Proximal Hamstring Tendinopathy: Difference between revisions
mNo edit summary |
No edit summary |
||
| Line 5: | Line 5: | ||
</div> | </div> | ||
= Description = | == Description == | ||
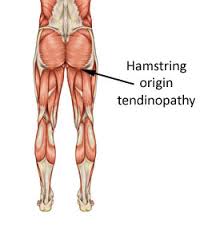
Hamstring origin tendinopathy, also called proximal hamstring tendinopathy or high hamstring tendinopathy, are a group of pathologies of the proximal hamstring tendon. | -Hamstring origin tendinopathy, also called proximal hamstring tendinopathy or high hamstring tendinopathy, are a group of pathologies of the proximal hamstring tendon. | ||
[ | They include tendon degeneration, partial tearing and peritendinous inflammatory reaction.<ref name="p5">Maurice H. Zissen, et al. High Hamstring Tendinopathy: MRI and Ultrasound Imaging and Therapeutic Efficacy of Percutaneous Coorticosteroid Injection [Internet]. American Roentgen Ray Society 2010.Available from: http://www.ajronline.org/doi/pdf/10.2214/AJR.09.3674
Level of evidence 2B, grades of recommendation B</ref> | ||
[[Image:Hamstring origin tendinopathy.jpg|right]] | |||
== Clinically Relevant Anatomy == | |||
-One of the most important muscle groups in running is the hamstring. They are active at various stages in the gait cycle, particularly in knee flexion and hip extension. | |||
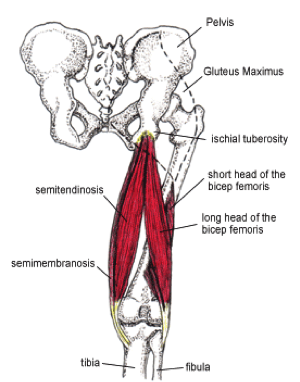
[[ | -Consisting of three fibers all originating from the ischial tuberosity and femur. | ||
-Distally the muscle is inserted on the back of the knee, both on tibia and fibula. | |||
-The junction between the tendons of the hamstrings and the ischial tuberosity is the area affected by high hamstring tendinopathy. The tendon’s thickness, fibrousness and poor blood supply are the cases of difficult healing.<ref name="p0">High hamstring tendinopathy injuries – Signs, symptoms and research-backed treatment solutions for a literal pain in the butt.
Available from:
http://runnersconnect.net/running-injury-prevention/high-hamstring-tendinopathy-injuries-a-pain-in-the-butt/</ref> | |||
[[File:Hamstring_tendons.png|right]] | |||
<br>-The muscles contain a higher proportion of type 2 muscle fibers than the other muscles of the lower extremity; suggesting high intrinsic force generation. | |||
-During running, the hamstrings have three main functions. First, they decelerate knee extension at the end of the forward swing phase of the gait cycle. Through an eccentric contraction, the hamstrings decelerate the forward momentum (ie, leg swing) at approximately 30° short of full knee extension. This action helps provide dynamic stabilization to the weight bearing knee. Second, at foot strike, the hamstrings elongate to facilitate hip extension through an eccentric contraction, thus further stabilizing the leg for weight bearing. Third, the hamstrings assist the gastrocnemius in paradoxically extending the knee during the takeoff phase of the running cycle.<ref name="p4">Michael Fredericson, et al. High Hamstring Tendinopathy in Runners. Meeting the Challenges of Diagnosis, Treatment, and Rehabilitation [Internet]. The Physician and Sportsmedicine 2005. Available from: http://www.agilept.com/downloads/high-hamstring-tendinopathy-in-runners.pdf - Level of evidence 2A, grades of recommendation B</ref> | |||
(For extra information about pathology mechanisms see [http://www.physio-pedia.com/Tendinopathy Tendinopathy])<br> | (For extra information about pathology mechanisms see [http://www.physio-pedia.com/Tendinopathy Tendinopathy])<br> | ||
= Epidemiology / Etiology = | == Epidemiology / Etiology == | ||
* Acute tear at the origin that is not properly treated. | |||
* Overuse Injury: the most common case, and often seen in middle- or long distance runners than sprinters<ref name="p4" />, repetitive jumping and kicking activities. | |||
* The hamstrings are prone to this type of injury as they contribute to the deceleration of knee extension during activities such as sprinting and hill climbing. (Petersen J. et al, 2005). | |||
== Risk Factors: == | |||
<br>'''''Intrinsic factors:''''' | |||
*Malalignments | *Malalignments | ||
*Leg length discrepancy | *Leg length discrepancy | ||
*Imbalance | *Imbalance | ||
*Decreased flexibility | *Decreased flexibility | ||
*Joint laxity | |||
*Joint laxity | |||
*Female gender | *Female gender | ||
*Age - | *Age - Reduction in muscle fiber size and number are associated with advancing in age, this leads to losses of mass and strength.<ref name="p6">P.BRUKNER & K. KAHN, clinical sports medicine, McGraw-Hill, Australia, 2005 (third edition), P388-390</ref> | ||
*Overweight | *Overweight | ||
*Proprioceptive | *Proprioceptive deficiency<ref name="kristen">White, K. E., High hamstring tendinopathy in 3 female long distance runners. Journal of Chiropractic Medicine 2011, 10 (2), 93-99
Level of evidence 4. grades of recommendation C</ref> | ||
*Ischial tuberosity tenderness | *Ischial tuberosity tenderness | ||
*Core weakness | *Core weakness<ref name="fred" /> | ||
*Pelvic dysfunction<ref name="fred">Fredericson, M.; Moore, W.; Guillet, M.; Beaulieu, C., High hamstring tendinopathy in runners: Meeting the challanges of diagnosis, treatment, and rehabilitation. Physician and Sportsmedicine 2005, 33 (5), 32-43.
Level of evidence 4, grades of recommendation C</ref> | *Pelvic dysfunction<ref name="fred">Fredericson, M.; Moore, W.; Guillet, M.; Beaulieu, C., High hamstring tendinopathy in runners: Meeting the challanges of diagnosis, treatment, and rehabilitation. Physician and Sportsmedicine 2005, 33 (5), 32-43.
Level of evidence 4, grades of recommendation C</ref> | ||
*Previous injury - the strength is reduced by previous hamstrings, knee or groin injuries.<ref name="p6" /> | *Previous injury - the strength is reduced by previous hamstrings, knee or groin injuries.<ref name="p6" /> | ||
*Neuromyofascial involvement- | *Neuromyofascial involvement- increased neural tension and posterior thigh pain due to myofascial trigger points; often associated with decreased flexibility.<ref name="p6" /> | ||
* | *Hip stiffness | ||
*Tightness/Weakness of the hamstrings and quadriceps | *Tightness/Weakness of the hamstrings and quadriceps | ||
* | *poor pelvic/core stability.<ref name="p9">Tele Demetrious and Brett Harrop. Hamstring Origin Tendonitis. PhysioAdvisor 2008. [http://www.physioadvisor.com.au/9628550/hamstring-origin-tendonitis-hamstring-injury-p.htm http://www.physioadvisor.com.au/9628550/hamstring-origin-tendonitis-hamstring-injury-p.htm
Level] of evidence 5, grades of recommendation D</ref> | ||
<br>'''Extrinsic factors:''' | <br>'''Extrinsic factors:''' | ||
* | *Excessive, repetitive overloads and over training. | ||
*training | *Poor training | ||
* | *Environmental conditions | ||
* | *Poor equipment | ||
*Insufficient | *Insufficient warm up - A warm-up with isometric contractions increases strength and length of the muscle.<ref name="p6" /> A study found an association between hamstrings injuries and lack of stretch prior to sports participation.<ref name="p6" /> | ||
*Fatigue - causes decline in muscle energy, decreased concentration and coordination and poor technique.<ref name="p6" /> | |||
<br> | <br>-Intrinsic and Extrinsic factors contribute to the formation of injury.<ref name="p0" /> | ||
< | |||
The | -The tendinopathy usually starts with micro-damage without a remarkable trauma. Normally the tendon is capable to intrinsic repair, meaning that the consequences of this injury are little. Sometimes, imbalance can cause further damage and failed healing. All of this leads to the formation of tendinosis. (Kannus 1997, Sharma and Maffulli 2005, Warden 2007).<br> | ||
Continued exercises and stretching can cause even more pain<ref name="p4"/>.<br>Pain down the back of the thigh can be caused by irritation of the sciatic nerve. This nerve passes very close to the ischial tuberosity.<ref name="p0" /> Due to its degenerative nature, this injury is classified as a tendinopathy rather than a tendonitis, an inflammatory pathology.<ref name="p5"/> | == Clinical Picture == | ||
* Deep buttock pain and pain in the posterior thigh. | |||
* The pain is often felt on the lower gluteal region, radiating along the hamstings<ref name="fred" />. | |||
[[Image:Hamstring-tendonitis-pain-pattern.jpg|right]] | |||
* The pain increases with repetitive activities (such as long-distance running). And in some cases pain flares with seating or driving. | |||
* The onset is mostly gradual, not with acute trauma.<ref name="p3">Puranen J.; Orava S., The hamstring syndrome. A new diagnosis of gluteal sciatic pain, American Journal of Sports Medicine, 1988, 16(5): 517 – 521.
Level of evidence 4, grades of recommendation C</ref>. | |||
* Continued exercises and stretching can cause even more pain<ref name="p4" />.<br>Pain down the back of the thigh can be caused by irritation of the sciatic nerve. This nerve passes very close to the ischial tuberosity.<ref name="p0" /> Due to its degenerative nature, this injury is classified as a tendinopathy rather than a tendonitis, an inflammatory pathology.<ref name="p5" /> | |||
= Differential Diagnosis = | == Differential Diagnosis == | ||
* First of all, it’s essential to determine if the pain is local or referred. referred pain is characterized by complains of pain in varies locations. Pain in the buttock combined with pain in the lower back may refer to the lumbar spine. This may be caused by muscles, ligaments or disks dysfunctions. | |||
* Localized constant pain in the buttock, around ischial tuberosity could be triggered by hamstring origin tendinopathy or ischiogluteal bursitis. | |||
* If the patient complains of higher pain (upper gluteal region) there might be a problem with the piriformis muscle. | |||
* Pain over the sacrum or near the sacroiliac joint refers to a pelvic stress fracture or inflammation or malalignment of the sacroiliac joint. | |||
* There are also some uncommon cases where buttock and posterior thigh pain refer to chronic compartment syndrome of the posterior thigh. Due to the resemblance of some symptoms of this injury with other hip injuries, it’s important to get a proper diagnosis; this will likely entail a physical examination and an MRI.<ref name="p4" /><br> | |||
== Diagnostic Procedures == | |||
-MRI is required to confirm the diagnosis and to take a look at the severity of the injury. <br>-MRI can detect tendon thickening, tearing, inflammation and swelling at the ischial tuberosity. | |||
-Ultrasound is also used, but this technique isn’t able to give a precise visualization of bone marrow edema.<ref name="p2">McCormack R. J., The management of bilateral high hamstring tendinopathy with ASTYM treatment and eccentric exercise: a case report, The Journal of Manual and Manipulative Therapy, 2012, 20(3) 142 – 146.
Level of evidence 4, grades of recommendation C</ref> <br>-Normally a high hamstring injury may be combined with stress reaction or bone edema in the ischial tuberosity and findings of the tendon. In case of a tendinopathy an increased signal is noticeable on T1-weighted images with no abnormalities on fat-suppressed T2-weighted images.<ref name="p4" /><ref name="p5" /> | |||
-A series of provocation tests have been developed in order to help for the diagnose of this injury.<br> | |||
Pain provocation tests: | '''''Pain provocation tests:''''' | ||
'''<br>1) Palpation of the tuber ishiadicum''' | '''<br>1) Palpation of the tuber ishiadicum''' | ||
| Line 137: | Line 104: | ||
<br> | <br> | ||
<br> | <br>'''2) The Puranen-Orava test''' | ||
'''2) The Puranen-Orava test''' | |||
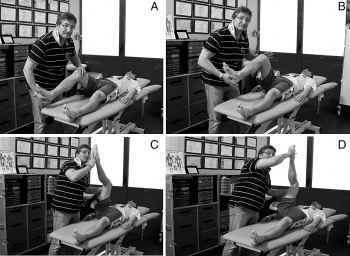
[[Image:PO test.jpg|300x200px|right]]This test is a standing stretch of the hamstrings, there must be a hip flexion of 90°. The foot rests on a support and the knee is in extension. | |||
This test is a standing stretch of the hamstrings, there must be a hip flexion of 90°. The foot rests on a support and the knee is in extension. | |||
<br>'''3) Bent-knee stretch test:''' | <br>'''3) Bent-knee stretch test:''' | ||
The test is performed while the patient is lying on his back. The hip and knee are maximally flexed. Slowly the therapist will straighten the knee till its | The test is performed while the patient is lying on his back. The hip and knee are maximally flexed. Slowly the therapist will straighten the knee till its maximally extended; the hip must remain in a 90° flexion. The test is also doable without the assistance of a therapist. The patient can use a rope or a belt to straighten his knee like depicted on the picture. | ||
{{#ev:youtube|Xg0ghED6AS8}}<ref>Physiotutors. Bent Knee Stretch Test ⎟ Proximal Hamstring Tightness and Tendinopathy. Available from: https://www.youtube.com/watch?v=Xg0ghED6AS8 </ref> | {{#ev:youtube|Xg0ghED6AS8}}<ref>Physiotutors. Bent Knee Stretch Test ⎟ Proximal Hamstring Tightness and Tendinopathy. Available from: https://www.youtube.com/watch?v=Xg0ghED6AS8 </ref> | ||
<br> | <br><br>'''4) Modified bent-knee stretch test''' | ||
<br>'''4) Modified bent-knee stretch test''' | |||
= | [[Image:Modified bent knee.jpg|350x300px|right]]The test is performed while the patient is lying on his back, the hip and knee are in extension. The therapist takes the heel in one hand and holds the knee with the other hand. He brings the hip and knee in maximal flexion and then rapidly straightens the knee.<br>These tests are used to identify a hamstrings origin tendinopathy, but do not replace an MRI.<ref name="p0" /> | ||
== Prevention == | |||
Good flexibility of the hamstring and quadriceps muscles must be maintained for the prevention of this injury.<br>Some preventive techniques related to sport techniques are to avoid block drills in the beginning of the season or on two following days.<ref name="p2" /> <br><br> | |||
= <br> | == Medical Management == | ||
-Anti-inflammatory drugs..<ref name="p0" /> <br>-In more severe cases, when physical therapy does not help, a corticosteroid injection into the peritendinous soft tissues is recommended in combination with physical therapy. Injecting the substance in the tendon itself can be dangerous. Frederickson et al. found that patients whose MRIs showed more swelling around the tuberositas ischiadicum and less thickening of the tendon got more relief from a cortisone injection than patients with more pronounced tendon thickening. However, corticosteroid injections can also have a negative impact on the tendons inter alia the weakening of tendons, the rupture of tendons, particularly in load-bearing tendons (Kleinman M. et al, 1983) | |||
-A novel treatment is platelet-rich plasma injection at the origin of the muscle.<ref name="p0" /> Platelet-rich plasma (PRP) seems to be a promising alternative to the corticosteroid injections. The alpha and dense granulates that are present in the platelets, release multiple growth factors and cytokines that promote wound healing (Alsousou J. et al, 2009 & Mishra A. et al, 2009). An enhancement of the recruitment, proliferation and differentiation of the cells involved in soft-tissue regeneration has been reported by the authors of in vitro studies (Hall MP et al, 2009, De Mos M. et al, 2008) | |||
The shockwave therapy has almost no influence on hamstrings origin tendinopathies.<ref name="p5" /> <br>When | -The shockwave therapy has almost no influence on hamstrings origin tendinopathies.<ref name="p5" /> <br>-When conservative treatment fails, patient may need surgery to decrease the pressure on the nerve and to divide the fibrous and damaged tendon.<ref name="p6" /><br> <br> | ||
= Physical Therapy Management = | == Physical Therapy Management == | ||
* The earlier the patients starts physical therapy, the faster he/she will return to previous normal function. | |||
* Therapy takes from weeks to months depending on the condition and the history of previous injuries.<ref name="p9" /> | |||
* Controlling the pain is one of the important therapy goals, this is possible through ice, electrical stimulation of the tendon and pulsed ultrasound. | |||
* Correction of pelvis misalignment has to be taken into consideration, as it might increase the tension on the hamstring muscles,and affects muscle strength. Anterior pelvic tilt is the most common misalignment and it could be easily corrected by manual or chiropractic manipulation. | |||
* Soft-tissue mobilization has to be included in the rehabilitation program. It’s very beneficial to break up the adhesions and scar tissues. A friction treatment with transverse frictions is commonly used. The therapist has to pay attention to not compress directly on the ischial tuberosity as it can irritate underlying edema. Techniques like ART (Active Release Technique) or Gastron can be included as well. | |||
* At the same time the patient may start a gradual stretching program for the hamstrings. starting with double-leg non weight bearing isometric exercises followed by single-leg closed-chain isometric and isotonic open-chain exercises. | |||
* Eccentric muscle strengthening program is a good treatment program for teninopathies , as it can normalize the thickness and structure of the tendon. It can also prepare the hamstrings for the high-force load while running. | |||
* Glute bridges are interesting exercises to start a strength rehabilitation program with. Afterwards the patient can start with introductory exercises such as a standing ‘hamstring catch’. By using a Swiss Ball we can increase the difficulty of the exercise. As Frederickson et al stated, Swiss ball curl is ideal for development of both eccentric and concentric strength. According to the tolerance and the progression of the patient these Swiss ball curls can be practiced with short range of motion to full range of motion and eventually, single-legged Swiss ball curls. | |||
* Core strength is a considerable element for the rehabilitation of hamstring origin tendinopathy as it reduces the risk of recurrent hamstring strains.. Plank exercises, especially with leg lifts incorporated are recommended by Frederickson who has conducted numerous studies about the rehabilitation of the hamstrings. Exercises like these encourage co-activation of the glute and hamstring muscles. | |||
* If the ROM of the muscle is normal and pain-free, pool running and stationary biking could be put into the rehabilitation program.<ref name="p1">Reid, D.C., 1992. Sports injury assessment and rehabilitation. USA: Churchill Livingstone Inc. Pp. 415, 417, 554-570.
Level of evidence 2A, grades of recommendation B</ref><ref name="p3" /><ref name="p4" /><ref name="p6" /><ref name="p7">Daniel Lorenz and Michael Reiman. The Role and Implementation of Eccentric Training in Athletic Rehabilitation: Tendinopathy, Hamstring Strains, and ACL Reconstruction [Internet]. Sports Physical Therapy Section 2011. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3105370/?tool=pubmed
Level of evidence 2A, grades of recommendation B</ref><ref name="p8">Mike Walden. Hamstring Origin Tendinitis / Tendinopathy. Sportsinjuryclinic.net 2011
[http://www.sportsinjuryclinic.net/cybertherapist/back/buttocks/hamstring_tendinitis.htm http://www.sportsinjuryclinic.net/cybertherapist/back/buttocks/hamstring_tendinitis.htm
Level] of evidence 5, grades of recommendation D</ref> | |||
* Stretching of both legs is crucial for balance. Even the antagonist hip flexor muscles should be stretched for an optimal function. | |||
* ROM can be increased by the use of ultrasound or shockwave therapy before stretching. Frequent stretching may avoid a recurrence of the injury. | |||
'''''Running again:''''' | |||
* High hamstring tendinopathy is known as a disease that takes a long time to recover from. Fredericson et al. estimates a recovery of 8-12 weeks. It’s likely that cross training doesn’t stress the legs until the bent-knee stretch test can be done without pain. | |||
* When exercises becomes pain free, the following return-to-running program could be initiated:<br><br>Week 1: Walk 5min/jog 1min, build to sets on alternating days (ex. 2x5min/1min, off, 3x5min/1min, off, ect)<br>Week 2: If no pain, walk 5min/jog 5min, build to 5 sets on alternating days<br>Week 3: If no pain, advance to 20min jog, no more than 5 days per week<br>Week 4: If no pain, advance to 20min run at normal training pace, no more than 5 days per week<br>Week 5-8: If no pain, gradually increase running speed, volume, and acceleration as tolareted<ref name="p0" /> <br> | |||
== | == Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
<div class="researchbox">
<rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=14spTIXMx9q9VwGc_iFE1h7hwFbE0SyCjyPXH6byN8</rss>
<br> </div> | <div class="researchbox">
<rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=14spTIXMx9q9VwGc_iFE1h7hwFbE0SyCjyPXH6byN8</rss>
<br> </div> | ||
= References = | == References == | ||
<references /><br> | <references /><br> | ||
[[Category:Conditions]] [[Category:Knee]] [[Category:Hip]] [[Category:Knee_Conditions]] [[Category:Sports_Injuries]] [[Category:Musculoskeletal/Orthopaedics]] | [[Category:Conditions]] [[Category:Knee]] [[Category:Hip]] [[Category:Knee_Conditions]] [[Category:Sports_Injuries]] [[Category:Musculoskeletal/Orthopaedics]] | ||
Revision as of 17:17, 17 August 2017
Original Editor - Melissa De Maeyer
Top Contributors - Wanda van Niekerk, Kim Jackson, Vidya Acharya, Mandeepa Kumawat, Mariam Hashem, Lisa De Donder, Melissa De Maeyer, Vanessa Rhule, Admin, Lotte De Clerck, WikiSysop, 127.0.0.1, Oyemi Sillo, Kai A. Sigel, HaniaElGibaly, Rachael Lowe, Aidan Rich, Evan Thomas, Naomi O'Reilly and George Prudden
Description[edit | edit source]
-Hamstring origin tendinopathy, also called proximal hamstring tendinopathy or high hamstring tendinopathy, are a group of pathologies of the proximal hamstring tendon.
They include tendon degeneration, partial tearing and peritendinous inflammatory reaction.[1]
Clinically Relevant Anatomy[edit | edit source]
-One of the most important muscle groups in running is the hamstring. They are active at various stages in the gait cycle, particularly in knee flexion and hip extension.
-Consisting of three fibers all originating from the ischial tuberosity and femur.
-Distally the muscle is inserted on the back of the knee, both on tibia and fibula.
-The junction between the tendons of the hamstrings and the ischial tuberosity is the area affected by high hamstring tendinopathy. The tendon’s thickness, fibrousness and poor blood supply are the cases of difficult healing.[2]
-The muscles contain a higher proportion of type 2 muscle fibers than the other muscles of the lower extremity; suggesting high intrinsic force generation.
-During running, the hamstrings have three main functions. First, they decelerate knee extension at the end of the forward swing phase of the gait cycle. Through an eccentric contraction, the hamstrings decelerate the forward momentum (ie, leg swing) at approximately 30° short of full knee extension. This action helps provide dynamic stabilization to the weight bearing knee. Second, at foot strike, the hamstrings elongate to facilitate hip extension through an eccentric contraction, thus further stabilizing the leg for weight bearing. Third, the hamstrings assist the gastrocnemius in paradoxically extending the knee during the takeoff phase of the running cycle.[3]
(For extra information about pathology mechanisms see Tendinopathy)
Epidemiology / Etiology[edit | edit source]
- Acute tear at the origin that is not properly treated.
- Overuse Injury: the most common case, and often seen in middle- or long distance runners than sprinters[3], repetitive jumping and kicking activities.
- The hamstrings are prone to this type of injury as they contribute to the deceleration of knee extension during activities such as sprinting and hill climbing. (Petersen J. et al, 2005).
Risk Factors:[edit | edit source]
Intrinsic factors:
- Malalignments
- Leg length discrepancy
- Imbalance
- Decreased flexibility
- Joint laxity
- Female gender
- Age - Reduction in muscle fiber size and number are associated with advancing in age, this leads to losses of mass and strength.[4]
- Overweight
- Proprioceptive deficiency[5]
- Ischial tuberosity tenderness
- Core weakness[6]
- Pelvic dysfunction[6]
- Previous injury - the strength is reduced by previous hamstrings, knee or groin injuries.[4]
- Neuromyofascial involvement- increased neural tension and posterior thigh pain due to myofascial trigger points; often associated with decreased flexibility.[4]
- Hip stiffness
- Tightness/Weakness of the hamstrings and quadriceps
- poor pelvic/core stability.[7]
Extrinsic factors:
- Excessive, repetitive overloads and over training.
- Poor training
- Environmental conditions
- Poor equipment
- Insufficient warm up - A warm-up with isometric contractions increases strength and length of the muscle.[4] A study found an association between hamstrings injuries and lack of stretch prior to sports participation.[4]
- Fatigue - causes decline in muscle energy, decreased concentration and coordination and poor technique.[4]
-Intrinsic and Extrinsic factors contribute to the formation of injury.[2]
-The tendinopathy usually starts with micro-damage without a remarkable trauma. Normally the tendon is capable to intrinsic repair, meaning that the consequences of this injury are little. Sometimes, imbalance can cause further damage and failed healing. All of this leads to the formation of tendinosis. (Kannus 1997, Sharma and Maffulli 2005, Warden 2007).
Clinical Picture[edit | edit source]
- Deep buttock pain and pain in the posterior thigh.
- The pain is often felt on the lower gluteal region, radiating along the hamstings[6].
- The pain increases with repetitive activities (such as long-distance running). And in some cases pain flares with seating or driving.
- The onset is mostly gradual, not with acute trauma.[8].
- Continued exercises and stretching can cause even more pain[3].
Pain down the back of the thigh can be caused by irritation of the sciatic nerve. This nerve passes very close to the ischial tuberosity.[2] Due to its degenerative nature, this injury is classified as a tendinopathy rather than a tendonitis, an inflammatory pathology.[1]
Differential Diagnosis[edit | edit source]
- First of all, it’s essential to determine if the pain is local or referred. referred pain is characterized by complains of pain in varies locations. Pain in the buttock combined with pain in the lower back may refer to the lumbar spine. This may be caused by muscles, ligaments or disks dysfunctions.
- Localized constant pain in the buttock, around ischial tuberosity could be triggered by hamstring origin tendinopathy or ischiogluteal bursitis.
- If the patient complains of higher pain (upper gluteal region) there might be a problem with the piriformis muscle.
- Pain over the sacrum or near the sacroiliac joint refers to a pelvic stress fracture or inflammation or malalignment of the sacroiliac joint.
- There are also some uncommon cases where buttock and posterior thigh pain refer to chronic compartment syndrome of the posterior thigh. Due to the resemblance of some symptoms of this injury with other hip injuries, it’s important to get a proper diagnosis; this will likely entail a physical examination and an MRI.[3]
Diagnostic Procedures[edit | edit source]
-MRI is required to confirm the diagnosis and to take a look at the severity of the injury.
-MRI can detect tendon thickening, tearing, inflammation and swelling at the ischial tuberosity.
-Ultrasound is also used, but this technique isn’t able to give a precise visualization of bone marrow edema.[9]
-Normally a high hamstring injury may be combined with stress reaction or bone edema in the ischial tuberosity and findings of the tendon. In case of a tendinopathy an increased signal is noticeable on T1-weighted images with no abnormalities on fat-suppressed T2-weighted images.[3][1]
-A series of provocation tests have been developed in order to help for the diagnose of this injury.
Pain provocation tests:
1) Palpation of the tuber ishiadicum
2) The Puranen-Orava test
This test is a standing stretch of the hamstrings, there must be a hip flexion of 90°. The foot rests on a support and the knee is in extension.
3) Bent-knee stretch test:
The test is performed while the patient is lying on his back. The hip and knee are maximally flexed. Slowly the therapist will straighten the knee till its maximally extended; the hip must remain in a 90° flexion. The test is also doable without the assistance of a therapist. The patient can use a rope or a belt to straighten his knee like depicted on the picture.
4) Modified bent-knee stretch test
The test is performed while the patient is lying on his back, the hip and knee are in extension. The therapist takes the heel in one hand and holds the knee with the other hand. He brings the hip and knee in maximal flexion and then rapidly straightens the knee.
These tests are used to identify a hamstrings origin tendinopathy, but do not replace an MRI.[2]
Prevention[edit | edit source]
Good flexibility of the hamstring and quadriceps muscles must be maintained for the prevention of this injury.
Some preventive techniques related to sport techniques are to avoid block drills in the beginning of the season or on two following days.[9]
Medical Management[edit | edit source]
-Anti-inflammatory drugs..[2]
-In more severe cases, when physical therapy does not help, a corticosteroid injection into the peritendinous soft tissues is recommended in combination with physical therapy. Injecting the substance in the tendon itself can be dangerous. Frederickson et al. found that patients whose MRIs showed more swelling around the tuberositas ischiadicum and less thickening of the tendon got more relief from a cortisone injection than patients with more pronounced tendon thickening. However, corticosteroid injections can also have a negative impact on the tendons inter alia the weakening of tendons, the rupture of tendons, particularly in load-bearing tendons (Kleinman M. et al, 1983)
-A novel treatment is platelet-rich plasma injection at the origin of the muscle.[2] Platelet-rich plasma (PRP) seems to be a promising alternative to the corticosteroid injections. The alpha and dense granulates that are present in the platelets, release multiple growth factors and cytokines that promote wound healing (Alsousou J. et al, 2009 & Mishra A. et al, 2009). An enhancement of the recruitment, proliferation and differentiation of the cells involved in soft-tissue regeneration has been reported by the authors of in vitro studies (Hall MP et al, 2009, De Mos M. et al, 2008)
-The shockwave therapy has almost no influence on hamstrings origin tendinopathies.[1]
-When conservative treatment fails, patient may need surgery to decrease the pressure on the nerve and to divide the fibrous and damaged tendon.[4]
Physical Therapy Management[edit | edit source]
- The earlier the patients starts physical therapy, the faster he/she will return to previous normal function.
- Therapy takes from weeks to months depending on the condition and the history of previous injuries.[7]
- Controlling the pain is one of the important therapy goals, this is possible through ice, electrical stimulation of the tendon and pulsed ultrasound.
- Correction of pelvis misalignment has to be taken into consideration, as it might increase the tension on the hamstring muscles,and affects muscle strength. Anterior pelvic tilt is the most common misalignment and it could be easily corrected by manual or chiropractic manipulation.
- Soft-tissue mobilization has to be included in the rehabilitation program. It’s very beneficial to break up the adhesions and scar tissues. A friction treatment with transverse frictions is commonly used. The therapist has to pay attention to not compress directly on the ischial tuberosity as it can irritate underlying edema. Techniques like ART (Active Release Technique) or Gastron can be included as well.
- At the same time the patient may start a gradual stretching program for the hamstrings. starting with double-leg non weight bearing isometric exercises followed by single-leg closed-chain isometric and isotonic open-chain exercises.
- Eccentric muscle strengthening program is a good treatment program for teninopathies , as it can normalize the thickness and structure of the tendon. It can also prepare the hamstrings for the high-force load while running.
- Glute bridges are interesting exercises to start a strength rehabilitation program with. Afterwards the patient can start with introductory exercises such as a standing ‘hamstring catch’. By using a Swiss Ball we can increase the difficulty of the exercise. As Frederickson et al stated, Swiss ball curl is ideal for development of both eccentric and concentric strength. According to the tolerance and the progression of the patient these Swiss ball curls can be practiced with short range of motion to full range of motion and eventually, single-legged Swiss ball curls.
- Core strength is a considerable element for the rehabilitation of hamstring origin tendinopathy as it reduces the risk of recurrent hamstring strains.. Plank exercises, especially with leg lifts incorporated are recommended by Frederickson who has conducted numerous studies about the rehabilitation of the hamstrings. Exercises like these encourage co-activation of the glute and hamstring muscles.
- If the ROM of the muscle is normal and pain-free, pool running and stationary biking could be put into the rehabilitation program.[11][8][3][4][12][13]
- Stretching of both legs is crucial for balance. Even the antagonist hip flexor muscles should be stretched for an optimal function.
- ROM can be increased by the use of ultrasound or shockwave therapy before stretching. Frequent stretching may avoid a recurrence of the injury.
Running again:
- High hamstring tendinopathy is known as a disease that takes a long time to recover from. Fredericson et al. estimates a recovery of 8-12 weeks. It’s likely that cross training doesn’t stress the legs until the bent-knee stretch test can be done without pain.
- When exercises becomes pain free, the following return-to-running program could be initiated:
Week 1: Walk 5min/jog 1min, build to sets on alternating days (ex. 2x5min/1min, off, 3x5min/1min, off, ect)
Week 2: If no pain, walk 5min/jog 5min, build to 5 sets on alternating days
Week 3: If no pain, advance to 20min jog, no more than 5 days per week
Week 4: If no pain, advance to 20min run at normal training pace, no more than 5 days per week
Week 5-8: If no pain, gradually increase running speed, volume, and acceleration as tolareted[2]
Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Maurice H. Zissen, et al. High Hamstring Tendinopathy: MRI and Ultrasound Imaging and Therapeutic Efficacy of Percutaneous Coorticosteroid Injection [Internet]. American Roentgen Ray Society 2010.Available from: http://www.ajronline.org/doi/pdf/10.2214/AJR.09.3674 Level of evidence 2B, grades of recommendation B
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 High hamstring tendinopathy injuries – Signs, symptoms and research-backed treatment solutions for a literal pain in the butt. Available from: http://runnersconnect.net/running-injury-prevention/high-hamstring-tendinopathy-injuries-a-pain-in-the-butt/
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Michael Fredericson, et al. High Hamstring Tendinopathy in Runners. Meeting the Challenges of Diagnosis, Treatment, and Rehabilitation [Internet]. The Physician and Sportsmedicine 2005. Available from: http://www.agilept.com/downloads/high-hamstring-tendinopathy-in-runners.pdf - Level of evidence 2A, grades of recommendation B
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 P.BRUKNER & K. KAHN, clinical sports medicine, McGraw-Hill, Australia, 2005 (third edition), P388-390
- ↑ White, K. E., High hamstring tendinopathy in 3 female long distance runners. Journal of Chiropractic Medicine 2011, 10 (2), 93-99 Level of evidence 4. grades of recommendation C
- ↑ 6.0 6.1 6.2 Fredericson, M.; Moore, W.; Guillet, M.; Beaulieu, C., High hamstring tendinopathy in runners: Meeting the challanges of diagnosis, treatment, and rehabilitation. Physician and Sportsmedicine 2005, 33 (5), 32-43. Level of evidence 4, grades of recommendation C
- ↑ 7.0 7.1 Tele Demetrious and Brett Harrop. Hamstring Origin Tendonitis. PhysioAdvisor 2008. http://www.physioadvisor.com.au/9628550/hamstring-origin-tendonitis-hamstring-injury-p.htm Level of evidence 5, grades of recommendation D
- ↑ 8.0 8.1 Puranen J.; Orava S., The hamstring syndrome. A new diagnosis of gluteal sciatic pain, American Journal of Sports Medicine, 1988, 16(5): 517 – 521. Level of evidence 4, grades of recommendation C
- ↑ 9.0 9.1 McCormack R. J., The management of bilateral high hamstring tendinopathy with ASTYM treatment and eccentric exercise: a case report, The Journal of Manual and Manipulative Therapy, 2012, 20(3) 142 – 146. Level of evidence 4, grades of recommendation C
- ↑ Physiotutors. Bent Knee Stretch Test ⎟ Proximal Hamstring Tightness and Tendinopathy. Available from: https://www.youtube.com/watch?v=Xg0ghED6AS8
- ↑ Reid, D.C., 1992. Sports injury assessment and rehabilitation. USA: Churchill Livingstone Inc. Pp. 415, 417, 554-570. Level of evidence 2A, grades of recommendation B
- ↑ Daniel Lorenz and Michael Reiman. The Role and Implementation of Eccentric Training in Athletic Rehabilitation: Tendinopathy, Hamstring Strains, and ACL Reconstruction [Internet]. Sports Physical Therapy Section 2011. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3105370/?tool=pubmed Level of evidence 2A, grades of recommendation B
- ↑ Mike Walden. Hamstring Origin Tendinitis / Tendinopathy. Sportsinjuryclinic.net 2011 http://www.sportsinjuryclinic.net/cybertherapist/back/buttocks/hamstring_tendinitis.htm Level of evidence 5, grades of recommendation D