Osteophyte: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (17 intermediate revisions by 3 users not shown) | |||
| Line 2: | Line 2: | ||
'''Original Editor '''- [[User:Lucinda hampton|Lucinda hampton]] | '''Original Editor '''- [[User:Lucinda hampton|Lucinda hampton]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' -{{Special:Contributors/{{FULLPAGENAME}}}}<span style="line-height: 1.5em;"> </span> | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Osteophytes are cartilage-capped bony proliferations (bony spurs) that most commonly develop at the margins of a synovial joint as a response to articular cartilage damage, as seen very commonly in osteoarthritis (OA).<ref name=":1">Radiopedia [https://radiopaedia.org/articles/osteophyte-2 Osteophyte] Available:https://radiopaedia.org/articles/osteophyte-2 (accessed 7.9.2022)</ref> | Osteophytes are [[cartilage]]-capped bony proliferations (bony spurs) that most commonly develop at the margins of a [[Synovial Joints|synovial joint]] as a response to articular cartilage damage, as seen very commonly in [[osteoarthritis]] (OA).<ref name=":1">Radiopedia [https://radiopaedia.org/articles/osteophyte-2 Osteophyte] Available:https://radiopaedia.org/articles/osteophyte-2 (accessed 7.9.2022)</ref> | ||
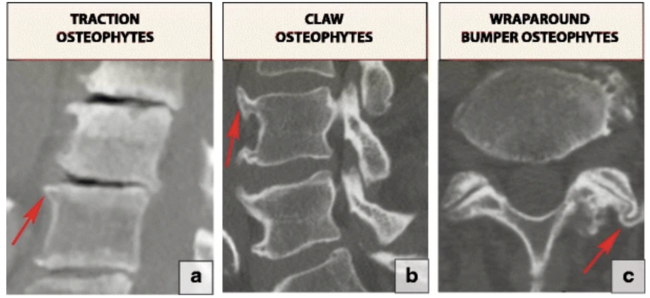
[[File:Osteophytes.png|center|thumb|650x650px|Three types of osteophytes related to the degenerative spine: (a) traction osteophytes (arrow), (b) claw osteophytes (arrow) and (c) wraparound bumper osteophytes (arrow)]] | |||
== Pathophysiology == | == Pathophysiology == | ||
Osteophytes are formed of fibrocartilage and bone, often forming at the peripheral margins of joints at the interface between cartilage and the periosteum. Osteophytes are thought to develop from chondrogenic differentiation of progenitor cells, commonly from within the periosteum. Osteophytes appear to be a cellular repair response to the altered growth factor environment following joint injury. In some cases osteophytes can contribute to the stability of the joints.<ref>Firestein GS, Budd RC, Gabriel SE, McInnes IB, O'Dell JR. Kelley's Textbook of Rheumatology E-Book. Elsevier Health Sciences; 2012 Aug 31. Available:https://www.sciencedirect.com/topics/medicine-and-dentistry/osteophyte (accessed 7.9.2022)</ref> | Osteophytes are formed of fibrocartilage and [[bone]], often forming at the peripheral margins of joints at the interface between cartilage and the periosteum. Osteophytes are thought to develop from chondrogenic differentiation of progenitor cells, commonly from within the periosteum. Osteophytes appear to be a cellular repair response to the altered [[Growth Factors|growth factor]] environment following joint injury. In some cases osteophytes can contribute to the stability of the joints.<ref>Firestein GS, Budd RC, Gabriel SE, McInnes IB, O'Dell JR. Kelley's Textbook of Rheumatology E-Book. Elsevier Health Sciences; 2012 Aug 31. Available:https://www.sciencedirect.com/topics/medicine-and-dentistry/osteophyte (accessed 7.9.2022)</ref> | ||
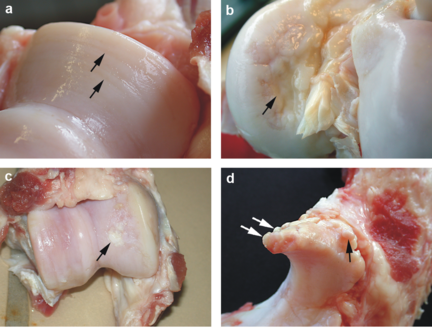
[[File:Damaged cartilage Danish sow.png|center|thumb|432x432px|a. Cartilage erosion (arrows) b: Cartilage ulceration (arrow) c: Cartilage repair (arrow) d: Marginal osteophytes (arrows)]] | [[File:Damaged cartilage Danish sow.png|center|thumb|432x432px|a. Cartilage erosion (arrows) b: Cartilage ulceration (arrow) c: Cartilage repair (arrow) d: Marginal osteophytes (arrows)]] | ||
== Presentation == | == Presentation == | ||
Osteophytes are most commonly found in the following areas. Neck, shoulder, knee, lower back, fingers or big toe, foot or heel. Osteophytes cause problems for example if they: cause friction if rubbing against footwear; impinge nerves such as an existing spinal root; restrict movement as may occur in hip and knee OA | Osteophytes are most commonly found in the following areas. Neck, shoulder, knee, lower back, fingers or big toe, foot or heel. Osteophytes cause problems for example if they: cause friction if rubbing against footwear; impinge nerves such as an existing spinal root; restrict movement as may occur in hip and knee OA.<ref name=":0">NHS [https://www.nhs.uk/conditions/osteophyte/ Osteophyte] Available:https://www.nhs.uk/conditions/osteophyte/ (accessed 7.9.2022)</ref> Following are the pages of conditions where osteophytes are present: | ||
* [[Hallux Rigidus]] | |||
* [[Anterior Ankle Impingement Syndrome]] | |||
* [[Osteoarthritis]] of knee | |||
* [[Uncovertebral Joints]] | |||
* [[Lumbar Spinal Stenosis]] | |||
* Vertebral osteophytes are a characteristic of [[Degenerative Disc Disease|disc degeneration]]. <ref>Czervionke LF, Fenton DS. Imaging Painful Spine Disorders E-Book. Elsevier Health Sciences; 2011 Apr 28.Available:https://www.sciencedirect.com/topics/medicine-and-dentistry/osteophyte (accessed 8.9.2022)</ref> | |||
* [[Cervical Osteoarthritis]] | |||
* [[Lumbar Spondylosis]] | |||
* [[Hip Osteoarthritis]] | |||
* [[Ankle Osteoarthritis|Ankle osteoarthritis]] | |||
== Treatment == | == Treatment == | ||
Osteophytes when causing issues, for example with OA, can be managed along side management of OA, See link here [[Osteoarthritis]]. | Osteophytes when causing issues, for example with OA, can be managed along side management of OA, See link here [[Osteoarthritis|Osteoarthritis.]] They are not managed specifically. | ||
Removal of an osteophyte is not usual, unless it's irritating a nerve in the spine or restricting a joint's range of movement. If surgery is warranted, a surgeon will explain the procedure's risks and benefits.<ref name=":0" /> | Removal of an osteophyte is not usual, unless it's irritating a nerve in the spine or restricting a joint's range of movement. If surgery is warranted, a surgeon will explain the procedure's risks and benefits.<ref name=":0" /> | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
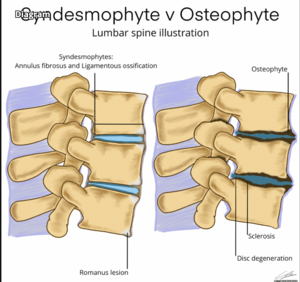
Enthesophyte: located at an attachment of a ligament or tendon, not associated with a joint.<ref name=":1" /> | # [[File:Dx osteophyte.png|right|frameless]]Syndesmophyte: Thin, vertically oriented ossification of annular ligament (Sharpey fibers) from [[Ankylosing Spondylitis (Axial Spondyloarthritis)|ankylosing spondylitis]]<ref>Blankenbaker DG, Davis KW. ExpertDDx: Musculoskeletal E-Book. Elsevier Health Sciences; 2017 Oct 13.Available: https://www.sciencedirect.com/topics/medicine-and-dentistry/osteophyte<nowiki/>(accessed 8.9.2022)</ref> | ||
# Enthesophyte: located at an attachment of a [[ligament]], [[fascia]] or [[Tendon Anatomy|tendon]], not associated with a joint.<ref name=":1" /> | |||
# It is difficult to tell the difference between an osteophyte and [[Disc Herniation|disc herniation]] solely by [[MRI Scans|MRI]]. [[CT Scans|CT]] is a helpful adjunct; however, often central canal and foraminal narrowing are caused by a combination of a disc herniation and osteophyte. | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Osteoarthritis]] | |||
[[Category:Bone - Conditions]] | |||
[[Category:Physiology]] | |||
[[Category:Anatomy]] | |||
Latest revision as of 21:16, 9 January 2024
Original Editor - Lucinda hampton
Top Contributors -Lucinda hampton, Nupur Smit Shah and Kim Jackson
Introduction[edit | edit source]
Osteophytes are cartilage-capped bony proliferations (bony spurs) that most commonly develop at the margins of a synovial joint as a response to articular cartilage damage, as seen very commonly in osteoarthritis (OA).[1]
Pathophysiology[edit | edit source]
Osteophytes are formed of fibrocartilage and bone, often forming at the peripheral margins of joints at the interface between cartilage and the periosteum. Osteophytes are thought to develop from chondrogenic differentiation of progenitor cells, commonly from within the periosteum. Osteophytes appear to be a cellular repair response to the altered growth factor environment following joint injury. In some cases osteophytes can contribute to the stability of the joints.[2]
Presentation[edit | edit source]
Osteophytes are most commonly found in the following areas. Neck, shoulder, knee, lower back, fingers or big toe, foot or heel. Osteophytes cause problems for example if they: cause friction if rubbing against footwear; impinge nerves such as an existing spinal root; restrict movement as may occur in hip and knee OA.[3] Following are the pages of conditions where osteophytes are present:
- Hallux Rigidus
- Anterior Ankle Impingement Syndrome
- Osteoarthritis of knee
- Uncovertebral Joints
- Lumbar Spinal Stenosis
- Vertebral osteophytes are a characteristic of disc degeneration. [4]
- Cervical Osteoarthritis
- Lumbar Spondylosis
- Hip Osteoarthritis
- Ankle osteoarthritis
Treatment[edit | edit source]
Osteophytes when causing issues, for example with OA, can be managed along side management of OA, See link here Osteoarthritis. They are not managed specifically.
Removal of an osteophyte is not usual, unless it's irritating a nerve in the spine or restricting a joint's range of movement. If surgery is warranted, a surgeon will explain the procedure's risks and benefits.[3]
Differential Diagnosis[edit | edit source]
- Syndesmophyte: Thin, vertically oriented ossification of annular ligament (Sharpey fibers) from ankylosing spondylitis[5]
- Enthesophyte: located at an attachment of a ligament, fascia or tendon, not associated with a joint.[1]
- It is difficult to tell the difference between an osteophyte and disc herniation solely by MRI. CT is a helpful adjunct; however, often central canal and foraminal narrowing are caused by a combination of a disc herniation and osteophyte.
References[edit | edit source]
- ↑ 1.0 1.1 Radiopedia Osteophyte Available:https://radiopaedia.org/articles/osteophyte-2 (accessed 7.9.2022)
- ↑ Firestein GS, Budd RC, Gabriel SE, McInnes IB, O'Dell JR. Kelley's Textbook of Rheumatology E-Book. Elsevier Health Sciences; 2012 Aug 31. Available:https://www.sciencedirect.com/topics/medicine-and-dentistry/osteophyte (accessed 7.9.2022)
- ↑ 3.0 3.1 NHS Osteophyte Available:https://www.nhs.uk/conditions/osteophyte/ (accessed 7.9.2022)
- ↑ Czervionke LF, Fenton DS. Imaging Painful Spine Disorders E-Book. Elsevier Health Sciences; 2011 Apr 28.Available:https://www.sciencedirect.com/topics/medicine-and-dentistry/osteophyte (accessed 8.9.2022)
- ↑ Blankenbaker DG, Davis KW. ExpertDDx: Musculoskeletal E-Book. Elsevier Health Sciences; 2017 Oct 13.Available: https://www.sciencedirect.com/topics/medicine-and-dentistry/osteophyte(accessed 8.9.2022)