|
|
| (47 intermediate revisions by 12 users not shown) |
| Line 1: |
Line 1: |
| <div class="noeditbox">Welcome to [[Pathophysiology of Complex Patient Problems|PT 635 Pathophysiology of Complex Patient Problems]] This is a wiki created by and for the students in the School of Physical Therapy at Bellarmine University in Louisville KY. Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!</div><div class="editorbox">
| | <div class="editorbox"> |
| '''Original Editors '''- Paul Clark & Sam Holzknecht from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | | '''Original Editors '''- Paul Clark and Sam Holzknecht from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] |
|
| |
|
| '''Lead Editors''' - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]] | | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} |
| </div> | | </div> |
| == Definition/Description ==
| |
|
| |
|
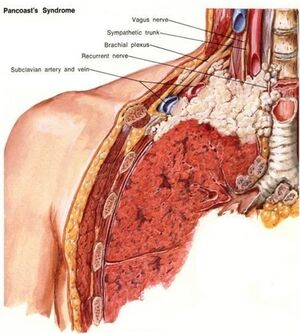
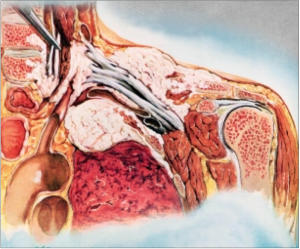
| A pancoast tumor is an uncommon lung cancer that arises at the level of the superior sulcus and is limited to the apical segment of either lung. <ref name="1">Muscolino G, Valente M, Andreani M. Pancoast tumours: clinical assessment and long term results of combined radio surgical treatment. Thorax. 1997; 52:284-6</ref> This is a form of non-small-cell carcinomas (NSCLCs) that are very difficult to treat because of their proximity and frequent metastasis to adjacent structures such as the subclavian vessels, lymphatic system, brachial plexus, spine, second and third ribs, stellate ganglion, and the sympathetic nervous system. <ref name="2">Archie VC, Thomas Jr. CR. Superior sulcus tumors: a mini-review. The oncologist lung cancer. 2004;9:550-5</ref> NSCLCs generally grow and spread slower and are divided into three different forms of cancer: squamous cell carcinomas (45-50%), adenocarcinomas (36-38%), or undifferentiated large-cell carcinomas (11-13%). <ref name="3">Parissis H, Young V. Treatment of pan coast tumors from the surgeons prospective: re-appraisal of the anterior-manubrial sternal approach. J of cardiothoracic surgery. 2010; 5:102.</ref> Rather than invading underlying lung tissue, this tumor presents as an abnormal patch of tissue over the lung apex and initially involves the chest wall structures. This can be treated if caught early on before it spreads and moves to the lymph nodes. Pancoast tumors are often mis-diagnosed and/or diagnosed too late.<ref name="4">Aigner C, Klepetko W. Current treatment concepts of pancoast tumors. European surgery. 2010; 42(5):214-9</ref><br>
| | == Introduction == |
| | [[File:Pancoast drawing.jpg|thumb|Pancoast Tumour]] |
| | A pancoast tumour is a relatively uncommon primary lung cancer forming in the lung apex and invading the surrounding soft tissues. This is a tumour type is hard to difficult to treat because of its closeness, and frequent metastasis, to adjacent structures such as the subclavian vessels, [[Lymphatic System|lymphatic system]], [[Brachial Plexus|brachial plexus]], spine, second and third [[ribs]], stellate [[ganglion]], and the [[Sympathetic Nervous System|sympathetic nervous system]].<ref name="p2">Archie V, Thomas C. Superior sulcus tumors: a mini-review. The Oncologist [serial on the Internet]. (2004), [cited April 4, 2012]; 9(5): 550-555. Available from: MEDLINE.</ref> Pancoast tumors are often mis-diagnosed and/or diagnosed too late.<ref name="p4">Aigner C, Klepetko W. Current treatment concepts of Pancoast tumors. European Surgery: ACA Acta Chirurgica Austriaca [serial on the Internet]. (2010, Oct), [cited April 4, 2012]; 42(5): 214-219. Available from: Academic Search Premier.</ref> |
|
| |
|
| <br>
| | == Etiology == |
| | Common risk factors include (similar to lung cancer): |
|
| |
|
| [[Image:Tumor.png|248x300px|Tumor located at the apex of the lungs.]]
| | *[[Smoking Cessation and Brief Intervention|Smoking]] |
| | *Secondhand smoke |
| | *Asbestos exposure |
| | *Exposure to industrial elements like gold or nickel |
| | *Diesel exhaust<ref name="p1">Muscolino G, Valente M, Andreani M. Pancoast tumours: clinical assessment and long term results of combined radio surgical treatment. Thorax. 1997; 52:284-6</ref> |
| | == Epidemiology == |
| | Pancoast tumours account for 3-5% of all bronchogenic [[Oncological Disorders|carcinomas]] and having demographics similar to other [[Lung Cancer|lung cancers]] (see link). |
|
| |
|
| <br> | | == Characteristics/Clinical Presentation == |
| | [[File:Bc_pancoast_mr.JPG|alt=|thumb|167x167px|Pancoast MRI]] |
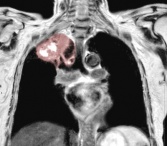
| | Symptom commonly include: chest shoulder and/or arm pain; weight loss (frequently present). Pancoast syndrome occurs in 25% cases and includes: severe pain in the shoulder region radiating toward the axilla and [[scapula]] along the ulnar aspect of the muscles of the hand; atrophy of hand and arm muscles; [[Horner's Syndrome|Horner syndrome]] (ptosis, miosis, hemianhidrosis, enophthalmos); and compression of the blood vessels with edema."<ref name="p0">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview</ref><ref name=":0">Radiopedia [https://radiopaedia.org/articles/pancoast-tumour Pancoast Tumour] Available:https://radiopaedia.org/articles/pancoast-tumour (accessed 24.1.2023)</ref> |
| | == Diagnosis == |
|
| |
|
| Pancoast tumors may occur in the three compartments of the thoracic inlet and symptoms are related to the location.
| | Diagnosis is often difficult and delayed due to the typical absence of lung cancer symptoms and includes a combination of CT scans and MRI followed by a biopsy confirmation <ref name="p2" />. |
| | |
| [[Image:Compartments.png|400x358px]]
| |
| | |
| '''Anterior Middle'''<br>
| |
| | |
| [[Image:Pancoast tumor Anterior.png|300x198px]] [[Image:Pancoast tumor middle.png|300x200px]]
| |
| | |
| '''Posterior'''
| |
| | |
| [[Image:Pancoast tumor posterior.png|300x201px]]
| |
| | |
| == Prevalence ==
| |
| | |
| "Lung cancers are the leading cause of death in both men and women in North American."<ref name="8">Kim P, Hains F, Wallace MC, Mior SA. Pancoast tumour: a case report. The journal of the CCA. 1993 December; 37(4):214-20.</ref> In 2011, there was an estimated new diagnosis of 221,130 new cases of lung cancer with 156,940 deaths relating to lung cancer. Lung cancer accounts for more deaths when compared to prostate/breast, colon, and pancreatic cancer combined.<ref name="5">Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011. CA: A Cancer journal for clinicians. 2011;61:212–36.</ref> Of the number of new lung cancer diagnosis, approximately 5% can be attributed to pancoast tumors.<ref name="6">Gofeld M, Bhatia A. Alleviation of pancoast's tumor pain by ultrasound-guided percutaneous ablation of cervical nerve roots. Pain practice. 2008; 8(4): 314-9.</ref> The highest occurrence is found in men between the ages of 40 and 60 with a history of smoking. <br><br>
| |
| | |
| [[Image:Smoking.jpg]]
| |
| | |
| == Characteristics/Clinical Presentation ==
| |
| | |
| Pancoast tumors are very difficult to diagnosis early on. This is based on their low prevalence rate and many differential diagnosis'. "Typical" symptoms of lung cancer such as cough, dyspnea, and hemoptysis are less frequent.<ref name="4">Aigner C, Klepetko W. Current treatment concepts of pancoast tumors. European surgery. 2010; 42(5):214-9.</ref>
| |
| | |
| Pancoast syndrome includes: "(1) severe pain in the shoulder region radiating toward the axilla and scapula along the ulnar aspect of the muscles of the hand, (2) atrophy of hand and arm muscles, (3) Horner syndrome (ptosis, miosis, hemianhidrosis, enophthalmos), and (4) compression of the blood vessels with edema."<ref name="10">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview</ref>
| |
| | |
| '''Common presentations include:<br>'''
| |
| | |
| pancoast syndrome
| |
| | |
| pain is relieved by propping up arm on table or holding with other arm
| |
| | |
| radiating pain to the ulnar side of the arm and hand (55-60%)<ref name="3">Parissis H, Young V. Treatment of pan coast tumors from the surgeons prospective: re-appraisal of the anterior-manubrial sternal approach. J of cardiothoracic surgery. 2010; 5:102.</ref>
| |
| | |
| Horner's syndrome (30%)<ref name="3">Parissis H, Young V. Treatment of pan coast tumors from the surgeons prospective: re-appraisal of the anterior-manubrial sternal approach. J of cardiothoracic surgery. 2010; 5:102.</ref><br>
| |
| | |
| parasthesias of the hand<ref name="2">Archie VC, Thomas Jr. CR. Superior sulcus tumors: a mini-review. The oncologist lung cancer. 2004;9:550-5</ref>
| |
| | |
| between the ages of 40-60<ref name="5">Kim P, Hains F, Wallace MC, Mior SA. Pancoast tumour: a case report. The journal of the CCA. 1993 December; 37(4):214-20.</ref>
| |
| | |
| men > female<ref name="5">Kim P, Hains F, Wallace MC, Mior SA. Pancoast tumour: a case report. The journal of the CCA. 1993 December; 37(4):214-20.</ref>
| |
| | |
| == Associated Co-morbidities ==
| |
| | |
| muscle atrophy<ref name="2">Archie VC, Thomas Jr. CR. Superior sulcus tumors: a mini-review. The oncologist lung cancer. 2004;9:550-5.</ref><br>
| |
| | |
| cervical radiculopathy
| |
| | |
| Horner's Syndrome<ref name="10">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview.</ref>
| |
| | |
| COPD
| |
| | |
| vertebrae compression<ref name="10">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview.</ref>
| |
| | |
| bone cancer
| |
| | |
| == Medications ==
| |
| | |
| Pharmacotherapy goals are to induce remission, reduce morbidity, and prevent complications <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref>
| |
| | |
| '''<br>Opioid Analgesics''': Primary treatment of pain that can be combined with NSAIDs and may be a short-acting potent opioid such as oxycodone or an immediate-release morphine or methadone<ref name="8">Petraglia, Md JF. International Pain Medical Group. [homepage on the Internet]. 2008 [cited 2012 Mar 30]. Available from: http://www.gotpaindocs.com/pancsts_tmor_syndrm.htm</ref>.
| |
| | |
| '''<br>Antineoplastic agents:''' Inhibit cell growth and proliferation and are used in a variety of different cancers including head, neck, breast, testicular and ovarian cancer <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref>.
| |
| | |
| '''<br>Cisplatin (Platinol): '''Alkylating agent causing intrastrand and interstrand cross-linking of DNA that leads to strand breakage. It has a broad range of antitumor activity and forms backbone of currently available approved combination chemotherapy regimens that cause Pancoast syndrome. Its administered via IV in isotonic sodium chloride solution (0.9%) or sodium chloride and glucose. Adequate hydration must be maintained up to 24 hours after a dose and Renal, hematological, auditory, and neurological function must be monitored <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref>.
| |
| | |
| <br>'''Etoposide (Toposar, VePesid):''' Semisynthetic derivative of podophyllotoxin with antineoplastic properties interferes with topoisomerase II function thus inhibiting DNA synthesis <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref>.<br><br><br>
| |
| | |
| == Diagnostic Tests/Lab Tests/Lab Values ==
| |
| | |
| Diagnosis is often difficult and delayed due to the typical absence of lung cancer symptoms and includes a combination of CT scans and MRI followed by a biopsy confirmation <ref name="12">Lynne Eldridge Md. What Is a Pancoast Tumor? [homepage on the Internet]. March 4th, 2012 [cited 2012 Mar 30]. Available from: http://lungcancer.about.com/od/typesoflungcancer/f/pancoasttumor.htm</ref>.
| |
| | |
| <br>'''Chest x-ray: '''Difficult early detection due to limited visualization of the top of the lung but may reveal asymmetries like a small, uniform patch of tissue or pleural thickening on the apex of one lung, invasion of the ribs or vertebrae and enlargement of the mediastinum <ref name="11">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview</ref> (Apical lordotic films may be more revealing) <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref>.
| |
| | |
| [[Image:132 pancoast1.jpg|157x172px]]
| |
| | |
| <br>'''MRI:''' Most accurate at displaying the extent of the involvement and invasion of nearby structures including the brachial plexus, subclavian vessels, spine, and neural foramina. Contrast can be used to better display the local extent of the damage <ref name="10">Rusch, Md VW, Management of Pancoast tumours. The Lancet Oncology Nov 27, 2006; 7(12):997–1005.</ref><ref name="11">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview</ref>.
| |
| | |
| [[Image:Bc pancoast mr.JPG|168x146px]]
| |
| | |
| '''CT scan:''' Displays involvement of the brachial plexus, chest wall, mediastinum, liver, adrenal glands, pulmonary nodules, vertebra, vena cava, trachea, and esophagus and contrast can be utilized to see involvement of blood vessels under the clavicle. CT scan is less expensive, more available and more effective than the MRI at assessing the mediastinum to determine if the tumor has involved the lymph nodes <ref name="10">Rusch, Md VW, Management of Pancoast tumours. The Lancet Oncology Nov 27, 2006; 7(12):997–1005.</ref><ref name="11">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview</ref>. This is essential in detecting N2 mediastinal lymphadenopathy which has a significant adverse effect on survival but only present in 20% of cases <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref><ref name="13">Aigner C, Klepetko W. Current treatment concepts of Pancoast tumors. European Surgery: ACA Acta Chirurgica Austriaca Oct 2010; 42(5):214-219.</ref>. '' (Pictures can be seen above under description)''<br>
| |
| | |
| <br> MRI and CT scan of the brain is often performed at the initial evaluation to check for distant metastases to the brain which is the most common site of metastasis and failure in pancoast tumor <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref>
| |
| | |
| <br>'''Arteriogram or a venogram: '''Look at the involvement of the subclavian artery/vein under the clavicle <ref name="11">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview</ref>
| |
| | |
| <br>'''Bronchoscopy:''' Involvement of the tracheal and bronchial cavities and used in excluding unsuspected concurrent endobronchial lesions <ref name="11">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview</ref><ref name="12">Lynne Eldridge Md. What Is a Pancoast Tumor? [homepage on the Internet]. March 4th, 2012 [cited 2012 Mar 30]. Available from: http://lungcancer.about.com/od/typesoflungcancer/f/pancoasttumor.htm</ref>
| |
| | |
| <br>'''Biopsy:''' 90% of patients can be correctly diagnosed based on clinical and radiological findings alone but 95% can be diagnosed through percutaneous, supraclavicular fine-needle aspiration biopsy that’s fluoroscopy or CT guided <ref name="11">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview</ref><ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref>. Transthoracic needle biopsy with CT guidance has a high yield of 95% and some tumors maybe only evaluated by open or video assisted thoracotomy.
| |
| | |
| <br>'''Mediastinoscopy:''' Samples of lymph nodes are taken at the lowest part of the neck behind the breastbone to determine if the tumor has spread into the mediastinum.
| |
| | |
| <br>'''Sputum cytology:''' results are positive in fewer than 15% of patients <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref>.
| |
| | |
| <br>'''PET scans:''' Help identify involved lymph nodes and the distant spread of cancer <ref name="11">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview</ref> and is used in staging non–small cell lung cancer<ref name="12">Lynne Eldridge Md. What Is a Pancoast Tumor? [homepage on the Internet]. March 4th, 2012 [cited 2012 Mar 30]. Available from: http://lungcancer.about.com/od/typesoflungcancer/f/pancoasttumor.htm</ref>.
| |
| | |
| <br>'''Liver and bone scans: '''determine if the cancer has spread <ref name="11">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview</ref>.
| |
| | |
| <br>'''Staging:''' Based on scalene node biopsy results of palpable lymph nodes or mediastinoscopy findings <ref name="11">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview</ref>. American Joint Committee on Cancer (AJCC) and the Union Internationale Contre le Cancer (UICC) have adopted the International System for Staging Lung Cancer that’s based on characteristics and distribution of the tumor… <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref><br> • T describes the size and invasiveness of the primary tumor<br> o T3 = tumor of any size that invades the chest wall (parietal pleura). <br> o T4 = tumor of any size that invades the vertebral body, neural or vascular structure, mediastinum, esophagus, or trachea. <br> • N describes the distribution of positive lymph nodes: <br> o N1 = metastasis to ipsilateral peribronchial or hilar nodes<br> o N2 = spread to ipsilateral mediastinal and/or subcarinal nodes<br> o N3 = metastasis to nodes of the contralateral hilar and mediastinal areas or scalene or supraclavicular nodes, either ipsilateral or contralateral.
| |
| | |
| • M describes the extent of distant metastasis: <br> o M0 = no identifiable metastatic disease<br> o M1 = (Stage IV) designates the presence of distant metastasis (brain, bone, liver)
| |
| | |
| [[Image:PT stages.jpg]] <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref>
| |
| | |
| The amount of nerve-root involvement and careful neurological investigation of the arm and shoulder function is also important and very informative <ref name="10">Rusch, Md VW, Management of Pancoast tumours. The Lancet Oncology Nov 27, 2006; 7(12):997–1005.</ref>.<br><br>
| |
| | |
| == Etiology/Causes ==
| |
| | |
| Common risk factors include (similar to lung cancer):
| |
| | |
| Smoking
| |
| | |
| Secondhand smoke
| |
| | |
| Asbestos exposure
| |
| | |
| Exposure to industrial elements like gold or nickel
| |
| | |
| Diesel exhaust<ref name="11">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview</ref><br>
| |
| | |
| [[Image:PT causes.jpg]]<ref name="16">Dartevelle P, Macchiarinib M. Surgical Management of Superior Sulcus Tumors. The Oncologist 1999; 4:398-407.</ref>
| |
|
| |
|
| == Systemic Involvement == | | == Systemic Involvement == |
| | [[File:Pancoast_tumor_spreading.png|alt=|thumb|300x300px|Pancoast tumor spreading]] |
| | Pancoast tumors are often mis-diagnosed or diagnosed too late to prevent metastasis to adjoining structures. This form of lung cancer is very dangerous because of its close proximity to other structures that include<ref name="p4" />: |
|
| |
|
| Pancoast tumors are often mis-diagnosed or diagnosed too late to prevent metastasis to adjoining structures. This form of lung cancer is very dangerous because of its close proximity to other structures that include<ref name="4">Aigner C, Klepetko W. Current treatment concepts of pancoast tumors. European surgery. 2010; 42(5):214-9.</ref>:
| | * '''Brachial plexus'''- this is commonly invaded at the ulnar distribution (C8-T1), thus atrohpy/parasthesia of the ulnar distribution is reported. This is often the patient's primary complaint/presentation to therapy with shoulder pain that radiates down to the 4th and 5th digit.<ref name="p2" /> |
| | * '''Subclavian vessels'''- metastasis to the subclavian artery or adjoining structure may lead to deterioration or compression of blood vessels causing edema.<ref name="p9" /> |
| | * '''Stellate ganglion'''- This is a large ganglion located at the bottom of the cervical spine in connection with the thoracic spine and is related to the sympathetic nervous system. Invasion of this may result in Horner's Syndrome.<ref name="p1" /> |
| | * '''Adjacent vertebral bodies'''- If the tumor is able to metastasize the vertebral bodies, this may lead to permanent paralysis of the affected area.<ref name="p1" /> |
| | == Medical Management == |
| | For many years, Pancoast tumors were considered untreatable. In recent decades, the outlook for people with Pancoast tumors has greatly improved.Treatment for Pancoast tumors involves a combination of [[Chemotherapy Side Effects and Syndromes|chemotherapy]], [[Radiation Side Effects and Syndromes|radiation]], and [[Surgery and General Anaesthetic|surgery]]. Treatment depends on the extent of involvement especially through the apex (these tumours usually involve the brachial plexus and subclavian vessels). In this case, radiotherapy is typically administered in an attempt to reduce the tumour sufficiently to allow for attempted resection. If the tumor has metastasized to areas beyond the chest surgery may not be appropriate.<ref>Healthline [https://www.healthline.com/health/pancoast-tumor#treatment Pancoast tumours] Available:https://www.healthline.com/health/pancoast-tumor#treatment (accessed 24.1.2023)</ref> |
|
| |
|
| '''Brachial plexus'''- this is commonly invaded at the ulnar distribution (C8-T1), thus atrohpy/parasthesia of the ulnar distribution is reported. This is often the patient's primary complaint/presentation to therapy with shoulder pain that radiates down to the 4th and 5th digit.<ref name="2">Archie VC, Thomas Jr. CR. Superior sulcus tumors: a mini-review. The oncologist lung cancer. 2004;9:550-5.</ref>
| | Complete resection is the major factor in determining survival |
|
| |
|
| '''Subclavian vessels'''- metastasis to the subclavian artery or adjoining structure may lead to deterioration or compression of blood vessels causing edema.<ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication.</ref>
| | * complete resection achieved - 45% 5-year survival |
| | * incomplete resection only - 0% 5-year survival<ref name=":0" /> |
|
| |
|
| ''' Stellate ganglion'''- This is a large ganglion located at the bottom of the cervical spine in connection with the thoracic spine and is related to the sympathetic nervous system. Invasion of this may result in Horner's Syndrome.<ref name="11">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview.</ref>
| | == Physical Therapy Management == |
|
| |
|
| '''Adjacent vertebral bodies'''- If the tumor is able to metastasize the vertebral bodies, this may lead to permanent paralysis of the affected area.<ref name="11">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview.</ref>
| | A mutimodal management of the patient is needed. When it comes to pancoast tumors, the primary role of the Physical Therapist is post operative treatment to prevent respiratory complications including atelectasis and pneumonia, and control the patient’s pain levels. The patient is immobilized the first post op day with attention to chest Physiotherapy and bronchoscopic suctioning may be necessary to clear secretions in patients with ineffective cough <ref name="p0" />. |
|
| |
|
| [[Image:Pancoast drawing.jpg|270x300px]] [[Image:Pancoast tumor spreading.png|300x249px]] | | Intensive respiratory care should be implemented and chest expansion measurements should be taken to ensure: <ref name="p6">Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011. CA: A Cancer journal for clinicians. 2011;61:212–36.</ref> |
|
| |
|
| == Medical Management (current best evidence) ==
| | *Adequate ventilation using mechanical support (if necessary) |
| | *Satisfactory chest tube function |
| | *Clearance of secretions by mobilizing, coughing, chest physiotherapy, nasotracheal or orotracheal or bronchoscopic suctioning, or a temporary tracheostomy |
| | *Adequate analgesia |
| | *Increased transpulmonary pressure with incentive spirometry or continuous positive airway pressure mask.<br /> |
| | Avoid fluid overload and use diuretics judiciously to avoid acute respiratory distress. Chest tubes remain in place until all air leaks have stopped, there is complete lung expansion and almost no fluid drainage present <ref name="p6" />. |
|
| |
|
| Complete resection of these tumors is a necessity for long term survival and this is made complicated due to their complexity and involvement of the structures around them that include the brachial plexus, subclavian vessels and the spine. Because of this, a multimodal approach is often needed to ensure removal while minimizing any further complications or recurrences <ref name="13">Aigner C, Klepetko W. Current treatment concepts of Pancoast tumors. European Surgery: ACA Acta Chirurgica Austriaca Oct 2010; 42(5):214-219.</ref>.
| | The role of the Physical Therapist it also depends on the type of surgery approach used. Its focus could be the articular mobilisation of the shoulder complex, the neck and the thoracic spine according to the surgeon. Soft tissue mobilisation around the scar (it can block the normal clavicular or scapular range of motion) can be performed 2-3 weeks after operation. Early mobilisation of the gleno-humeral can prevent secondary shoulder limitation in the ADL as subluxation and adhesive capsulitis <ref name="p8">Petraglia, Md JF. International Pain Medical Group. [homepage on the Internet]. 2008 [cited 2012 Mar 30]. Available from: http://www.gotpaindocs.com/pancsts_tmor_syndrm.htm</ref>. |
|
| |
|
| [[Image:PT stage algorithm.jpg]]<ref name="18">Parissis H, Young V. Treatment of pancoast tumors from the surgeons prospective: re-appraisal of the anteriormanubrial sternal approach. Journal of Cardiothoracic Surgery 5/1/2010; 102(5).</ref><br>
| | Specific scapular mobilisation could be address to the limited range of motion and to the local pain after surgery. To obtain better outomes the passive and active self mobilisation of the thoracic spine and of the cervical spine could be useful in the early stages of rehabilitation. |
|
| |
|
| Initially pancoast tumors were viewed as inoperable and incurable and treatment for them was radiotherapy with a palliative intent. It wasn’t until 1956 when resection with radiotherapy was attempted by Chardack and MacCallum which consisted of an upper lobe lobectomy with en-bloc chest wall and nerve root resection followed by adjuvant chemotherapy. This patient lived for 5 years without recurrence and further trials of induction radiotherapy and en-bloc resection conducted by Shaw & Paulson in 1961, confirmed a 5 year survival rate of 30% with complete resection in about 60% of patients.<ref name="13">Aigner C, Klepetko W. Current treatment concepts of Pancoast tumors. European Surgery: ACA Acta Chirurgica Austriaca Oct 2010; 42(5):214-219.</ref><ref name="10">Rusch, Md VW, Management of Pancoast tumours. The Lancet Oncology Nov 27, 2006; 7(12):997–1005.</ref> Preoperative radiation followed by surgery became the standard of care <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref> for the next 30 years until more and more complications were starting to be seen and other surgical techniques began developing in the late 80s and early 90s to addressed tumors invading the spine and the subclavian vessels. The first was the anterior (Anterior transclavicular approach) approach developed by Dartevelle which was later modified by Grunenwald who developed an anterior clavicular sparring approach (hemi-clamshell incision with supraclavicular extension). Its purpose was to optimize exposure by providing direct visualization of vascular structures, brachial plexus, sympathetic chain and stellate ganglion <ref name="15">Barbetakis N,, Pancoast Tumors: Surgical Approaches and Techniques. Topics in Thoracic Surgery 2012; :273-284.</ref>. This became very popular yet 5 year survival rates still remained around 30% and local recurrence was observed in 40% of all operated patients. The posterior approach was later developed by Shaw-Paulson to target tumors situated in the posterior superior sulcus that did not invade the anterior structures of the thoracic inlet but may invade the vertebral bodies or the brachial plexus (C8 and T1 nerve roots are most common).<ref name="15">Barbetakis N,, Pancoast Tumors: Surgical Approaches and Techniques. Topics in Thoracic Surgery 2012; :273-284.</ref><ref name="13">Aigner C, Klepetko W. Current treatment concepts of Pancoast tumors. European Surgery: ACA Acta Chirurgica Austriaca Oct 2010; 42(5):214-219.</ref>
| | The muscular strengthening of the arm and of the shoulder girdle can be performed in the early stages of rehabilitation. At the beginning isometric contraction could be useful to avoid excessive pain caused by repetitive active mobilisation. The simultaneous respiratory and surgical complication must be assessed before starting the strenghtening program. |
| | [[File:ULTT.png|thumb|Ulnar nerve self mobilisation]] |
| | Pancoast tumors with brachial plexus involvement use to underwent to neurosurgical nerve resection of C8-T1 roots. The tumor resection and the neurolysis could both outcome in a significant loss of hand function in many patients. In those cases the PT could prevent the muscluar retraction of hand and wrist with splints or orthesis. Exercises address to mobility and strenght can improve the quality of life and the arm and shoulder function. |
|
| |
|
| '''Anterior transclavicular (Dartevelle) ''' <ref name="15">Barbetakis N, Pancoast Tumors: Surgical Approaches and Techniques. Topics in Thoracic Surgery 2012; :273-284.</ref> '''Anterior approach (Grunenwald approach) '''<ref name="18">Parissis H, Young V. Treatment of pancoast tumors from the surgeons prospective: re-appraisal of the anteriormanubrial sternal approach. Journal of Cardiothoracic Surgery 5/1/2010; 102(5).</ref><br>
| | The use of the [[Upper Limb Tension Tests (ULTTs)|Upper Limb Tension Test 3 (ULTT3)]] as a neurodynamic slider mobilisation could be a good exercise in the first stages of rehabilitation. The passive neurodynamic mobilisation could be address to make feel the patient comfortable in the positione: then self ulnar nerve mobilisation in contribution to a specific home exercise program could improve range of motion both acting on the mechanosensitivity of the nerve and on the articular active movements of scapula and gleno-humeral. In that cases in which the abduction of the shoulder is limited some variation could be performed. |
|
| |
|
| [[Image:PT ant 1.jpg|182x157px]] [[Image:PT ant 3.jpg|228x163px]] [[Image:PT ant resection.png|191x230px]]<br> | | [[Low Level Laser Therapy|Laser]] therapy in combination with and individualized wellness program is also effective in treating this condition and can improve the patients overall health and wellbeing. <ref name="p8" /> [[Therapeutic Ultrasound|Ultrasound]] therapy could be locally contraindicated in those patient who risk bones or pulmunar metastasis. |
| | |
| <ref name="15">Barbetakis N, Pancoast Tumors: Surgical Approaches and Techniques. Topics in Thoracic Surgery 2012; :273-284.</ref> '''Posterior approach (Paulson)''' <ref name="16">Dartevelle P, Macchiarinib M. Surgical Management of Superior Sulcus Tumors. The Oncologist 1999; 4:398-407.</ref> <ref name="10">Rusch, Md VW, Management of Pancoast tumours. The Lancet Oncology Nov 27, 2006; 7(12):997–1005.</ref><br>
| |
| | |
| [[Image:PT post 1.jpg|229x159px]][[Image:PT post 3.jpg|215x128px]][[Image:PT post 2.jpg|150x216px]]
| |
| | |
| <br> The multimodal treatment approach (chemoradiation followed by surgical resection) became the standard during this time and resulted in much improved outcomes as can be seen by the studies listed below <ref name="13">Aigner C, Klepetko W. Current treatment concepts of Pancoast tumors. European Surgery: ACA Acta Chirurgica Austriaca Oct 2010; 42(5):214-219.</ref>. However, due to poor performance status and advanced tumor stages, only 30-40% of patients are eligible for multimodal treatment. <ref name="18">Parissis H, Young V. Treatment of pancoast tumors from the surgeons prospective: re-appraisal of the anteriormanubrial sternal approach. Journal of Cardiothoracic Surgery 5/1/2010; 102(5).</ref><br>
| |
| | |
| [[Image:PT multimodal chart.jpg]]<ref name="13">Aigner C, Klepetko W. Current treatment concepts of Pancoast tumors. European Surgery: ACA Acta Chirurgica Austriaca Oct 2010; 42(5):214-219.</ref><br>
| |
| | |
| <br>
| |
| | |
| Other surgical approaches include…<br>
| |
| | |
| <br>
| |
| | |
| '''Hemiclamshell or Trapdoor Incision ''' <ref name="16">Dartevelle P, Macchiarinib M. Surgical Management of Superior Sulcus Tumors. The Oncologist 1999; 4:398-407.</ref> '''Masoaka Incision'''<br>
| |
| | |
| [[Image:Hemiclamshell or Trapdoor Incision.jpg]][[Image:Masoaka Incision.jpg|266x297px]]<br>
| |
| | |
| <br>
| |
| | |
| '''Surgical limitations:''' Neural, vascular, vertebral body and lymph node invasion <ref name="16">Dartevelle P, Macchiarinib M. Surgical Management of Superior Sulcus Tumors. The Oncologist 1999; 4:398-407.</ref><br>
| |
| | |
| [[Image:Subclavian Art invasion.jpg]]<ref name="13">Aigner C, Klepetko W. Current treatment concepts of Pancoast tumors. European Surgery: ACA Acta Chirurgica Austriaca Oct 2010; 42(5):214-219.</ref><br>
| |
| | |
| '''Contraindications to surgery:''' presence of extra-thoracic sites of metastasis, histologically confirmed N2 disease, extensive invasion of the cervical trachea, esophagus and the brachial plexus above the C7 nerve root (indicates that the tumor is locally too extensive to achieve a complete resection or that limb amputation is necessary), massive vertebral invasion that’s diagnosed preoperatively. <ref name="16">Dartevelle P, Macchiarinib M. Surgical Management of Superior Sulcus Tumors. The Oncologist 1999; 4:398-407.</ref><br>
| |
| | |
| <br>
| |
| | |
| '''Surgical complications: '''Spinal fluid leakage, Horner’s syndrome and nerve deficits, Hemothorax, Chylothorax & Prolonged ventilator support <ref name="16">Dartevelle P, Macchiarinib M. Surgical Management of Superior Sulcus Tumors. The Oncologist 1999; 4:398-407.</ref>
| |
| | |
| <br>
| |
| | |
| '''Prognosis Factors:'''
| |
| | |
| [[Image:Px factors.jpg]]<ref name="16">Dartevelle P, Macchiarinib M. Surgical Management of Superior Sulcus Tumors. The Oncologist 1999; 4:398-407.</ref>
| |
| | |
| <br> The current treatment of choice is complete removal of the tumor by en bloc chest wall resection combined with lobectomy and node staging and it may include resection of the paravertebral sympathetic chain, stellate ganglion, lower trunks of the brachial plexus, subclavian artery, or portions of the thoracic vertebrae depending on its involvement. Radiation and chemotherapy can address individual adverse findings and for local and systemic control and induction chemoradiotherapy is used with potentially resectable tumors and surgery is undertaken 2-4 weeks after radiation therapy. A combined thoracic-nonsurgical approach is used for tumors invading the brachial plexus and/or the spine. <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref><br>
| |
| | |
| <br>'''Brachial Plexus block:''' Used in combination with local anesthetics and steroids as an adjunct to drug treatment for rapid relief of pain or to control breakthrough pain <ref name="8">Petraglia, Md JF. International Pain Medical Group. [homepage on the Internet]. 2008 [cited 2012 Mar 30]. Available from: http://www.gotpaindocs.com/pancsts_tmor_syndrm.htm</ref>. A study don’t by Peláez and colleagues purpose that in aggressive tumors compressing the brachial plexus that do not respond to conventional treatment or regional anaesthesia, utilizing the addition of a paravertebral nerve block to the plexus could substantially reduce the patients pain without impacting longevity <ref name="20">Peláez R, Pascual G, Aguilar J, Atanassoff P. Paravertebral Cervical Nerve Block in a Patient Suffering from a Pancoast Tumor. Pain Medicine [serial online]. December 2010;11(12):1799-1802.</ref>. This is also supported in a study by Vranken and colleagues who purposed a reversible, non destructive, continuous nerve blocking technique involving administration of local antsthetics through an axillary cathter into the brachial plexus. This resulted in a significant decrease in the patients visual analog pain score and an increase in performance skills and QOL without any side effects in 4 patients <ref name="22">Vranken J, Zuurmond W, de Lange J. Continuous brachial plexus block as treatment for the Pancoast syndrome. The Clinical Journal Of Pain [serial online]. December 2000;16(4):327-333.</ref>.
| |
| | |
| <br>'''Radiofrequency Destruction of the Brachial Plexus:''' Last resort treatment involving destruction of the brachial plexus via a radiofrequency lesion under biplanar fluoroscopic guidance. <ref name="8">Petraglia, Md JF. International Pain Medical Group. [homepage on the Internet]. 2008 [cited 2012 Mar 30]. Available from: http://www.gotpaindocs.com/pancsts_tmor_syndrm.htm</ref>
| |
| | |
| <br>'''Dorsal Root Entry Zone Lesioning (DREZ):''' Major neurosurgical procedure used as a last resort when all other branchial plexopathy treatments have failed <ref name="8">Petraglia, Md JF. International Pain Medical Group. [homepage on the Internet]. 2008 [cited 2012 Mar 30]. Available from: http://www.gotpaindocs.com/pancsts_tmor_syndrm.htm</ref><br>
| |
| | |
| <br>
| |
| | |
| ''' '''<u>'''Pharmacological management:'''</u>
| |
| | |
| Pharmacotherapy goals are to induce remission, reduce morbidity, and prevent complications <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref><br>
| |
| | |
| <br>
| |
| | |
| '''Opioid Analgesics:''' Primary treatment of pain that can be combined with NSAIDs and may be a short-acting potent opioid such as oxycodone or an immediate-release morphine or methadone <ref name="8">Petraglia, Md JF. International Pain Medical Group. [homepage on the Internet]. 2008 [cited 2012 Mar 30]. Available from: http://www.gotpaindocs.com/pancsts_tmor_syndrm.htm</ref>.
| |
| | |
| <br>'''Antineoplastic agents''': Inhibit cell growth and proliferation and are used in a variety of different cancers including head, neck, breast, testicular and ovarian cancer <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref>.
| |
| | |
| <br>'''Cisplatin (Platinol):''' Alkylating agent causing intrastrand and interstrand cross-linking of DNA that leads to strand breakage. It has a broad range of antitumor activity and forms backbone of currently available approved combination chemotherapy regimens that cause Pancoast syndrome. Its administered via IV in isotonic sodium chloride solution (0.9%) or sodium chloride and glucose. Adequate hydration must be maintained up to 24 hours after a dose and Renal, hematological, auditory, and neurological function must be monitored <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref>.
| |
| | |
| <br>'''Etoposide (Toposar, VePesid)''': Semisynthetic derivative of podophyllotoxin with antineoplastic properties interferes with topoisomerase II function thus inhibiting DNA synthesis <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref>.<br><br>
| |
| | |
| == Physical Therapy Management (current best evidence) ==
| |
| | |
| When it comes to pancoast tumors, the primary role of the Physical Therapist is post operative treatment to prevent respiratory complications including atelectasis and pneumonia, and control the patient’s pain levels. The patient is immobilized the first post op day with attention to chest Physiotherapy and bronchoscopic suctioning may be necessary to clear secretions in patients with ineffective cough <ref name="30">Slinger PD, &amp;amp;amp;amp;amp;amp;amp; Principles and Practice of Anesthesia for Thoracic Surgery. New York: Springer Science+Business media LLC; 2011.</ref>. Intensive respiratory care should be implemented and chest expansion measurements should be taken to ensure... <ref name="16">Dartevelle P, Macchiarinib M. Surgical Management of Superior Sulcus Tumors. The Oncologist 1999; 4:398-407.</ref>
| |
| | |
| o Adequate ventilation using mechanical support (if necessary)<br> o Satisfactory chest tube function <br> o Clearance of secretions by mobilizing, coughing, chest physiotherapy, nasotracheal or orotracheal or bronchoscopic suctioning, or a temporary tracheostomy<br> o Adequate analgesia <br> o Increased transpulmonary pressure with incentive spirometry or continuous positive airway pressure mask.<br>
| |
| | |
| <br>
| |
| | |
| Avoid fluid overload and use diuretics judiciously to avoid acute respiratory distress. Chest tubes remain in place until all air leaks have stopped, there is complete lung expansion and almost no fluid drainage present <ref name="16">Dartevelle P, Macchiarinib M. Surgical Management of Superior Sulcus Tumors. The Oncologist 1999; 4:398-407.</ref>. <br>
| |
| | |
| Other roles of the PT are to maintain function and ADLs and search for and treat shoulder issues that include subluxation and adhesive capsulitis <ref name="8">Petraglia, Md JF. International Pain Medical Group. [homepage on the Internet]. 2008 [cited 2012 Mar 30]. Available from: http://www.gotpaindocs.com/pancsts_tmor_syndrm.htm</ref>. Laser therapy in combination with and individualized wellness program is also effective in treating this condition and can improve the patients overall health and wellbeing. <ref name="8">Petraglia, Md JF. International Pain Medical Group. [homepage on the Internet]. 2008 [cited 2012 Mar 30]. Available from: http://www.gotpaindocs.com/pancsts_tmor_syndrm.htm</ref><br><br>
| |
| | |
| == Alternative/Holistic Management (current best evidence) ==
| |
| | |
| Alternative treatment options offered by the Cancer Treatment Centers of America (CTCA): <ref>Hamrick C, Schaner K. Cancer Treatment Centers of America. [homepage on the Internet]. 2010 [cited 2012 Apr 3]. Available from: http://www.cancercenter.com/complementary-alternative-medicine.cfm?source=GOOGLESE&channel=paid%20search&c=paid%20search:Google:Google%20-%20Southeastern%20Core%20Terms:General%3A+Cancer+Treatments%7CHolistic:holistic+cancer+treatment:Broad&OVMTC=Broad&site=&creative=4340713311&OVKEY=holistic%20cancer%20treatment&url_id=129219185&adpos=1t1&gclid=CI3s67uTmq8CFcjb4AodtWnWaQ</ref>
| |
| | |
| Nutrition Therapy to keep you strong and nutritionally balanced so your cancer treatment is not interrupted<br>
| |
| | |
| Mind-Body Medicine to reduce stress and improve quality of life
| |
| | |
| Naturopathic Medicine to support your health and conventional cancer treatment while minimizing the risk of side effects during treatment
| |
| | |
| Oncology Rehabilitation to build strength and endurance, regain independence, reduce stress, and maintain the energy you need to participate in activities that are important to you throughout your cancer treatment.
| |
| | |
| Spiritual Support to strengthen your spirituality to combat cancer
| |
| | |
| Acupuncture to alleviate treatment-related side effects, such as nausea and vomiting, pain, and other common symptoms like stress.
| |
| | |
| Chiropractic Care to help deal with pain and discomfort, reduce stress and increase mobility, flexibility, strength, and function, as well as help improve quality of life and overall well-being.
| |
| | |
| Image Enhancement to look and feel your best in effect reducing stress and improving quality of life. <br>
| |
|
| |
|
| == Differential Diagnosis == | | == Differential Diagnosis == |
|
| |
|
| Lung Cancer; Non-Small Cell or Oat Cell (Small Cell) <ref name="9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref> | | Lung Cancer; Non-Small Cell or Oat Cell (Small Cell) <ref name="p9">D'silva KJ. Medscape: Pancoast syndrome, [homepage on the Internet]. Aug 15, 2011 [cited 2012 Mar 30]. Available from: http://emedicine.medscape.com/article/284011-medication</ref><br>[[Thoracic Outlet Syndrome (TOS)|Thoracic Outlet syndrome]]<br>Pulmonary echinococcosis <ref name="p5">Kim P, Hains F, Wallace M, Mior S. Pancoast tumour: a case report. Journal Of The Canadian Chiropractic Association [serial on the Internet]. (1993, Dec), [cited April 4, 2012]; 37(4): 214. Available from: Health Source: Nursing/Academic Edition.</ref><br>Pulmonary leiomyosarcoma <ref>Shoji F, Yoshino I, Takeshita M, Sumiyoshi S, Sueishi K, Maehara Y. Pulmonary leiomyosarcoma presenting as a pancoast tumor. Pathology - Research & Practice [serial online]. October 18, 2007;203(10):745-748.</ref><br>[[Cervical Radiculopathy|C8-T1 radiculopathy]] <ref name="p7">Abdul Khader S, Kumar A. Pancoast tumor presenting as shoulder pain and C8-T1 radiculopathy: a case report. (Poster Session). Archives Of Physical Medicine & Rehabilitation [serial online]. November 2002;83(11):1663.</ref><br>Primary [[Ewing's Sarcoma|Ewing's sarcoma]] <ref name="p9" /> |
| | |
| <br>Thoracic Outlet syndrome | |
| | |
| <br>Pulmonary echinococcosis <ref name="25">Karamustafaoglu Y, Yoruk Y, Mamedov R, Yavasman I. Pulmonary echinococcosis mimicking Pancoast tumor. The Journal Of Thoracic And Cardiovascular Surgery [serial online]. April 2010;139(4):e57-e58.</ref> | |
| | |
| <br>Pulmonary leiomyosarcoma <ref name="26">Shoji F, Yoshino I, Takeshita M, Sumiyoshi S, Sueishi K, Maehara Y. Pulmonary leiomyosarcoma presenting as a pancoast tumor. Pathology - Research &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Practice [serial online]. October 18, 2007;203(10):745-748.</ref> | |
| | |
| <br>C8-T1 radiculopathy <ref name="27">Abdul Khader S, Kumar A. Pancoast tumor presenting as shoulder pain and C8-T1 radiculopathy: a case report. (Poster Session). Archives Of Physical Medicine &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Rehabilitation [serial online]. November 2002;83(11):1663.</ref> | |
| | |
| <br>Primary Ewing's sarcoma <ref name="29">Lowie V. Primary Ewing's sarcoma presenting as a Pancoast tumour. Thorax [serial online]. January 2011;66(1):89-90.</ref><br><br> | |
| | |
| "In all patients it is crucial to obtain histological proof before initiating treatment since not only NSCLC can present as on apical mass but also tumors of other origin such as metastases, sarcomas, lymphomas, tuberculosis or even echinococcus can present with similar clinical and radiological features."<ref name="4">Aigner C, Klepetko W. Current treatment concepts of pancoast tumors. European surgery. 2010; 42(5):214-9.</ref>
| |
| | |
| <br>
| |
| | |
| Cushing Syndrome<ref name="8">Shabir Bhimji, Md, May SK. Emedicinehealth: Pancoast tumor. [homepage on the Internet]. April 2, 2011 [cited 2012 Mar 30]. Available from: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm#Pancoast%20Tumor%20Overview.</ref>
| |
| | |
| <br>
| |
|
| |
|
| "Paraneoplastic syndromes are rare disorders that are triggered by an altered immune system response to a neoplasm. They are defined as clinical syndromes involving nonmetastatic systemic effects that accompany malignant disease."<ref>Santacroce L, Diomede L, Gagliardi S, Balducci L. Medscape: Paraneoplastic Syndromes. [Homepage on the Internet]. Feb 21, 2010 [cited 2012 April 3]. Available at: http://emedicine.medscape.com/article/280744-overview.</ref><br>
| | [[Cushing's Syndrome|Cushing Syndrome]]<ref name="p8" /><br> |
|
| |
|
| == Case Reports/ Case Studies == | | == Case Reports/ Case Studies == |
|
| |
|
| [http://www.mendeley.com/research/paravertebral-cervical-nerve-block-patient-suffering-pancoast-tumor/ Paravertebral Cervical Nerve Block in a Patient Suffering from a Pancoast Tumor]<br> | | [http://www.mendeley.com/research/paravertebral-cervical-nerve-block-patient-suffering-pancoast-tumor/ Paravertebral Cervical Nerve Block in a Patient Suffering from a Pancoast Tumor] |
|
| |
|
| [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2485088/pdf/jcca00044-0024.pdf Pancoast Tumour: a case report][http://web.ebscohost.com.libproxy.bellarmine.edu/ehost/pdfviewer/pdfviewer?vid=6&hid=9&sid=bd345b3b-c661-4517-913a-6766b51aeb6f%40sessionmgr14 <br>] | | [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2485088/pdf/jcca00044-0024.pdf Pancoast Tumour: a case report] |
|
| |
|
| [http://content.karger.com/ProdukteDB/produkte.asp?Aktion=ShowPDF&ArtikelNr=29516&Ausgabe=226560&ProduktNr=224278&filename=29516.pdf Severe Pancoast Tumour] | | [http://content.karger.com/ProdukteDB/produkte.asp?Aktion=ShowPDF&ArtikelNr=29516&Ausgabe=226560&ProduktNr=224278&filename=29516.pdf Severe Pancoast Tumour] |
|
| |
|
| [http://www.ncbi.nlm.nih.gov/pubmed/18503622 Alleviation of Pancoast tumor by Ultrasound-guided Percutaneous Ablation of Cervical Nerve Roots]<br> | | [http://www.ncbi.nlm.nih.gov/pubmed/18503622 Alleviation of Pancoast tumor by Ultrasound-guided Percutaneous Ablation of Cervical Nerve Roots] |
| | |
| [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2484347/pdf/jcca00076-0039.pdf Superior Pulmonary Sulcus Tumor]
| |
| | |
| == Resources <br> ==
| |
| | |
| Medscape: http://emedicine.medscape.com/article/284011-overview<br>
| |
| | |
| Cancer Treatment Centers of America (CTCA): http://www.cancercenter.com/?OVMTC=Phrase&site=&creative=1144020265&OVKEY=cancer%20treatments%20of%20america&url_id=144968219&adpos=1t1&gclid=CIKGr7CNm68CFYNo4AodeCYUdg
| |
| | |
| emedicinehealth: http://www.emedicinehealth.com/pancoast_tumor/article_em.htm<br>
| |
| | |
| Medscape: Paraneoplastic Syndromes. http://emedicine.medscape.com/article/280744-overview.<br>
| |
| | |
| About.com: Lung Cancer http://lungcancer.about.com/od/typesoflungcancer/f/pancoasttumor.htm<br>
| |
| | |
| == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) ==
| |
| | |
| see tutorial on [[Adding PubMed Feed|Adding PubMed Feed]]
| |
|
| |
|
| <br>
| | [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2484347/pdf/jcca00076-0039.pdf Superior Pulmonary Sulcus Tumor] |
| <div class="researchbox"><rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1R9m212NERpwMq0S8rdihhGUcgjNry_6S-Aru_0DFFuJA0aApO|charset=UTF-8|short|max=10</rss></div>
| |
|
| |
|
| == References == | | == References == |
|
| |
|
| <references /> | | <references /> |
|
| |
|
| <br><br>
| | [[Category:Oncology]] |
| | [[Category:Medical]] |
| | [[Category:Bellarmine_Student_Project]] |
| | [[Category:Cardiopulmonary]] |
| | [[Category:Conditions]] |
| | [[Category:Chronic Respiratory Disease - Conditions]] |