Pancreatic Cancer: Difference between revisions
m (Text replace - ''''Lead Editors'''' to ''''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}') |
(Added external link to reference and corrected the reference.) |
||
| (10 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors '''- Jaimin Shah | '''Original Editors '''- Jaimin Shah [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
== Definition/Description == | == Definition/Description == | ||
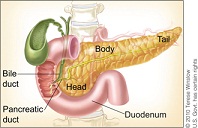
[[Image:Blah.jpg|Anatomical Position of Pancreas|alt=|right|frameless]]Pancreatic Cancer is a malignant disease of the pancreas. “Pancreatic adenocarcinoma is a highly lethal disease, which is usually diagnosed in an advanced state.”<ref name="Li et al">Li C, Heidt DG, Dalerba P, Burant CF, Zhang L, Adsay V, Wicha M, Clarke MF, Simeone DM. [https://aacrjournals.org/cancerres/article/67/3/1030/533872/Identification-of-Pancreatic-Cancer-Stem-Cells Identification of pancreatic stem cells]. Cancer research. 2007 Feb 1;67(3): 1030-1037</ref> The malignant tumor can be located near the head, body, or the tail of the pancreas. The pancreas is an organ that helps secrete insulin and glucagon which helps control blood glucose levels in the body. Pancreatic cancer is the fourth common cancer among men and the fifth leading cause of cancer in women. There are two types of pancreatic cancers which are exocrine cancer and endocrine cancer. “Pancreatic ductal adenocarcinoma (PDAC) compromises 90% of pancreatic cancers.”<ref name="Shore et al">Shore S, Vimalachadran D, Raraty MGT, Ghaneh P. Cancer in the elderly: pancreatic cancer. Surgical Onocology 2004;13:201-210</ref> Exocrine pancreatic cancers are the most common of pancreatic cancers. Exocrine pancreatic cancer is involved in the ducts of the pancreas that secrete juices. [[Image:Blah3.jpg|alt=|right|frameless]]Key Points | |||
* The pancreas is a gland that secretes digestive enzymes and insulin. | |||
* The symptoms of pancreatic cancer are often vague and common to many other disorders. | |||
* Pancreatic cancer is often only diagnosed in its later stages, which makes it difficult to treat.<ref name=":0">Better Health Pancreratic Cancer Available:https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pancreatic-cancer#diagnosis-of-pancreatic-cancer (accessed 3.9.2021)</ref> | |||
== Epidemiology == | |||
<br> | * Pancreatic cancer accounts for 22% of all deaths due to gastrointestinal malignancy, and 5% of all cancer deaths. In general, it is a malignancy of the [[Older People Introduction|elderly]] with over 80% of cases occurring after the age of 60.<ref name=":1">Radiopedia pancreatic Cancer Available: https://radiopaedia.org/articles/pancreatic-ductal-adenocarcinoma-2 (accessed 3.9.2021)</ref> | ||
* Pancreatic cancer is the fourth most common cause of cancer death for men and women in US.<ref name="Farma et al">Farma JM, Santillan AA, Melis M, Walters J, Belinc D, Chen D, Eikman EA, Malafa M. PET/CT fusion scan enhances CT staging in patients with pancreatic neoplasms. Annals of Surgical Oncology 2008;15(9):2465-2471</ref> | |||
* Pancreatic cancer is more common in black men and women than whites. <br>Pancreatic cancer is rare in people under the age of 45, the risk increases after age of 50. | |||
== Etiology == | |||
[[Image:Smoke-that-cigarette.jpg|frame|cigarette-- risk factor|alt=]]Risk factors include: | |||
* cigarette smoking: the strongest environmental risk factor | |||
* a diet rich in animal fats and protein | |||
< | * obesity | ||
* family history: three or more first-order relatives with pancreatic cancer results in ~20x risk | |||
* hereditary syndromes<ref name=":1" /> | |||
* Possible risk factors include heavy alcohol consumption, coffee consumption, physical inactivity, high red meat consumption, and two or more soft drinks per day. | |||
* Ten percent have a genetic cause such as genetic mutations or association with syndromes eg multiple endocrine neoplasia type 1<ref name=":2">Puckett Y, Garfield K. [https://www.ncbi.nlm.nih.gov/books/NBK518996/ Pancreatic Cancer]. InStatPearls [Internet] 2021 Aug 11. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK518996/ (accessed 3.9.2021)</ref>. | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Most clinical presentations of pancreatic cancers are vague and delay the potential diagnosis. “Pancreatic cancer is relatively asymptomatic during its early course. The vague presentation includes back and epigastric pain.”<ref name="Shore et al" /> Symptoms associated with pancreatic cancer include:[[Image:Abdominal pain.jpg|alt=|right|frameless]] | |||
Most clinical presentations of pancreatic cancers are vague and delay the potential diagnosis. “Pancreatic cancer is relatively asymptomatic during its early course. The vague presentation includes back and epigastric pain.”<ref name="Shore et al" /> | *Pain is the presenting symptom in between 31% and 71% of pancreatic cancer patients | ||
*Jaundice | |||
Pain | *Digestive Problems | ||
*Blood Clots | |||
Jaundice | *Weight Loss | ||
*Abdominal or Back Pain | |||
Digestive Problems | *Gallbladder Enlargement | ||
*Dark Urine | |||
Blood Clots | *Nausea and Vomiting <ref name="Shore et al" /> | ||
Advanced Cancer symptoms: | |||
Weight Loss | *Weakness or very feeling tired | ||
*Loss of appetite or fullness <br> | |||
Abdominal or Back Pain | |||
Gallbladder Enlargement | |||
Dark Urine | |||
Nausea and Vomiting | |||
Advanced Cancer symptoms: | |||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
Diabetes<ref name="Extermann">Extermann M. Interaction between comorbidity and cancer. Cancer Control 2007;14(1):13-22</ref> | [[Diabetes]]<ref name="Extermann">Extermann M. Interaction between comorbidity and cancer. Cancer Control 2007;14(1):13-22</ref> | ||
== Treatment == | |||
[[Image:Kwhipple.jpg|alt=|right|frameless]]Most tumours are not resectable at diagnosis. | |||
* Surgery for stage I and II does offer the chance of cure, though with high morbidity (20-30%) and mortality (5%). | |||
Even when resection is possible, the majority of patients succumb to recurrence, with only a doubling of survival in operated patients 1, from 5% to 10% at 5 years. At 12 months following the diagnosis, almost a quarter of the patients will have died<ref name=":1" />. | |||
If the cancer has spread and it is not possible to cure it with surgery, the doctor may still recommend treatment that focuses on improving quality of life by relieving the symptoms (this is called [[Palliative Care Competence Framework for Physiotherapists|palliative]] treatment)<ref name=":0" />. | |||
== Diagnosis == | |||
[[Image:Ct scan.png|alt=|right|frameless]] | |||
* [[Blood Tests|Blood tests]] – to check how well the liver and kidney are working and measure for a protein known as CA19.9. | |||
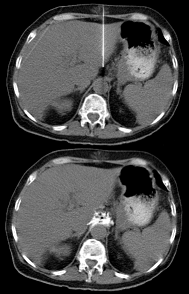
* Computed Tomography Scan( [[CT Scans|CT Scan]]) | |||
* Magnetic resonance imaging ([[MRI Scans|MRI]]) | |||
* [[Ultrasound Scans|Ultrasound]] | |||
* Endoscopy (also called endoscopic retrograde cholangiopancreatography, ERCP) | |||
* Laparoscopy – the internal organs are examined with an instrument inserted into the abdomen through a small cut. | |||
* Tissue biopsy – a small sample of the pancreas is removed with a needle and examined in a laboratory. | |||
* Positron emission tomography (PET) scan – an injection with a glucose solution containing a very small amount of radioactive material is given. The scanner can ‘see’ the radioactive substance. Cancerous cells show up as ‘hot spots’ – areas where the glucose is being taken up. | |||
These tests also help the doctor find out if the cancer has spread. The cancer may have spread into blood vessels or lymph nodes near the pancreas, or into organs further away, like the liver or the lungs. This is called ‘secondary cancer’ or metastasis. The tests help doctors decide the best treatment.<ref name=":2" /> | |||
== Systemic Involvement == | == Systemic Involvement == | ||
Pancreatic cancers are often diagnosed in advanced stages where the cancer has metastasized to other areas. Pancreatic cancers can metastasize to regional lymph nodes, liver, lungs, duodenum, stomach, colon, and anywhere in the abdominal cavity. Pancreatic cancer can spread to the skin as painful nodules. Usual sites for metastases in pancreatic cancer occur in the liver and peritoneal cavity<ref name="Borad et el">Borad MJ, Saadati H, Lakshmipathy A, Campbell E, Hopper P, Jameson G, Von Hoff DD, Wasif Saif M. Skeletal metastases in pancreatic cancer: a retrospective study and review of the literature. Yale Journal of Biology and Medicine 2009;82:1-6</ref>. | Pancreatic cancers are often diagnosed in advanced stages where the cancer has metastasized to other areas. Pancreatic cancers can metastasize to regional lymph nodes, liver, lungs, duodenum, stomach, colon, and anywhere in the abdominal cavity. Pancreatic cancer can spread to the skin as painful nodules. Usual sites for metastases in pancreatic cancer occur in the liver and peritoneal cavity<ref name="Borad et el">Borad MJ, Saadati H, Lakshmipathy A, Campbell E, Hopper P, Jameson G, Von Hoff DD, Wasif Saif M. Skeletal metastases in pancreatic cancer: a retrospective study and review of the literature. Yale Journal of Biology and Medicine 2009;82:1-6</ref>. | ||
== Physical Therapy Management == | |||
Physical therapy management involves helping the patient live a functional life while dealing with pain, fatigue, and weakness. The patient feels he/she is not able to do much because of the disease and its implications. | |||
Physical therapy management involves helping the patient live a functional life | |||
"Disability in patients with advanced cancer often results from bed rest, deconditioning, and neurologic and musculosketal complications of cancer or cancer treatment. Terminally ill patients have a high prevelance of weakness, pain, fatigue, and dyspnea in addition to other symptoms."<ref name="Santiago-Palma et al">Santiago-Palma J, Payne R. Palliative care and rehabilitation. Cancer Supplement 2001;92(4):1049-1052</ref>Improvement in functional ability is necessary for a patient with a diagnosis of cancer to enjoy a quality of life. "Clinical experience suggests that the application of the fundamental principles of rehabilitation medicine is likely to improve care."<ref name="Santiago-Palma et al" /> Physical training had a significant and beneficial effects on reducing fatigue<ref name="van Weert et al">van Weert EV, May AM, Korstjens I, Post WJ, van der Schans CP, van den Borne B, Mesters I, Ros WJG, Hoekstra-Weebers JEHM. Cancer-related fatigue and rehabilitation: a randomized controlled multicenter trial comparing physical training combined with congnitive-behavioral therapy with physical training only and with no intervention. Physical Therapy 2010;90(10):1413-1425</ref>. | |||
The physical therapy management will consist of controlling symptoms of pain, reducing fatigue, and strengtening weak muscles. Along with these 3 focal points, impairments should be addressed to improve functional abilities. "When patients are terminally ill, both symptom control and maintenance of function become central aspects of their treatment."<ref name="Santiago-Palma et al" /> Patients who have advanced cancer will have symptoms of pain, fatigue, generalized weakness, dyspnea, delirium, nausea, vomiting, [[depression]], and anxiety<ref name="Santiago-Palma et al" />. The physical therapist will need to address these symptoms in order for the patient to become independent and reduce the burden of caregivers. "Two-hundred thirty nine of 301 patients had difficulties with activities of daily living. A mean 27% improvement in the Barthel mobility index was recorded following rehabilitation."<ref name="Santiago-Palma et al" /> | |||
< | Pain is one of the most common symptom of cancer and its advancing state. Severe pain in patients with cancer leads to impaired function. "Knowledge of the biology and natural history of the specific cancer types, including familiarity with common cancer pain syndromes and opioid pharmacology, are important in assessing and managing these patients."<ref name="Santiago-Palma et al" /> | ||
Physical therapy modalities can also be used for treatment of pain but with caution. "The use of physical modalities such as massage, heat, and cold can be implemented at bedside and aid in the pain management of patients."<ref name="Santiago-Palma et al" /> Heat can be utilized when performing ROM exercises in order to reduce the symptoms of pain. "Heat should not be applied to skin areas that are insensitive, have been exposed to radiation, or are atrophic or acutely inflamed."<ref name="Santiago-Palma et al" /> Cold therapy should not also be applied to these areas<ref name="Santiago-Palma et al" />. | |||
<br> | Providing the patient with education on about the cancer and its implications can also be beneficial in physical therapy management. Energy conservation and work simplification can also assist patients in reducing and controlling symptoms<ref name="Santiago-Palma et al" />. Patient education can also include the use of [[Assistive Devices|assistive devices]] if necessary. "Immune function may be improved by moderate exercise."<ref name="Santiago-Palma et al" /> Exercise should be implemented at low intensity levels<ref name="Santiago-Palma et al" />.<br> | ||
== Differential Diagnosis == | |||
Typically, at the time of diagnosis of pancreatic cancer, 52% have distant metastasis, and 23% have local spread. | |||
= | Differential diagnosis before imaging and biopsy includes the following: acute pancreatitis, chronic [[Pancreatitis|pancreatitis,]] cholangitis, [[cholecystitis]], choledochal cyst, [[Peptic Ulcers|peptic ulcer disease,]] cholangiocarcinoma, and [[Gastric Cancer|gastric cancer]].<ref name=":2" /> | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category: | [[Category:Oncology]] | ||
[[Category:Medical]] | |||
[[Category:Bellarmine_Student_Project]] | |||
Latest revision as of 12:33, 4 December 2023
Original Editors - Jaimin Shah from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Jaimin Shah, Admin, Elaine Lonnemann, Lucinda hampton, WikiSysop, Kirenga Bamurange Liliane, Wendy Walker, Evan Thomas, Kim Jackson and Chelsea Mclene
Definition/Description[edit | edit source]
Pancreatic Cancer is a malignant disease of the pancreas. “Pancreatic adenocarcinoma is a highly lethal disease, which is usually diagnosed in an advanced state.”[1] The malignant tumor can be located near the head, body, or the tail of the pancreas. The pancreas is an organ that helps secrete insulin and glucagon which helps control blood glucose levels in the body. Pancreatic cancer is the fourth common cancer among men and the fifth leading cause of cancer in women. There are two types of pancreatic cancers which are exocrine cancer and endocrine cancer. “Pancreatic ductal adenocarcinoma (PDAC) compromises 90% of pancreatic cancers.”[2] Exocrine pancreatic cancers are the most common of pancreatic cancers. Exocrine pancreatic cancer is involved in the ducts of the pancreas that secrete juices.
Key Points
- The pancreas is a gland that secretes digestive enzymes and insulin.
- The symptoms of pancreatic cancer are often vague and common to many other disorders.
- Pancreatic cancer is often only diagnosed in its later stages, which makes it difficult to treat.[3]
Epidemiology[edit | edit source]
- Pancreatic cancer accounts for 22% of all deaths due to gastrointestinal malignancy, and 5% of all cancer deaths. In general, it is a malignancy of the elderly with over 80% of cases occurring after the age of 60.[4]
- Pancreatic cancer is the fourth most common cause of cancer death for men and women in US.[5]
- Pancreatic cancer is more common in black men and women than whites.
Pancreatic cancer is rare in people under the age of 45, the risk increases after age of 50.
Etiology[edit | edit source]
Risk factors include:
- cigarette smoking: the strongest environmental risk factor
- a diet rich in animal fats and protein
- obesity
- family history: three or more first-order relatives with pancreatic cancer results in ~20x risk
- hereditary syndromes[4]
- Possible risk factors include heavy alcohol consumption, coffee consumption, physical inactivity, high red meat consumption, and two or more soft drinks per day.
- Ten percent have a genetic cause such as genetic mutations or association with syndromes eg multiple endocrine neoplasia type 1[6].
Characteristics/Clinical Presentation[edit | edit source]
Most clinical presentations of pancreatic cancers are vague and delay the potential diagnosis. “Pancreatic cancer is relatively asymptomatic during its early course. The vague presentation includes back and epigastric pain.”[2] Symptoms associated with pancreatic cancer include:
- Pain is the presenting symptom in between 31% and 71% of pancreatic cancer patients
- Jaundice
- Digestive Problems
- Blood Clots
- Weight Loss
- Abdominal or Back Pain
- Gallbladder Enlargement
- Dark Urine
- Nausea and Vomiting [2]
Advanced Cancer symptoms:
- Weakness or very feeling tired
- Loss of appetite or fullness
Associated Co-morbidities[edit | edit source]
Treatment[edit | edit source]
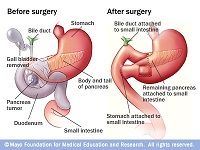
Most tumours are not resectable at diagnosis.
- Surgery for stage I and II does offer the chance of cure, though with high morbidity (20-30%) and mortality (5%).
Even when resection is possible, the majority of patients succumb to recurrence, with only a doubling of survival in operated patients 1, from 5% to 10% at 5 years. At 12 months following the diagnosis, almost a quarter of the patients will have died[4].
If the cancer has spread and it is not possible to cure it with surgery, the doctor may still recommend treatment that focuses on improving quality of life by relieving the symptoms (this is called palliative treatment)[3].
Diagnosis[edit | edit source]
- Blood tests – to check how well the liver and kidney are working and measure for a protein known as CA19.9.
- Computed Tomography Scan( CT Scan)
- Magnetic resonance imaging (MRI)
- Ultrasound
- Endoscopy (also called endoscopic retrograde cholangiopancreatography, ERCP)
- Laparoscopy – the internal organs are examined with an instrument inserted into the abdomen through a small cut.
- Tissue biopsy – a small sample of the pancreas is removed with a needle and examined in a laboratory.
- Positron emission tomography (PET) scan – an injection with a glucose solution containing a very small amount of radioactive material is given. The scanner can ‘see’ the radioactive substance. Cancerous cells show up as ‘hot spots’ – areas where the glucose is being taken up.
These tests also help the doctor find out if the cancer has spread. The cancer may have spread into blood vessels or lymph nodes near the pancreas, or into organs further away, like the liver or the lungs. This is called ‘secondary cancer’ or metastasis. The tests help doctors decide the best treatment.[6]
Systemic Involvement[edit | edit source]
Pancreatic cancers are often diagnosed in advanced stages where the cancer has metastasized to other areas. Pancreatic cancers can metastasize to regional lymph nodes, liver, lungs, duodenum, stomach, colon, and anywhere in the abdominal cavity. Pancreatic cancer can spread to the skin as painful nodules. Usual sites for metastases in pancreatic cancer occur in the liver and peritoneal cavity[8].
Physical Therapy Management[edit | edit source]
Physical therapy management involves helping the patient live a functional life while dealing with pain, fatigue, and weakness. The patient feels he/she is not able to do much because of the disease and its implications.
"Disability in patients with advanced cancer often results from bed rest, deconditioning, and neurologic and musculosketal complications of cancer or cancer treatment. Terminally ill patients have a high prevelance of weakness, pain, fatigue, and dyspnea in addition to other symptoms."[9]Improvement in functional ability is necessary for a patient with a diagnosis of cancer to enjoy a quality of life. "Clinical experience suggests that the application of the fundamental principles of rehabilitation medicine is likely to improve care."[9] Physical training had a significant and beneficial effects on reducing fatigue[10].
The physical therapy management will consist of controlling symptoms of pain, reducing fatigue, and strengtening weak muscles. Along with these 3 focal points, impairments should be addressed to improve functional abilities. "When patients are terminally ill, both symptom control and maintenance of function become central aspects of their treatment."[9] Patients who have advanced cancer will have symptoms of pain, fatigue, generalized weakness, dyspnea, delirium, nausea, vomiting, depression, and anxiety[9]. The physical therapist will need to address these symptoms in order for the patient to become independent and reduce the burden of caregivers. "Two-hundred thirty nine of 301 patients had difficulties with activities of daily living. A mean 27% improvement in the Barthel mobility index was recorded following rehabilitation."[9]
Pain is one of the most common symptom of cancer and its advancing state. Severe pain in patients with cancer leads to impaired function. "Knowledge of the biology and natural history of the specific cancer types, including familiarity with common cancer pain syndromes and opioid pharmacology, are important in assessing and managing these patients."[9]
Physical therapy modalities can also be used for treatment of pain but with caution. "The use of physical modalities such as massage, heat, and cold can be implemented at bedside and aid in the pain management of patients."[9] Heat can be utilized when performing ROM exercises in order to reduce the symptoms of pain. "Heat should not be applied to skin areas that are insensitive, have been exposed to radiation, or are atrophic or acutely inflamed."[9] Cold therapy should not also be applied to these areas[9].
Providing the patient with education on about the cancer and its implications can also be beneficial in physical therapy management. Energy conservation and work simplification can also assist patients in reducing and controlling symptoms[9]. Patient education can also include the use of assistive devices if necessary. "Immune function may be improved by moderate exercise."[9] Exercise should be implemented at low intensity levels[9].
Differential Diagnosis[edit | edit source]
Typically, at the time of diagnosis of pancreatic cancer, 52% have distant metastasis, and 23% have local spread.
Differential diagnosis before imaging and biopsy includes the following: acute pancreatitis, chronic pancreatitis, cholangitis, cholecystitis, choledochal cyst, peptic ulcer disease, cholangiocarcinoma, and gastric cancer.[6]
References[edit | edit source]
- ↑ Li C, Heidt DG, Dalerba P, Burant CF, Zhang L, Adsay V, Wicha M, Clarke MF, Simeone DM. Identification of pancreatic stem cells. Cancer research. 2007 Feb 1;67(3): 1030-1037
- ↑ 2.0 2.1 2.2 Shore S, Vimalachadran D, Raraty MGT, Ghaneh P. Cancer in the elderly: pancreatic cancer. Surgical Onocology 2004;13:201-210
- ↑ 3.0 3.1 Better Health Pancreratic Cancer Available:https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pancreatic-cancer#diagnosis-of-pancreatic-cancer (accessed 3.9.2021)
- ↑ 4.0 4.1 4.2 Radiopedia pancreatic Cancer Available: https://radiopaedia.org/articles/pancreatic-ductal-adenocarcinoma-2 (accessed 3.9.2021)
- ↑ Farma JM, Santillan AA, Melis M, Walters J, Belinc D, Chen D, Eikman EA, Malafa M. PET/CT fusion scan enhances CT staging in patients with pancreatic neoplasms. Annals of Surgical Oncology 2008;15(9):2465-2471
- ↑ 6.0 6.1 6.2 Puckett Y, Garfield K. Pancreatic Cancer. InStatPearls [Internet] 2021 Aug 11. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK518996/ (accessed 3.9.2021)
- ↑ Extermann M. Interaction between comorbidity and cancer. Cancer Control 2007;14(1):13-22
- ↑ Borad MJ, Saadati H, Lakshmipathy A, Campbell E, Hopper P, Jameson G, Von Hoff DD, Wasif Saif M. Skeletal metastases in pancreatic cancer: a retrospective study and review of the literature. Yale Journal of Biology and Medicine 2009;82:1-6
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 Santiago-Palma J, Payne R. Palliative care and rehabilitation. Cancer Supplement 2001;92(4):1049-1052
- ↑ van Weert EV, May AM, Korstjens I, Post WJ, van der Schans CP, van den Borne B, Mesters I, Ros WJG, Hoekstra-Weebers JEHM. Cancer-related fatigue and rehabilitation: a randomized controlled multicenter trial comparing physical training combined with congnitive-behavioral therapy with physical training only and with no intervention. Physical Therapy 2010;90(10):1413-1425