopausal female with excessive daytime sleepiness and loud nightly snoring. | * Overweight or obese middle-aged male or postmenopausal female with excessive daytime sleepiness and loud nightly snoring. | ||
* May also complain of waking to gasp for breath or choking, sleep maintenance insomnia, night sweats, nighttime reflux, and nocturia in the absence of excessive nighttime liquid intake. | * May also complain of waking to gasp for breath or choking, sleep maintenance insomnia, night sweats, nighttime reflux, and nocturia in the absence of excessive nighttime liquid intake. | ||
* Typically larger than average neck circumference (17 inches in males) with crowded oropharynx and large tongue. | * Typically larger than average neck circumference (17 inches in males) with crowded oropharynx and large tongue. | ||
* Retrognathism (an abnormal posterior positioning of the maxilla or mandible relative to the facial skeleton and soft tissues) may be present. | * Retrognathism (an abnormal posterior positioning of the maxilla or mandible relative to the facial skeleton and soft tissues) may be present. | ||
Patients with refractory atrial fibrillation, resistant hypertension, and history of a stroke should be screened for sleep apnea regardless of symptoms<ref name=":0" /> | Patients with refractory atrial fibrillation, resistant hypertension, and history of a stroke should be screened for sleep apnea regardless of symptoms<ref name=":0" /> | ||
Typical child with obstructive sleep apnea | |||
* Loud nightly snoring | * Loud nightly snoring | ||
* May be hyperactive rather than sleepy | * May be hyperactive rather than sleepy | ||
| Line 66: | Line 64: | ||
== Treatment == | == Treatment == | ||
For adults, the use of continuous positive airway pressure (CPAP) is the most effective treatment | [[Image:CPAP.png|right|250x200px|https://en.wikipedia.org/wiki/Positive_airway_pressure]]For adults, the use of continuous positive airway pressure ([[Non Invasive Ventilation|CPAP]]) is the most effective treatment | ||
* Adherence to nightly CPAP use can result in near complete resolution of symptoms. | * Adherence to nightly CPAP use can result in near complete resolution of symptoms. | ||
* For patients unable or unwilling to use CPAP or those who will be unable to access electricity reliably, custom fitted and titrated oral appliances can be used to bring the lower jaw forward and relieve airway obstruction. | * For patients unable or unwilling to use CPAP or those who will be unable to access electricity reliably, custom fitted and titrated oral appliances can be used to bring the lower jaw forward and relieve airway obstruction. | ||
| Line 75: | Line 73: | ||
* The primary treatment for obstructive sleep apnea in a child is tonsillectomy and adenoidectomy. The consideration for surgery should be balanced with the severity of symptoms, physical exam, and age. In mild cases, a trial of montelukast and nasal steroids may be enough to reduce the apnea-hypopnea index to goal. | * The primary treatment for obstructive sleep apnea in a child is tonsillectomy and adenoidectomy. The consideration for surgery should be balanced with the severity of symptoms, physical exam, and age. In mild cases, a trial of montelukast and nasal steroids may be enough to reduce the apnea-hypopnea index to goal. | ||
* There are surgical options for adults, but these are usually reserved for severe obstructive sleep apnea and patients unable to tolerate noninvasive treatment modalities due to surgical risks and varying efficacy.<ref name=":0" / | * There are surgical options for adults, but these are usually reserved for severe obstructive sleep apnea and patients unable to tolerate noninvasive treatment modalities due to surgical risks and varying efficacy.<ref name=":0" /> | ||
== Evaluation == | == Evaluation == | ||
* | * Nighttime in-laboratory Level 1 polysomnography (PSG) is the standard gold test for diagnosis of obstructive sleep apnea. During the test, patients are monitored with EEG leads, pulse oximetry, temperature and pressure sensors to detect nasal and oral airflow, respiratory impedance plethysmography or similar resistance belts around the chest and abdomen to detect motion, an ECG lead, and EMG sensors to detect muscle contraction in the chin, chest, and legs. A hypopnea can be based on one of two criteria. It can either be a reduction in airflow of at least 30% for more than 10 seconds associated with at least 4% oxygen desaturation or a reduction in airflow of at least 30% for more than 10 seconds associated with at least 3% oxygen desaturation or an arousal from sleep on EEG.<ref name=":0" /> | ||
* Home sleep tests (HST) have gained popularity due to their relative accessibility and lower cost. They are appropriate for adults with a high pretest probability for sleep apnea and no significant medical comorbidities (advanced congestive heart failure, COPD, and neurologic disorders). These are level 3 sleep tests consisting of pulse oximetry, heart rate monitoring, temperature and pressure sensors to detect nasal and oral airflow, resistance belts around the chest and abdomen to detect motion, and a sensor to detect body position.<ref name=":0" /><ref name="diagnose">Shayeb M, Topfer L, Stafinski T, Pawluk L, Menon D. Diagnostic accuracy of level 3 portable sleep tests versus level 1 polysomnography for sleep-disordered breathing: a systematic review and meta-analysis. Canadian Medical Association Journal 2013; 186(1):E25-E51. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3883848/pdf/18600e25.pdf (accessed 7 April 2016).</ref> | |||
Other testing may include | Other testing may include | ||
*History: possible risk factors, co-morbidities, snoring, and what a normal night of sleep is like to him/her.<ref name="diagnose2">Maurer J. Early diagnosis of sleep related breathing disorders. GMS Current Topics in Otorhinolaryngology- Head and Neck Surgery 2010; 7(3): 1-20. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3199834/ (accessed 7 April 2016).</ref> | *History: possible risk factors, co-morbidities, snoring, and what a normal night of sleep is like to him/her.<ref name="diagnose2">Maurer J. Early diagnosis of sleep related breathing disorders. GMS Current Topics in Otorhinolaryngology- Head and Neck Surgery 2010; 7(3): 1-20. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3199834/ (accessed 7 April 2016).</ref> | ||
| Line 89: | Line 83: | ||
*Clinical Examination: nose, tonsils, palate, tongue, neck circumference, upper airways.<ref name="diagnose2" /> <ref name="diagnose3">Culpepper L, Roth T. Recognizing and managing obstructive sleep apnea in primary care. Prim Care Companion J Clin Psychiatry 2009; 11(6): 330-338. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805569/ (accessed 9 April 2016)</ref> Findings are predominantly inconclusive and requires training for proper assessment.<ref name="diagnose2" /> | *Clinical Examination: nose, tonsils, palate, tongue, neck circumference, upper airways.<ref name="diagnose2" /> <ref name="diagnose3">Culpepper L, Roth T. Recognizing and managing obstructive sleep apnea in primary care. Prim Care Companion J Clin Psychiatry 2009; 11(6): 330-338. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805569/ (accessed 9 April 2016)</ref> Findings are predominantly inconclusive and requires training for proper assessment.<ref name="diagnose2" /> | ||
*Questionnaires: Epworth Sleepiness Score (ESS) for daytime sleepiness; Berlin questionnaire for common OSA risk factors and symptoms.<ref name="diagnose2" /> | *Questionnaires: Epworth Sleepiness Score (ESS) for daytime sleepiness; Berlin questionnaire for common OSA risk factors and symptoms.<ref name="diagnose2" /> | ||
*Oximetry: | *Oximetry: analyse oxygen saturation of haemoglobin to help identify individuals unlikely to have OSA.<ref name="diagnose3" /> | ||
== | == Morbidities associated with OSA == | ||
* OSA induced biological changes include intermittent hypoxia, intermittent hypercapnia, intrathoracic pressure changes, sympathetic activation and sleep fragmentation. | |||
* OSA can cause metabolic dysregulation, endothelial dysfunction, systemic inflammation, oxidative stress and hypercoagulation, and neurohumoral changes. | |||
* There is evidence suggesting that OSA is independently associated with metabolic syndrome. | |||
* OSA has been shown to increase the risk for systemic hypertension, [[Pulmonary Hypertension|pulmonary vascular disease]], [[Coronary Artery Disease (CAD)|ischemic heart disease]], cerebral vascular disease, [[Heart Failure|congestive heart failure]] and [[Heart Arrhythmias: Assessment|arrhythmias]]<ref>Vijayan VK. [https://www.medscape.com/viewarticle/775550 Morbidities associated with obstructive sleep apnea.] Expert review of respiratory medicine. 2012 Oct 1;6(5):557-66.Available from:https://www.medscape.com/viewarticle/775550 (last accessed 6.10.2020)</ref><sup></sup><sup></sup><sup></sup><sup></sup> | |||
== Physical Therapy Management == | |||
== | |||
Although there is little research providing sound evidence based physical therapy interventions for OSA at this time, it often goes undiagnosed providing opportunities for physical therapists to identify, educate and refer patients who present with signs and symptoms of OSA. | |||
Undiagnosed OSA is associated with increased risk of hypertension, cardiovascular disease, motor vehicle accidents and reduced quality of life<ref name="prevalence">Young T, Peppard P, Gottlieb D. Epidemiology of Obstructive Sleep Apnea. Am J Respir Crit Care Med 2002;165(9):1217-1239. http://www.atsjournals.org/doi/full/10.1164/rccm.2109080#.Vu73OZMrKYU (accessed 20 March 2016).</ref>. | |||
Physical Therapists can educate patients on OSA: | Physical Therapists can educate patients on OSA: | ||
* Signs and symptoms | |||
* Risk factors | |||
* Associated co-morbidities | |||
* How to get diagnosed/tested | |||
* Risks of undiagnosed OS | |||
=== '''Aerobic Exercise''' === | |||
Studies show significant effect of exercise in reducing the severity of sleep apnea in patients with OSA with minimal changes in body weight. The interventions typically involved aerobic activities for 30 minutes minimum on 3-5 days a week. The significant effects of exercise on cardiorespiratory fitness, daytime sleepiness, and sleep efficiency indicate the potential value of exercise in the management of OSA<ref name=":1">Iftikhar IH, Kline CE, Youngstedt SD. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4216726/ Effects of exercise training on sleep apnea: a meta-analysis.] Lung. 2014 Feb 1;192(1):175-84.Available from;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4216726/ (last accessed 6.10.2020)</ref>. | |||
An example of physiotherapy intervention | |||
* Supervision of 150 min/week of aerobic exercise (treadmill, elliptical trainer, or recumbent bicycle), performed at 60 % of heart rate reserve, spread across 4 days/week for 12 week<ref name=":1" /> | |||
< | * On 2 days/week for 12 week, aerobic exercise was followed by resistance exercise, consisting of 2 sets of 10–12 repetitions for 8 different exercises<ref name=":1" /> | ||
< | === '''Tongue Exercises''' === | ||
Physiotherapeutic treatment eg muscular exercises could have a place in the treatment ofOSA, particularly in the mild cases. This treatment could help to prevent the muscular hypotonia that develops progressively in the OSA<ref>Lequeux T, Chantrain G, Bonnand M, Chelle AJ, Thill MP. Physiotherapy in obstructive sleep apnea syndrome: preliminary results. European Archives of Oto-Rhino-Laryngology and Head & Neck. 2005 Jun 1;262(6):501-3.AVAILABLE FROM;https://www.researchgate.net/publication/8104544_Physiotherapy_in_obstructive_sleep_apnea_syndrome_Preliminary_results<nowiki/>(LAST ACCESSED 6.10.2020)</ref>. | |||
Below shows examples of exercises For Obstructive Sleep Apnea | |||
<br> | EXERCISES FOR THE TONGUE<br>TONGUE BRUSHING<br>Method:<br>1. With your toothbrush brush the top and sides of your tongue, while your tongue is sitting on the floor of your mouth.<br>2. Repeat the individual sections 5 times each.<br>3. Complete the exercise three times daily.<br>Purpose – to strengthen the tongue muscles-with the added advantage of maintaining great oral hygiene! | ||
[[File:Tongue_exercise2.png|right|frameless|599x599px]] | |||
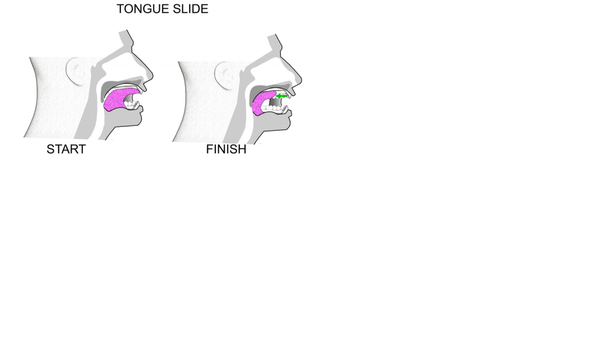
TONGUE SLIDE<br>Method:<br>1. Looking straight ahead, position the tip of your tongue against the back of your top, front teeth.<br>2. Slide your tongue backward.<br>3. Repeat 10 times.<br>Purpose – to tone and strengthen the tongue and throat muscles. | |||
[[File:Tongue_Force.png|right|frameless|400x400px]] | |||
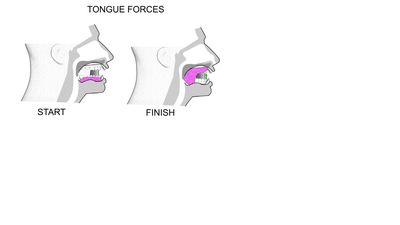
TONGUE FORCES<br>Method:<br>1. Forcibly suck your tongue upward until the whole tongue is against your palate.<br>2. Hold this position for 4 seconds.<br>3. Repeat 5 times.<br>Method:<br>1. Force the back of your tongue downward until the whole tongue is resting on the floor of your mouth.<br>2. Keep the tip of your tongue touching the back of your lower teeth.<br>3. Hold for 4 seconds.<br>4. Repeat 5 times.<br>Purpose - both of these exercises strengthen the tongue and tone your soft palate. | |||
[[File:Tongue_Press.png|right|frameless|400x400px]] | |||
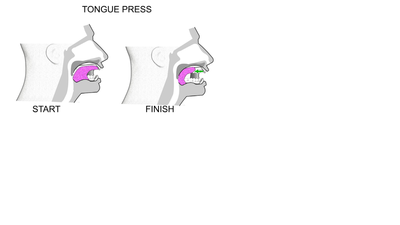
TONGUE PRESS<br>Method:<br>1. Push your tongue against your hard palate (the top and front of your mouth).<br>2. Do this for 5 seconds.<br>3. Slide your tongue backward to the back of your mouth.<br>4. The initial third of your tongue should be against your hard palate, not just the tip.<br>5. Keep your jaw open throughout the exercise.<br>6. Refrain from biting down - keep your teeth apart.<br>7. Repeat this movement 10 times.<br>8. Repeat 4 times a day.<br>Purpose – to strengthen the genioglossus (the main muscle used for sticking your tongue out), and to increase the strength in the hyoid muscles and bone. The hyoid bone is located in the centre of the neck. It sits between the chin and thyroid cartilage.<br>The exercise assists by putting the hyoid bone in the correct position and keeping it there1.<br>The hyoid bone is a free moving, u-shaped bone in the neck. The volume of the tongue should reduce too. | |||
=== Breathing Exercise === | |||
[[File:9445-hic-diaphragmatic-breathing-2.jpg|thumb|Diaphragmatic Breathing]] | |||
Respiratory training was found to have significant effect of sleep apnea, as shown by in the 2021 systematic review were patients with sleep apnea that underwent respiratory retraining had a measurable improvement in apnea-hypopnea indexes (AHI). <ref>Cavalcante-Leão BL, de Araujo CM, Ravazzi GC, Basso IB, Guariza-Filho O, Taveira KV, Santos RS, Stechman-Neto J, Zeigelboim BS. Effects of respiratory training on obstructive sleep apnea: Systematic review and meta-analysis. Sleep and Breathing. 2021 Dec 1:1-1.</ref> | |||
There is a diversity of breathing retraining methods that were found to improve sleep apnea including: inspiratory resistance training and diaphragmatic breathing.<ref name=":2">Courtney R. Breathing retraining in sleep apnoea: A review of approaches and potential mechanisms. Sleep and Breathing. 2020 Dec;24:1315-25.</ref> Also, they were found helpful in decreasing fatigue and day time sleepiness. <ref>Serçe S, Ovayolu Ö, Bayram N, Ovayolu N, Kul S. The effect of breathing exercise on daytime sleepiness and fatigue among patients with obstructive sleep apnea syndrome. Journal of Breath Research. 2022 Aug 25;16(4):046006.</ref> | |||
[[ | '''[[Respiratory Muscle Training|Inspiratory resistance training]]''' involves using an inspiratory threshold training device, examples for these devices include POWER breathe.<ref>Vranish JR, Bailey EF. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4863204/ Inspiratory muscle training improves sleep and mitigates cardiovascular dysfunction in obstructive sleep apnea.] Sleep. 2016 Jun 1;39(6):1179-85.</ref> | ||
< | '''[[Diaphragmatic Breathing Exercises|Diaphragmatic breathing]]''' involves patients taking slow and deep breathes, inhaling through their nose and exhaling through their mouth, placing a hand on their abdomen aiming to lifting it during inspiration.<ref>Yokogawa M, Kurebayashi T, Ichimura T, Nishino M, Miaki H, Nakagawa T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5909014/ Comparison of two instructions for deep breathing exercise: non-specific and diaphragmatic breathing.] Journal of physical therapy science. 2018;30(4):614-8.</ref> | ||
Regular practice of breathing control activities such as singing and playing wind instruments may also be helpful for people with sleep apnea.<ref name=":2" /> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
* [[Asthma]] | |||
* Central sleep apnea | |||
* [[COPD (Chronic Obstructive Pulmonary Disease)|Chronic Obstructive Pulmonary Disease]] | |||
* | * [[Depression]] | ||
* [[Gastroesophageal Reflux Disease|Gastroesophageal reflux]] | |||
* Hypothyroidism | |||
* | * [[Narcolepsy]] | ||
* | * Periodic limb movement disorder<ref name=":0" /> | ||
*Hypothyroidism | |||
*Narcolepsy | |||
* | |||
== Case Reports/ Case Studies == | == Case Reports/ Case Studies == | ||
# Daoulah A, Ocheltree S, Al-Faifi S, Ahmed W, Asrar F, Lotfi A. Sleep apnea and severe bradyarrhythmia – an alternative treatment option: a case report. J Med Case Reports 2015; 9(1): 113-117. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4437673/ (OSA and Bradyarrhythmia) | |||
# Guimarães T, Colen S, Cunali P, Rossi R, Dal-Fabbro C, Ferraz O, et al. Treatment of obstructive sleep apnea with mandibular advancement appliance over prostheses: A case report. Sleep Science 2015;8(2):103-106.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4608885/ (Treatment of OSA with Mandibular Appliance) | |||
# Fang H, Miao N, Chen C, Sithole T, Chung M. Risk of Cancer in Patients with Insomnia, Parasomnia, and Obstructive Sleep Apnea: A Nationwide Nested Case-Control Study. J Cancer 2015;6(11):1140-1147. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4615350/ (OSA and Cancer) | |||
# Cadby G, McArdle N, Briffa T, Hillman D, Simpson L, Knuiman M, et al. Severity of OSA Is an Independent Predictor of Incident Atrial Fibrillation Hospitalization in a Large Sleep-Clinic Cohort Chest. 2015;148(4):945-952.http://www.sciencedirect.com/science/article/pii/S0012369215502833 (OSA and A-fib) | |||
# Meuleners L, Fraser M, Govorko M, Stevenson M. Obstructive Sleep Apnea, Health-Related Factors, and Long Distance Heavy Vehicle Crashes in Western Australia: A Case Control Study. Journal of Clinical Sleep Medicine 2015; 11(4): 413-418.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4365454/ (OSA and MVA) | |||
== References == | == References == | ||
Latest revision as of 23:34, 29 April 2023
Original Editors - Ylice Bridges and Irena Tran
Top Contributors - Irena Tran, Ylice Bridges, Lucinda hampton, Venugopal Pawar, Kim Jackson, 127.0.0.1, Elaine Lonnemann, WikiSysop, Adam Vallely Farrell, Lilian Ashraf and Admin
Definition/Description[edit | edit source]
Sleep apnea is a disorder in which breathing is interrupted or paused during sleep. The pauses in breathing can last a few seconds to minutes and are long enough to:
- Disrupt sleep
- Decrease level of oxygen in the blood
- Increase level of carbon dioxide in the blood
These breathing interruptions can occur more than 30 times an hour and significantly impair the quality of sleep. Because of this, sleep apnea is a leading cause of excessive daytime sleepiness.[1]
There are three types of sleep apnea: central, obstructive and mixed. Obstructive sleep apnea is the most common and the main focus of this article.
- Obstructive sleep apnea (OSA) is caused by repeated partial or complete obstruction of the upper airway that diminishes or stops breathing.
- Central sleep apnea occurs when the brain is less sensitive to changes in carbon dioxide levels in the blood and fails to send signals to the respiratory muscles to breathe deeper.
- Mixed sleep apnea is a combination of both obstructive and central sleep apnea episodes.[1]
Aetiology[edit | edit source]
Sleep apnea occurs when there is not enough space to accommodate sufficient airflow in a portion of the upper airway during sleep.
- When muscle tone is decreased, the result is a repetitive total or partial collapse of the airway.
- In children, the most common cause of obstructive sleep apnea is enlarged tonsils and/or adenoids.
- In adults, it is most commonly associated with obesity, male sex, and advancing age.[2]
Factors that contribute to airway obstruction are:[3]
- Obesity
- Large neck circumference
- Large tongue or tonsils
- Narrow airway due to bony structures of head and neck
- Taking sedative medication
- Drinking alcohol
- Smoking
- Nasal congestion
Medical disorders associated with OSA include:
- Stroke
- Hypothyroidism
- Metabolic syndrome
- Acromegaly
- Neurological disorders (eg myasthenia gravis)[2]
Epidemiology[edit | edit source]
- In the United States, it has been reported that 4% of men and 2% of women meet criteria for obstructive sleep apnea.
- More recently, prevalence has been reported to be as high as 14% of men and 5% of women in the United States.
- Prevalence is higher in Hispanic, African American, and Asian populations[2].
- Prevalence also increases with age, and when individuals reach 50 years of age or more, there are as many women as men who develop the disorder.
- Genetics and abnormalities or conditions of the craniofacial morphology also increase the likelihood of OSA. Individuals with a first-degree relative with OSA were at a 1.5-2x increased risk of developing OSA[2].[4]
- OSA is common in individuals who spend long periods of time sitting and driving, such as commercial truck drivers.[5]
Characteristics/Clinical Presentation[edit | edit source]
Typical adult obstructive sleep apnea patient
- Overweight or obese middle-aged male or postmenopausal female with excessive daytime sleepiness and loud nightly snoring.
- May also complain of waking to gasp for breath or choking, sleep maintenance insomnia, night sweats, nighttime reflux, and nocturia in the absence of excessive nighttime liquid intake.
- Typically larger than average neck circumference (17 inches in males) with crowded oropharynx and large tongue.
- Retrognathism (an abnormal posterior positioning of the maxilla or mandible relative to the facial skeleton and soft tissues) may be present.
Patients with refractory atrial fibrillation, resistant hypertension, and history of a stroke should be screened for sleep apnea regardless of symptoms[2]
Typical child with obstructive sleep apnea
- Loud nightly snoring
- May be hyperactive rather than sleepy
- May have academic difficulties.
- These children can be incorrectly diagnosed with attention deficit hyperactivity disorder (ADHD).
- Night sweats, nighttime reflux, sleep maintenance insomnia, restless sleep with frequent limb movements, and secondary nocturnal enuresis may also be present.
- A physical exam is often notable for adenoidal facies ( long, open-mouthed face of children with adenoid hypertrophy[6]), tonsillar hypertrophy, hyponasal speech, and high arched palate.
Patients with Down syndrome and any other condition associated with hypotonia should be screened for obstructive sleep apnea regardless of symptoms.[2]
Treatment[edit | edit source]
For adults, the use of continuous positive airway pressure (CPAP) is the most effective treatment
- Adherence to nightly CPAP use can result in near complete resolution of symptoms.
- For patients unable or unwilling to use CPAP or those who will be unable to access electricity reliably, custom fitted and titrated oral appliances can be used to bring the lower jaw forward and relieve airway obstruction.
- Severe obstructive sleep apnea can be treated with BiPAP as well and is better tolerated by patients who require higher pressure settings (greater than 15 cm to 20 cm H2O).
- For all patients, it is important to address any concomitant nasal obstruction with nasal steroids for allergic rhinitis or surgically for nasal valve collapse.
- For obstructive sleep apnea with a strong positional component. Positioning devices to keep a patient on his or her side can be an option.
- Weight loss is recommended and can often decrease the severity of obstructive sleep apnea, it is not usually curative by itself.
- The primary treatment for obstructive sleep apnea in a child is tonsillectomy and adenoidectomy. The consideration for surgery should be balanced with the severity of symptoms, physical exam, and age. In mild cases, a trial of montelukast and nasal steroids may be enough to reduce the apnea-hypopnea index to goal.
- There are surgical options for adults, but these are usually reserved for severe obstructive sleep apnea and patients unable to tolerate noninvasive treatment modalities due to surgical risks and varying efficacy.[2]
Evaluation[edit | edit source]
- Nighttime in-laboratory Level 1 polysomnography (PSG) is the standard gold test for diagnosis of obstructive sleep apnea. During the test, patients are monitored with EEG leads, pulse oximetry, temperature and pressure sensors to detect nasal and oral airflow, respiratory impedance plethysmography or similar resistance belts around the chest and abdomen to detect motion, an ECG lead, and EMG sensors to detect muscle contraction in the chin, chest, and legs. A hypopnea can be based on one of two criteria. It can either be a reduction in airflow of at least 30% for more than 10 seconds associated with at least 4% oxygen desaturation or a reduction in airflow of at least 30% for more than 10 seconds associated with at least 3% oxygen desaturation or an arousal from sleep on EEG.[2]
- Home sleep tests (HST) have gained popularity due to their relative accessibility and lower cost. They are appropriate for adults with a high pretest probability for sleep apnea and no significant medical comorbidities (advanced congestive heart failure, COPD, and neurologic disorders). These are level 3 sleep tests consisting of pulse oximetry, heart rate monitoring, temperature and pressure sensors to detect nasal and oral airflow, resistance belts around the chest and abdomen to detect motion, and a sensor to detect body position.[2][7]
Other testing may include
- History: possible risk factors, co-morbidities, snoring, and what a normal night of sleep is like to him/her.[8]
- Indices: AHI (apnea-hypopnea index), RDI (respiratory disturbance index)[3]
- Clinical Examination: nose, tonsils, palate, tongue, neck circumference, upper airways.[8] [9] Findings are predominantly inconclusive and requires training for proper assessment.[8]
- Questionnaires: Epworth Sleepiness Score (ESS) for daytime sleepiness; Berlin questionnaire for common OSA risk factors and symptoms.[8]
- Oximetry: analyse oxygen saturation of haemoglobin to help identify individuals unlikely to have OSA.[9]
Morbidities associated with OSA[edit | edit source]
- OSA induced biological changes include intermittent hypoxia, intermittent hypercapnia, intrathoracic pressure changes, sympathetic activation and sleep fragmentation.
- OSA can cause metabolic dysregulation, endothelial dysfunction, systemic inflammation, oxidative stress and hypercoagulation, and neurohumoral changes.
- There is evidence suggesting that OSA is independently associated with metabolic syndrome.
- OSA has been shown to increase the risk for systemic hypertension, pulmonary vascular disease, ischemic heart disease, cerebral vascular disease, congestive heart failure and arrhythmias[10]
Physical Therapy Management[edit | edit source]
Although there is little research providing sound evidence based physical therapy interventions for OSA at this time, it often goes undiagnosed providing opportunities for physical therapists to identify, educate and refer patients who present with signs and symptoms of OSA.
Undiagnosed OSA is associated with increased risk of hypertension, cardiovascular disease, motor vehicle accidents and reduced quality of life[11].
Physical Therapists can educate patients on OSA:
- Signs and symptoms
- Risk factors
- Associated co-morbidities
- How to get diagnosed/tested
- Risks of undiagnosed OS
Aerobic Exercise[edit | edit source]
Studies show significant effect of exercise in reducing the severity of sleep apnea in patients with OSA with minimal changes in body weight. The interventions typically involved aerobic activities for 30 minutes minimum on 3-5 days a week. The significant effects of exercise on cardiorespiratory fitness, daytime sleepiness, and sleep efficiency indicate the potential value of exercise in the management of OSA[12].
An example of physiotherapy intervention
- Supervision of 150 min/week of aerobic exercise (treadmill, elliptical trainer, or recumbent bicycle), performed at 60 % of heart rate reserve, spread across 4 days/week for 12 week[12]
- On 2 days/week for 12 week, aerobic exercise was followed by resistance exercise, consisting of 2 sets of 10–12 repetitions for 8 different exercises[12]
Tongue Exercises[edit | edit source]
Physiotherapeutic treatment eg muscular exercises could have a place in the treatment ofOSA, particularly in the mild cases. This treatment could help to prevent the muscular hypotonia that develops progressively in the OSA[13].
Below shows examples of exercises For Obstructive Sleep Apnea
EXERCISES FOR THE TONGUE
TONGUE BRUSHING
Method:
1. With your toothbrush brush the top and sides of your tongue, while your tongue is sitting on the floor of your mouth.
2. Repeat the individual sections 5 times each.
3. Complete the exercise three times daily.
Purpose – to strengthen the tongue muscles-with the added advantage of maintaining great oral hygiene!
TONGUE SLIDE
Method:
1. Looking straight ahead, position the tip of your tongue against the back of your top, front teeth.
2. Slide your tongue backward.
3. Repeat 10 times.
Purpose – to tone and strengthen the tongue and throat muscles.
TONGUE FORCES
Method:
1. Forcibly suck your tongue upward until the whole tongue is against your palate.
2. Hold this position for 4 seconds.
3. Repeat 5 times.
Method:
1. Force the back of your tongue downward until the whole tongue is resting on the floor of your mouth.
2. Keep the tip of your tongue touching the back of your lower teeth.
3. Hold for 4 seconds.
4. Repeat 5 times.
Purpose - both of these exercises strengthen the tongue and tone your soft palate.
TONGUE PRESS
Method:
1. Push your tongue against your hard palate (the top and front of your mouth).
2. Do this for 5 seconds.
3. Slide your tongue backward to the back of your mouth.
4. The initial third of your tongue should be against your hard palate, not just the tip.
5. Keep your jaw open throughout the exercise.
6. Refrain from biting down - keep your teeth apart.
7. Repeat this movement 10 times.
8. Repeat 4 times a day.
Purpose – to strengthen the genioglossus (the main muscle used for sticking your tongue out), and to increase the strength in the hyoid muscles and bone. The hyoid bone is located in the centre of the neck. It sits between the chin and thyroid cartilage.
The exercise assists by putting the hyoid bone in the correct position and keeping it there1.
The hyoid bone is a free moving, u-shaped bone in the neck. The volume of the tongue should reduce too.
Breathing Exercise[edit | edit source]
Respiratory training was found to have significant effect of sleep apnea, as shown by in the 2021 systematic review were patients with sleep apnea that underwent respiratory retraining had a measurable improvement in apnea-hypopnea indexes (AHI). [14]
There is a diversity of breathing retraining methods that were found to improve sleep apnea including: inspiratory resistance training and diaphragmatic breathing.[15] Also, they were found helpful in decreasing fatigue and day time sleepiness. [16]
Inspiratory resistance training involves using an inspiratory threshold training device, examples for these devices include POWER breathe.[17]
Diaphragmatic breathing involves patients taking slow and deep breathes, inhaling through their nose and exhaling through their mouth, placing a hand on their abdomen aiming to lifting it during inspiration.[18]
Regular practice of breathing control activities such as singing and playing wind instruments may also be helpful for people with sleep apnea.[15]
Differential Diagnosis[edit | edit source]
- Asthma
- Central sleep apnea
- Chronic Obstructive Pulmonary Disease
- Depression
- Gastroesophageal reflux
- Hypothyroidism
- Narcolepsy
- Periodic limb movement disorder[2]
Case Reports/ Case Studies[edit | edit source]
- Daoulah A, Ocheltree S, Al-Faifi S, Ahmed W, Asrar F, Lotfi A. Sleep apnea and severe bradyarrhythmia – an alternative treatment option: a case report. J Med Case Reports 2015; 9(1): 113-117. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4437673/ (OSA and Bradyarrhythmia)
- Guimarães T, Colen S, Cunali P, Rossi R, Dal-Fabbro C, Ferraz O, et al. Treatment of obstructive sleep apnea with mandibular advancement appliance over prostheses: A case report. Sleep Science 2015;8(2):103-106.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4608885/ (Treatment of OSA with Mandibular Appliance)
- Fang H, Miao N, Chen C, Sithole T, Chung M. Risk of Cancer in Patients with Insomnia, Parasomnia, and Obstructive Sleep Apnea: A Nationwide Nested Case-Control Study. J Cancer 2015;6(11):1140-1147. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4615350/ (OSA and Cancer)
- Cadby G, McArdle N, Briffa T, Hillman D, Simpson L, Knuiman M, et al. Severity of OSA Is an Independent Predictor of Incident Atrial Fibrillation Hospitalization in a Large Sleep-Clinic Cohort Chest. 2015;148(4):945-952.http://www.sciencedirect.com/science/article/pii/S0012369215502833 (OSA and A-fib)
- Meuleners L, Fraser M, Govorko M, Stevenson M. Obstructive Sleep Apnea, Health-Related Factors, and Long Distance Heavy Vehicle Crashes in Western Australia: A Case Control Study. Journal of Clinical Sleep Medicine 2015; 11(4): 413-418.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4365454/ (OSA and MVA)
References[edit | edit source]
- ↑ 1.0 1.1 Strohl KP. Sleep Apnea [Internet]. Kenilworth (NJ): Merck & Co., Inc.; c2016 [cited 2016 Mar 30]. Available from: http://www.merckmanuals.com/home/lung-and-airway-disorders/sleep-apnea/sleep-apnea
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Slowik JM, Collen JF. Obstructive Sleep Apnea.(2019)Available from:https://www.ncbi.nlm.nih.gov/books/NBK459252/ (last accessed 5.10.2020)
- ↑ 3.0 3.1 Downey III R, Rowley J, Wickramasinghe H, Gold P. Obstructive Sleep Apnea Differential Diagnoses. Emedicinemedscapecom. 2016. Available at: http://emedicine.medscape.com/article/295807-differential. Accessed April 9, 2016.
- ↑ Lam J, Sharma S, Lam B. Obstructive sleep apnea: Definitions, epidemiology & natural history. Indian J Med Res 2010;131:165-170. http://pharexmedics.com/wp-content/uploads/2015/11/sleepapnea_ebook.pdf (accessed 3 April 2016).
- ↑ Epstein L, Kristo D, Strollo Jr. P, Friedman N, Malhotra A, Patil S, et al. Clinical Guideline for the Evaluation, Management and Long-term Care of Obstructive Sleep Apnea in Adults. Journal of Clinical Sleep Medication 2009; 5(3): 263-276. http://pharexmedics.com/wp-content/uploads/2015/11/sleepapnea_ebook.pdf (accessed 3 April 2016).
- ↑ Radiopedia Adenoid Facies Available from:https://radiopaedia.org/articles/adenoid-facies-2 (last accessed 6.10.2020)
- ↑ Shayeb M, Topfer L, Stafinski T, Pawluk L, Menon D. Diagnostic accuracy of level 3 portable sleep tests versus level 1 polysomnography for sleep-disordered breathing: a systematic review and meta-analysis. Canadian Medical Association Journal 2013; 186(1):E25-E51. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3883848/pdf/18600e25.pdf (accessed 7 April 2016).
- ↑ 8.0 8.1 8.2 8.3 Maurer J. Early diagnosis of sleep related breathing disorders. GMS Current Topics in Otorhinolaryngology- Head and Neck Surgery 2010; 7(3): 1-20. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3199834/ (accessed 7 April 2016).
- ↑ 9.0 9.1 Culpepper L, Roth T. Recognizing and managing obstructive sleep apnea in primary care. Prim Care Companion J Clin Psychiatry 2009; 11(6): 330-338. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2805569/ (accessed 9 April 2016)
- ↑ Vijayan VK. Morbidities associated with obstructive sleep apnea. Expert review of respiratory medicine. 2012 Oct 1;6(5):557-66.Available from:https://www.medscape.com/viewarticle/775550 (last accessed 6.10.2020)
- ↑ Young T, Peppard P, Gottlieb D. Epidemiology of Obstructive Sleep Apnea. Am J Respir Crit Care Med 2002;165(9):1217-1239. http://www.atsjournals.org/doi/full/10.1164/rccm.2109080#.Vu73OZMrKYU (accessed 20 March 2016).
- ↑ 12.0 12.1 12.2 Iftikhar IH, Kline CE, Youngstedt SD. Effects of exercise training on sleep apnea: a meta-analysis. Lung. 2014 Feb 1;192(1):175-84.Available from;https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4216726/ (last accessed 6.10.2020)
- ↑ Lequeux T, Chantrain G, Bonnand M, Chelle AJ, Thill MP. Physiotherapy in obstructive sleep apnea syndrome: preliminary results. European Archives of Oto-Rhino-Laryngology and Head & Neck. 2005 Jun 1;262(6):501-3.AVAILABLE FROM;https://www.researchgate.net/publication/8104544_Physiotherapy_in_obstructive_sleep_apnea_syndrome_Preliminary_results(LAST ACCESSED 6.10.2020)
- ↑ Cavalcante-Leão BL, de Araujo CM, Ravazzi GC, Basso IB, Guariza-Filho O, Taveira KV, Santos RS, Stechman-Neto J, Zeigelboim BS. Effects of respiratory training on obstructive sleep apnea: Systematic review and meta-analysis. Sleep and Breathing. 2021 Dec 1:1-1.
- ↑ 15.0 15.1 Courtney R. Breathing retraining in sleep apnoea: A review of approaches and potential mechanisms. Sleep and Breathing. 2020 Dec;24:1315-25.
- ↑ Serçe S, Ovayolu Ö, Bayram N, Ovayolu N, Kul S. The effect of breathing exercise on daytime sleepiness and fatigue among patients with obstructive sleep apnea syndrome. Journal of Breath Research. 2022 Aug 25;16(4):046006.
- ↑ Vranish JR, Bailey EF. Inspiratory muscle training improves sleep and mitigates cardiovascular dysfunction in obstructive sleep apnea. Sleep. 2016 Jun 1;39(6):1179-85.
- ↑ Yokogawa M, Kurebayashi T, Ichimura T, Nishino M, Miaki H, Nakagawa T. Comparison of two instructions for deep breathing exercise: non-specific and diaphragmatic breathing. Journal of physical therapy science. 2018;30(4):614-8.