Palliative Care Competence Framework for Physiotherapists
Introduction[edit | edit source]
The Palliative Care Competence Framework for Physiotherapists was designed to standardise education for undergraduates and postgraduates in Europe. It provides a guide for the acquirement of knowledge, skills and attributes needed for clinical practice in health and social care professions. This document provides flexibility and autonomy in order to develop core and discipline specific competencies which can be applied to both generalist and specialist palliative care. [1]
Core Competencies[edit | edit source]
When caring for people with life-limiting conditions who may have complex care needs, a multidisciplinary approach is preferred. The core competencies outlined in the guide are common to all health professionals and convey the primary level of understanding that is essential to provide palliative care.
There are 6 domains of competency:
- Principles of palliative care
- Communication
- Optimising comfort and quality of life
- Care planning and collaborative practice
- Loss, grief and bereavement
- Professional and ethical practice in the context of palliative care
Each domain is defined with a statement which remains the same regardless of the setting where care is provided. Each domain has an indicator that outlines the competences required by professionals depending on the context of their roles and the level that palliative care is provided. The indicators are based on advanced knowledge, skills and understanding and clinical expertise. The indicators are named “ALL”, “SOME” and “FEW” and are outlined below -
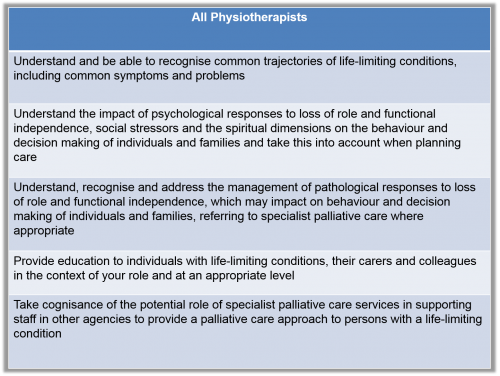
Principles of Palliative Care[edit | edit source]
The aim of palliative care is to improve the quality of life of people who are suffering with life-limiting conditions. This care does not only include the physical facet of their condition but the social, psychological and spiritual aspects also. Palliative care is applicable for people of all ages and may be introduced at any point in a disease trajectory.
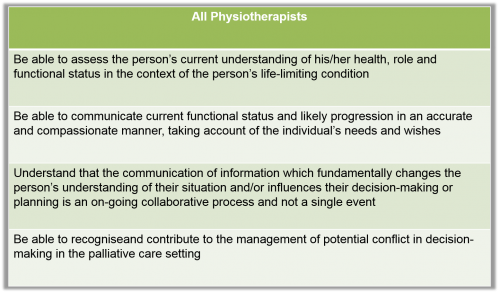
Communication[edit | edit source]
Communication is an essential component to the delivery of palliative care. When caring for people with complex and life-threatening conditions, good communication is important particularly when bad news needs to be relayed or when difficult decisions regarding treatment need to be made. Communication is imperative when circumstances are uncertain or when distress and strong emotions arise.
Communication is a method of:
- Enabling therapeutic relationships with patients and families
- Ensuring that the patient and family are key components in decision making regarding care
- Enabling effective inter-professional or inter-agency teamwork
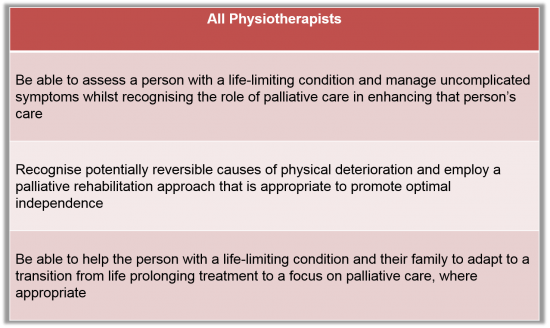
Optimising Comfort and Quality of Life[edit | edit source]
People receiving palliative care are not only affected by the physical symptoms of their condition but also the psychological, spiritual and social aspects. Optimising quality of life for people is a dynamic process that involves acknowledging, anticipating, continuously assessing and responding to a range of complex symptoms and needs. The process must be done in a proactive manner to relieve suffering.
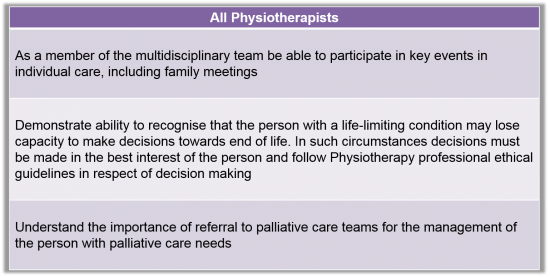
Care Planning and Collaborative Practice[edit | edit source]
In palliative care, care planning involves co-ordinating and integrating person-centred care to promote quality of life. Patients and their families should engage in the process and concerns from families or carers should be considered.
Planning involves:
- Assessing need
- Promoting and preserving a person’s choice
- Predicting likely problems
- Planning for the future in the wake of a changing or deteriorating disease trajectory.
Care planning should ensure that multi- disciplines and agencies can be referred to as required.
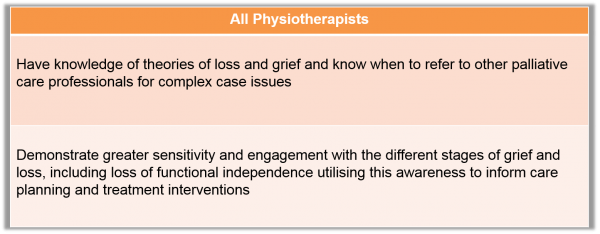
Loss, Grief and Bereavement[edit | edit source]
Dealing with loss, grief and bereavement is an intrinsic part of palliative care. A minority of people may be at risk of developing difficulties during their grieving. Professionals using a palliative care approach have an essential role to play for all but in particular for those who may require bereavement therapy or counselling by providing support and information.
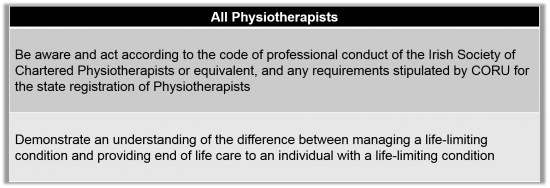
Professional and Ethical Practice in the Context of Palliative Care[edit | edit source]
There may be a time when specific treatments or interventions are futile or burdensome. Deference in palliative care refers to the importance of respecting the patient’s wishes, needs and values when dealing with a life-limiting condition. Professional and ethical practice concerns the best way to provide continuing care as people’s care needs change during the course of their condition. It guides professionals to reflect on their contribution to a person’s care and the contribution of other professionals.
Guidelines[edit | edit source]
While the principles of palliative care have remained relatively the same over the past number of years, the evidence base surrounding interventions and how care should be delivered is constantly evolving. The NICE guidelines - End of Life Care for Adults is one of the most recent guidelines available[2]. NICE guidelines are classed as high quality evidence and is an excellent resource for not only newly qualified professionals but for anyone working in the field of palliative care.
References[edit | edit source]
- ↑ Palliative Care Competence Framework Steering Group. Palliative Care Competence Framework. http://www.hse.ie/eng/about/Who/clinical/natclinprog/palliativecareprogramme/Resources/competencyframework.pdf (accessed 20 Nov 2015).
- ↑ End of life care for adults: service delivery NICE guideline [NG142]Published: 16 October 2019 Available:https://www.nice.org.uk/guidance/NG142 (accessed 13.12.2023)