Rehabilitation of Burns in Disasters and Conflicts
Original Editors - Add your name/s here if you are the original editor/s of this page. User Name
Top Contributors - Stacy Schiurring, Naomi O'Reilly, Rishika Babburu, Kim Jackson, Jess Bell, Chelsea Mclene and Carin Hunter
Introduction[edit | edit source]
Burn injuries are complex and involve injuries that require immediate and specialised interventions. Burn injuries commonly require a prolonged rehabilitation process to return to functional independence, often with adaptation or compensatory training in the long term. These patients will require both physical and psychological support throughout their rehabilitation process, this is especially true when an injury occurs as a result of disaster or conflict.[1]
Acutely, rehabilitation will be supportive of the medical needs of the patient. However, rehabilitation plays an important role in the acute phase to prepare the patient both physically and mentally for the therapy to come. This article will focus on the physical rehabilitation of patients who have had a burn injury but will include important wound care considerations with regards to mobility and positioning.
Rehabilitation for burn injuries starts from day one of the injury, right through the period of scar maturation, and often for years after the injury, especially relevant to the prevention of contractures and in children where growth is not complete.[1]
Burn Overview[edit | edit source]
Please read the linked article for background knowledge on the anatomy and physiology of the skin. Understanding the structure of the skin is an important part of burn classification.
Please read the linked article for background knowledge of wound healing. Understanding the expected timeline of wound healing and the body's response to injury is vital in patient education and differentiating normal wound healing from the signs and symptoms of infection. This article also contains links to wound assessment and wound debridement to better understand these procedures. Wound care is a specialised skill and should not be performed without the proper training. Physiotherapists can specialise in wound management with advanced training.
Types of Burns[edit | edit source]
Burns injuries have several common causes which include but are not limited to:
- Thermal burns: due to heat sources that raise the temperature of the skin and surrounding tissues. This causes tissue cell death or charring. Heat sources can include hot metals, scalding liquids, steam, and flames. Thermal burns can also be caused by exposure to extreme colds such as a frostbite injury.
- Radiation burns: due to prolonged exposure to ultraviolet rays or to other sources of radiation. Radiation sources can include the sun, X-rays.
- Chemical burns: due to strong acids, alkalies, detergents, or solvents which come into contact with the skin.
- Electrical burns: due to electrical current, either alternating current (AC) or direct current (DC) coming into contact with the body.
Classification of Burns[edit | edit source]
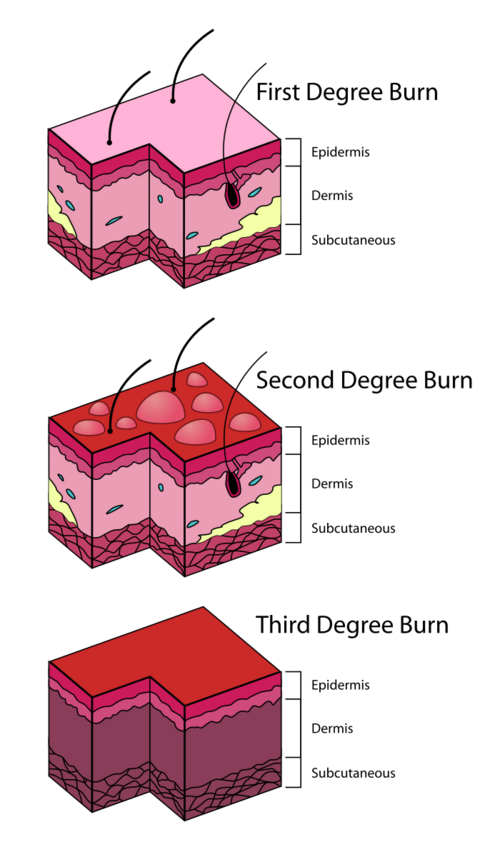
| Depth of burn | Tissues destroyed | Burn Appearance | Pain Sensitivity |
|---|---|---|---|
| Superficial
i.e. 1st degree burn |
Outer layer of epidermis |
|
Painful |
| Superficial Partial Thickness (SPT)
i.e. 2nd degree burn: superficial/intermediate |
|
|
Very painful and hypersensitive |
| Deep Partial Thickness (DPT)
i.e. 2nd degree burn: deep |
|
|
Less sensitive to pain due to destroyed nerve endings |
| Full Thickness Burn (FTB)
i.e. 3rd degree burn |
All skin layers damaged or destroyed; fat or bone may be visible. |
|
No pain from lost cutaneous pain receptors BUT situation is often painful for the patient. |
Below is a video which goes into greater detail on burn classification and staging. It also includes examples of the burn's appearance.
[3]Next is a video of the capillary refill test being performed on a healthy finger. Note the blanching of the skin when pressure is removed and how long it takes for the colour to return.
[4]Burn Assessment[edit | edit source]
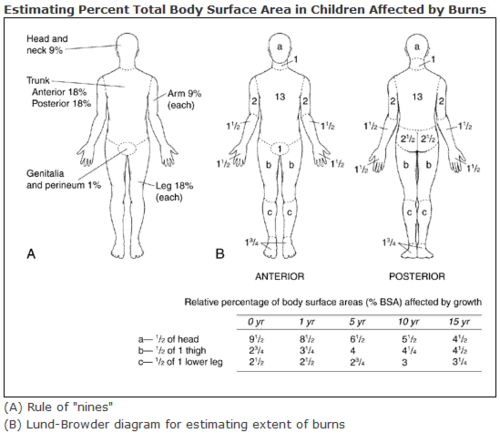
Total Body Surface Area (TBSA) burned: the area of the body that is affected by a burn. This is expressed in a percentage, for example if a chart read 20% TBSA burn, this would mean 20% of the total surface area of that patient was affected by a burn.
- Different forms are used for adults and children
- For adults, a major burn involves 30% TBSA or more, children 20% TBSA or more.
- Location and type of burn also influence both the severity and functional implications. For example: deep burns on the hands records as a small TBSA but has a huge functional impact for that patient.
Immediate Medical Care Needs[edit | edit source]
In the acute care phase of major burns injuries, medical management will include:
- Fluid resuscitation[1]
- Airway management[1][5]
- Wound debridement and or surgical procedures such as escharotomy or fasciotomy[1]
- Pain management [5]
Acute Rehabilitation for Burn Injury[edit | edit source]
Acute Burn Injury Mobility Precautions[edit | edit source]
- Burns encountered in conflict zones or disaster areas are often combined with trauma injuries such as fractures[1], internal injuries, or brain and or head injuries. Appropriate mobility precautions such as extremity weightbearing status, spinal and or cervical immobilisation, or bedrest needs in the case of internal organ injuries or bleeding need to be determined with the medical team.
- If shrapnel is present in the burn/wound which cannot be easily removed due to risk of further tissue damage, it may be left in place.[1] Defer to medical team regarding mobilisation of affected area in these cases.
- Pain will develop following surgical debridements[1], plan accordingly with pain medication schedule.
Acute Rehabilitation[edit | edit source]
Rehabilitation should begin as soon as the patient is medically stable.Acute Rehabilitation for Burn Injury focuses on:
- Respiratory care
- Oedema management
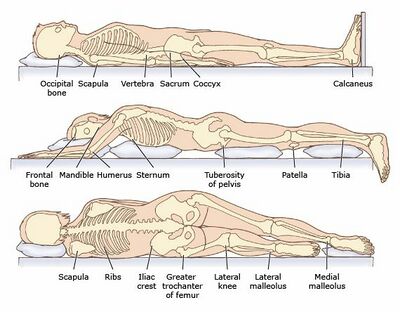
- Positioning, splinting and pressure relief
- Early mobility
- Progressive graded exercises
- Maintaining functional independence
- Patient and caregiver education[1]
Respiratory Care[edit | edit source]
The aims of physiotherapy for respiratory care involve: airway maintenance, secretion removal, gas exchange improvement, prevention and or treatment of atelectasis, and maintenance of thoracic expansion.[1]
For deeper knowledge on these topics please read about chest physiotherapy.
Oedema Management[edit | edit source]
Oedema is a normal response to injury and an important step in wound healing. However, excessive oedema can negatively effect wound healing.
Acute oedema management includes:
- appropriate extremity positioning
- use of muscle pump action through active AROM
- facial oedema requires patient to sit up to at least 45 degrees 24 hours/day
- expect dressings used for oedema management to be firm but allowing for AROM of all joints
Positioning, Splinting, Pressure Relief[edit | edit source]
Patients with burns will typically wish to go into a position of comfort, which is generally a flexion pattern. Developing scar tissue will result in shortened muscle lengths if patients are allows to maintain these positions over time.Proper and correct positioning is essential for contracture prevention. Positioning for contracture prevention should be used prophylactically even when there is no sign of lost ROM upon initial assessment of affected area. Depending on the severity of the burn injury, splinting and positioning programmes may need to be continued for at least six months for optimal results.[1]
Anti-deformity positioning:
- Shoulders: abducted to 90 degrees, horizontally adducted to 20 degrees, encourage external rotation
- Scapula: retracted, depressed, supinated
- Upper extremities: neutral rotation, forearms supinated
- Elbows: extended
- Wrist: 30-40 degrees extension, MP 45-70 degrees flexion, IP extension, thumb abducted and opposed
- Neck: slightly extended, no pillow
- Hips: slight abduction with full extension, block external rotation[1]
Splinting is typically indicated:
- to position extremities for contracture prevention
- to protect grafts or surgical flaps during initial phase of healing
Early Mobility, Exercise, Functional Independence[edit | edit source]
The goal of early mobilisation and therapy interventions after a burn is to maintain functional mobility and endurance while the body heals. The degree of burn will dictate therapy intensity. The areas affected by the burn will require gentle ROM, which should be slow and smooth to decrease associated pain and inflammation with movement.[1]
Education[edit | edit source]
Due to the long healing and rehabilitation timeframe following a burn, patient and caregiver education is of vital importance for successful burn management and rehabilitation.This education and training should include:
- ROM and stretching exercises with special consideration given to patient fear of movement due to pain
- Contracture etiology and prevention
- Functional activities and mobility to include assistive device use
- Positioning and pressure relief techniques
- Splint use and wearing schedule
- Infection control
- Anticipated healing times as patient moves from acute phase into subacute and beyond[1]
Treatment Red Flags[edit | edit source]
Rehabilitation therapists such as physiotherapists often have the most direct contact with their patients. Therefore it is important to monitor these patients for treatment red flags and alert the medical team as appropriate.
- Hypovolemic shock
- Infection: this is the most common cause of death of patients with burns who survive the initial injury.
- Compartment syndrome
- Inadequate pain management[1]
Familiarise yourself with the signs and symptoms of sepsis.
References [edit | edit source]
see adding references tutorial.
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 Lathia C, Skelton P, Clift Z. Early rehabilitation in conflicts and disasters. Handicap International: London, UK. 2020.
- ↑ Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. Burn injury. Nature Reviews Disease Primers. 2020 Feb 13;6(1):1-25.
- ↑ YouTube. Burns: Clinical Estimation – Emergency Medicine | Lecturio. Available from: https://www.youtube.com/watch?v=vCzPNl8EvHM [last accessed 03/03/2022]
- ↑ YouTube. Capillary Refill Test. Available from: https://www.youtube.com/watch?v=n--wFoZFklg [last accessed 02/03/2022]
- ↑ 5.0 5.1 Legrand M, Barraud D, Constant I, Devauchelle P, Donat N, Fontaine M, Goffinet L, Hoffmann C, Jeanne M, Jonqueres J, Leclerc T. Management of severe thermal burns in the acute phase in adults and children. Anaesthesia Critical Care & Pain Medicine. 2020 Apr 1;39(2):253-67.