Malaria: Difference between revisions
m (Text replace - '- Your name will be added here if you are a lead editor on this page.' to ' ') |
No edit summary |
||
| (15 intermediate revisions by 8 users not shown) | |||
| Line 2: | Line 2: | ||
'''Original Editors '''- [[User:Aaron Hume|Aaron Hume]] from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | '''Original Editors '''- [[User:Aaron Hume|Aaron Hume]] from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
[[File:Mosquito3.jpg|right|frameless]] | |||
Malaria is caused by ''Plasmodium'' parasites. The parasites are spread to people through the bites of infected female ''Anopheles'' mosquitoes, called "malaria vectors." There are 5 parasite species that cause malaria in humans, and 2 of these species – ''P. falciparum'' and ''P. vivax'' – pose the greatest threat. | |||
* Malaria is a life-threatening disease. | |||
* It is preventable and curable. | |||
* In 2018, there were an estimated 228 million cases of malaria worldwide.<ref name=":0">WHO Malaria Available from:https://www.who.int/news-room/fact-sheets/detail/malaria (last accessed 14.11.2020)</ref> | |||
== Etiology == | |||
[[File:Cycle2.gif|right|frameless|400x400px]] | |||
[[ | Five ''Plasmodium'' species possess the ability to infect humans: ''P. falciparum, P. ovale, P. vivax, P. malariae'', and ''P. knowlesi''.<ref name=":1" /><ref>Picture courtesy of http://qspace.library.queensu.ca/dspace/html/1974/421/pfalcip01.htm</ref> | ||
* Transmission can also occur by way of blood transfusion, organ transplant, the sharing of needles with contaminated blood, or by congenital means when a mother passes the infection to her unborn baby. Furthermore, “Airport” Malaria can occur when infected mosquitos are transported from a Malarious region to an area not affected by Malaria. Subsequently, civilians of the non-endemic region can be infected by Malaria without having travelled to a foreign country.<ref name="M">Malaria. Centers for Disease Control and Prevention Web Site. http://www.CDC.gov/malaria. Updated June, 2009. Accessed March 1st, 2010.</ref> | |||
* Once the parasites are inside your body, they travel to the [[Liver Disease|liver]], where they mature. After several days, the mature parasites enter the bloodstream and begin to infect red [[Blood Physiology|blood]] cells. | |||
* Within 48 to 72 hours, the parasites inside the red blood cells multiply, causing the infected cells to burst open. | |||
* The parasites continue to infect red blood cells, resulting in symptoms that occur in cycles that last two to three days at a time<ref>Healthline [https://www.healthline.com/health/malaria Malaria] Available from:https://www.healthline.com/health/malaria (last accessed 14.11.2020)</ref>. | |||
The below video describes the the sequence of events causing an infection by a Malarial parasite and also describes how the infection can spread throughout the body<br>{{#ev:youtube|qvlTOhCmxvY}}<ref>You Tube. HHMI -- Life Cycle of Malaria Parasite in Human Host.http://www.youtube.com/watch?v=qvlTOhCmxvY. Accessed Feb 12th, 2019.</ref> | |||
== Epidemiology == | |||
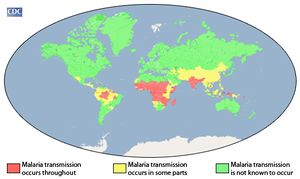
* [[File:Geodistribution2.jpg|right|frameless]]According to the latest ''World malaria report'', released in December 2019, there were 228 million cases of malaria in 2018 compared to 231 million cases in 2017. The estimated number of malaria deaths stood at 405 000 in 2018, compared with 416 000 deaths in 2017. | |||
* The WHO African Region continues to carry a disproportionately high share of the global malaria burden. In 2018, the region was home to 93% of malaria cases and 94% of malaria deaths. | |||
* In 2018, 6 countries accounted for more than half of all malaria cases worldwide: Nigeria (25%), the Democratic Republic of the Congo (12%), Uganda (5%), and Côte d’Ivoire, Mozambique and Niger (4% each). | |||
* Those at highest risk include: children under age 5 (in 2018, they accounted for 67% of all malaria deaths worldwide); pregnant women; disease naïve populations (including refugee populations in Central and Eastern Africa); nonimmune civilian and military travelers; immigrants returning to their place of origin. | |||
* Of the 125 million travelers who visit endemic locations each year, 10000 to 30000 develop malaria, and 1% of these will die from complications of their disease. | |||
* Rising average global temperatures and changes in weather patterns are projected to expand the burden of malaria; a rise of 3 degrees Celsius is postulated to increase malaria incidence by 50 to 80 million<ref name=":1">Buck E, Finnigan NA. [https://www.ncbi.nlm.nih.gov/books/NBK551711/ Malaria. [Updated 2020 Aug 10]]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from:https://www.ncbi.nlm.nih.gov/books/NBK551711/ (last accessed 14.11.2020)</ref><ref name=":0" /> | |||
| |||
== Clinical Presentation == | |||
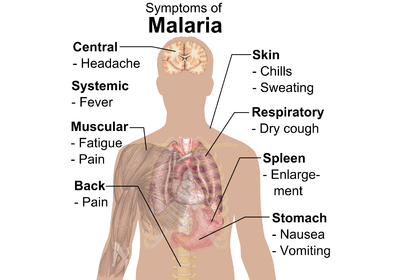
[[File:Malaria whitebackground.png|right|frameless|400x400px]] | |||
== | Malaria is an acute febrile illness. In a non-immune individual, symptoms usually appear 10–15 days after the infective mosquito bite. | ||
* The first symptoms (fever, [[headache]], and chills) may be mild and difficult to recognize as malaria. | |||
* If not treated within 24 hours, P. falciparum malaria can progress to severe illness, often leading to death. | |||
Children with severe malaria frequently develop one or more of the following symptoms: severe [[Anaemia|anaemia]], respiratory distress in relation to metabolic acidosis, or cerebral malaria. In adults, multi-organ failure is also frequent. In malaria endemic areas, people may develop partial immunity, allowing asymptomatic infections to occur<ref name=":0" />.<br> | |||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
Co-morbidities caused by severe Malaria (P. flaciparum) could include cerebral malaria, hypoglycemia, severe | Co-morbidities caused by severe Malaria (P. flaciparum) could include cerebral malaria, hypoglycemia, severe anaemia, pulmonary oedema, respiratory failure, renal failure, and metabolic acidosis.<ref name="F">Fairhurst R, Wellems T: Plasmodium Species (Malaria). In: Mandell G, Bennett J, Dolin R. Principles and Practice of Infectious Diseases. 6th Edition. Philadelphia, Pennsylvania: Elsevier Inc; 2005: 3121-3144.</ref> | ||
# Cerebral Malaria: This form of Malaria can only be caused by P. Flaciparum. It is characterized by “the intense sequestration of parasites in the cerebral microvasculature.” In other words, the parasite invades the blood vessels of the brain and disallows blood to circulate as it normally would. Furthermore, oxygen and glucose supply to the brain is compromised because of improper amounts of blood flow. Cerebral Malaria causes over 80% of the casualties caused by Malaria. Symptoms of cerebral Malaria include seizures, stupor and focal neurological symptoms.<ref name="F" /> | |||
# <u></u>Hypoglycemia :In children, hypoglycemia is caused by the inability of the liver to make new forms of glucose (hepatic gluconeogenesis) because the hepatocytes (liver cells) have been infected. In adults, hypoglycemia is caused by increased amounts of insulin in cells which is a result of stimulation of the islet cells in the pancreas, which are responsible for some insulin production.<ref name="F" /> | |||
# <u></u>[[Anaemia]]: Loss of red blood cells results not only from phagocytic removal of infected erythrocytes, but also removal of uninfected erythrocytes. The bone marrow, which is responsible for blood cell production, is defective in the Malaria infected individual and the result is a decreased level of erythroprotein production and an increased level of phagocytic activity within red blood cells. <ref name="F" /><u></u><u></u><u></u><u></u> | |||
<u></ | # [[Pulmonary Oedema|Pulmonary Edema]] and [[Respiratory Failure]]: Inflammatory cytokines (substances that carry signals between cells) are produced in the lungs in response to erythrocyte sequestration (microvascular obstruction). As a result, capillary permeability is increased which can produce pulmonary oedema, dyspnea, hypoxia, or acute respiratory distress syndrome. <ref name="F" /><u></u><u></u> | ||
# Metabolic Acidosis: Lack of oxygen to the tissues produces acidosis (High H+ concentration and low pH). The effects of anaemia, microvascular obstruction, and hypovolemia (reduced perfusion of the tissues) can cause this lack of oxygen.<ref name="F" /> | |||
<u></u> | |||
<u></u> | |||
<u></u> | |||
<u></u> | |||
<u></u> | |||
<u></u> | |||
For | == Antimalarial Drugs == | ||
Antimalarial medicines can also be used to prevent malaria. For travellers, malaria can be prevented through chemoprophylaxis, which suppresses the blood stage of malaria infections, thereby preventing malaria disease. For pregnant women living in moderate-to-high transmission areas, WHO recommends intermittent preventive treatment with sulfadoxine-pyrimethamine, at each scheduled antenatal visit after the first trimester. Similarly, for infants living in high-transmission areas of Africa, 3 doses of intermittent preventive treatment with sulfadoxine-pyrimethamine are recommended, delivered alongside routine vaccinations. | |||
* Since 2012, WHO has recommended seasonal malaria chemoprevention as an additional malaria prevention strategy for areas of the Sahel sub-region of Africa. The strategy involves the administration of monthly courses of amodiaquine plus sulfadoxine-pyrimethamine to all children under 5 years of age during the high transmission season<ref name=":0" />. | |||
'''<u></u>''' | |||
== <span id="fck_dom_range_temp_1267738224014_451"></span>Prevention == | |||
Vector control is the main way to prevent and reduce malaria transmission. If coverage of vector control interventions within a specific area is high enough, then a measure of protection will be conferred across the community. | |||
< | WHO recommends protection for all people at risk of malaria with effective malaria vector control. Two forms of vector control – insecticide-treated mosquito nets and indoor residual spraying – are effective in a wide range of circumstances.<ref name=":0" /> | ||
== Vaccines == | |||
[[File:Vacinne.jpg|right|frameless]] | |||
RTS,S/AS01 (RTS,S) is the first and, to date, the only [[Vaccines|vaccine]] to show that it can significantly reduce malaria, and life-threatening severe malaria, in young African children. It acts against P. falciparum, the most deadly malaria parasite globally and the most prevalent in Africa. Among children who received 4 doses in large-scale clinical trials, the vaccine prevented approximately 4 in 10 cases of malaria over a 4-year period.<ref name=":0" /> | |||
== Evaluation == | |||
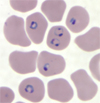
[[File:Falciparum.jpg|right|frameless]] | |||
Initial evaluation of undifferentiated fever in stable patients with possible malaria exposure includes a complete blood count, comprehensive metabolic panel, coagulation panel, blood culture, urinalysis, chest radiograph, and thick and thin blood smears. In patients with altered mental status when cerebral malaria is suspected, a lactate level, arterial blood gas, and lumbar puncture may also be indicated. | |||
* The picture shows malarial parasites within the red bed blood cell on a microscopic blood smear. | |||
'''Diagnosing Severe Malaria:''' can be aided by the recognition of specific criteria designated by the World Health Organization. <sup></sup>Any one of the following criteria along with a positive blood smear for the parasite P. falciparum establishes the diagnoses of severe or complicated Malari<ref name="F" />a: | |||
* Cerebral Malaria- symptoms include decreased consciousness and seizures | |||
* Respiratory distress- symptoms include dyspnea and nasal flaring | |||
* Prostation-lying in the prone position due to a decline in fluid and electrolytes | |||
* Hyperparasitemia- parasite density greater than or equal to 500,000/mm3 | |||
* Severe anaemia- haemoglobin less than or equal to 5 g/dL | |||
* Hypoglycemia- blood glucose less than or equal to 5 g/dL | |||
* Jaundice/icterus- characterized by yellowing of the skin as a result of loss of red blood cells | |||
* Renal Insufficiency- classified as anuria for at least 24 hours | |||
* Hemoglobinuria- dark colored urine | |||
* Shock- decreased perfusion of tissues due to infection of erythrocytes | |||
* Cessation of eating and drinking | |||
* Repetitive vomiting | |||
* Hyperpyrexia- axillary temperature greater than or equal to 40 degrees celsius<u></u><u></u><u></u><u></u><u></u><u></u><u></u><u></u><u></u><u></u><u></u><u></u> | |||
== Physical Therapy Management == | |||
The most important part of physical therapy management of Malaria is the ability to recognize the signs and symptoms of Malaria and quickly refer to a physician for treatment. An efficient diagnosis and treatment can help reduce morbidity and mortality associated with Malaria.<ref name="AMA">Griffith K, Lewis L, Mali S, Parise M. Treatment of Malaria in the United States. JAMA: Journal of the American Medical Association [serial online]. May 23, 2007;297(20):2264-2277. Available from: Academic Search Premier, Ipswich, MA. Accessed April 1, 2010.</ref> Therefore, a physical therapist should always be aware of a patient who has travelled to a Malarious region and Malaria should be considered in any traveller who experiences symptoms of fever within the first year of returning from a Malarious region.<ref name="AMA" /> However, fever does not have to present to diagnose Malaria. Therapists should be cognizant of other symptoms of Malaria including chills, headache, malaise, nausea, vomiting, diarrhoea, abdominal pain, myalgias, back pain, weakness, dizziness, confusion, cough, and/or coma.<ref name="AMA" /> A thorough history can help prevent the spread of infection and even death.<br> | |||
Furthermore, it may be necessary for a therapist to educate a patient who is planning on travelling to a Malarious region on the options for prevention. The best resource for explanation options would be the [http://www.CDC.gov/malaria Center for Disease Control website] | |||
== | == Prevention Advice == | ||
[[File:Rufiji_net.jpg|right|frameless|230x230px]] | |||
Alternative treatment for Malaria is based upon prevention of infection. Prophylaxis is not 100 % effective. Therefore, to prevent the bite of a female Anopheles mosquito one should always wear long sleeves and pants during dusk in Malarious regions and should also sleep under impregnated bed nets. | |||
Bed nets not only prevent mosquitos from biting while an individual is sleeping, but they also kill the mosquitos, helping reduce the risk of infection to everyone in the surrounding community.<ref name="CDCnets">Center for Disease Control: Insecticide-Treated Bed Nets. http://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html. Accessed April 5th, 2010.</ref> The nets are made out of either cotton, polyethylene, or polypropylene and are impregnated with the insecticide, pyrethroid.<ref name="CDCnets" /> These nets usually retain the insectiside for about 6-12 months, but a new line of bed nets called long-lasting insecticide treated nets (LLIS) can last for up to 3 years.<ref name="CDCnets" /><ref>Picture courtesy of the President's Malarial Initiative [http://www.pmi.gov/technical/itn/index.html http://www.pmi.gov/technical/itn/index.html ] </ref> | |||
According to the CDC, The use of insecticide treated bed nets has been proven to be effective in preventing deaths of children under the age of 5. Other clinical trials have proven that the nets are effective at reducing the rate morbidity and mortality among people living in Malarious regions.<ref name="bed2">D'Alessandro U. Insecticide treated bed nets to prevent malaria. BMJ (Clinical Research Ed.) [serial online]. February 3, 2001;322(7281):249-250. Available from: MEDLINE, Ipswich, MA. Accessed April 5, 2010.</ref> <ref name="bed3">Enserink M. Bed Nets Prove Their Mettle Against Malaria. Science [serial online]. December 14, 2001;294(5550):2271. Available from: Academic Search Premier, Ipswich, MA. Accessed April 5, 2010.</ref> They are also effective for the prevention of Malaria in pregnant women, although coverage of bed nets is lacking in Malarial areas such as Kenya.<ref name="Kenya">van Eijk A, Blokland I, Slutsker L, et al. Use of intermittent preventive treatment for malaria in pregnancy in a rural area of western Kenya with high coverage of insecticide-treated bed nets. Tropical Medicine & International Health [serial online]. November 2005;10(11):1134-1140. Available from: Academic Search Premier, Ipswich, MA. Accessed April 5, 2010.</ref> Therefore, programs have been established to help raise money for the funding of nets. | |||
According to the CDC, The use of insecticide treated bed nets has been proven to be effective in preventing deaths of children under the age of 5. Other clinical trials have proven that the nets are effective at reducing the rate morbidity and mortality among people living in Malarious regions.<ref name="bed2">D'Alessandro U. Insecticide treated bed nets to prevent malaria. BMJ (Clinical Research Ed.) [serial online]. February 3, 2001;322(7281):249-250. Available from: MEDLINE, Ipswich, MA. Accessed April 5, 2010.</ref> <ref name="bed3">Enserink M. Bed Nets Prove Their Mettle Against Malaria. Science [serial online]. December 14, 2001;294(5550):2271. Available from: Academic Search Premier, Ipswich, MA. Accessed April 5, 2010.</ref> They are also effective for the prevention of Malaria in pregnant women, although coverage of bed nets is lacking in Malarial areas such as Kenya.<ref name="Kenya">van Eijk A, Blokland I, Slutsker L, et al. Use of intermittent preventive treatment for malaria in pregnancy in a rural area of western Kenya with high coverage of insecticide-treated bed nets. Tropical Medicine & | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Malaria can be similar to multiple other illnesses because of its common symptoms of fever, chills, headache, and malaise. However, Malaria is considered the most likely cause of fever if the patient has recently returned from travel to a Malrious region. The following are other possible diagnoses.<ref name="F" /> | Malaria can be similar to multiple other illnesses because of its common symptoms of fever, chills, headache, and malaise. However, Malaria is considered the most likely cause of fever if the patient has recently returned from travel to a Malrious region. The following are other possible diagnoses.<ref name="F" /> | ||
* <u>Influenza</u>- The flu is similar to Malaria in that they share multiple symptoms including fever, malaise, headache, and myalgia. However, upper respiratory symptoms are more likely to present in a patient who has the flu. | |||
<u> | * <u>Typhoid Fever</u>- Similar symptoms including fever, headache, nausea, and malaise make it difficult to distinguish Malaria from enteric fever. The diagnosis is likely to be enteric fever if the patient has a history of unsanitary food or water intake as well as gastrointestinal symptoms. | ||
* <u>[[Sepsis]]</u> | |||
<u> | * <u>Dengue Fever</u>- Although this illness, like Malaria, is contracted from a Mosquito, symptoms arise more quickly compared to Malaria (4-7 days). The two infections have similar symptoms, but patients with Dengue fever will likely have a rash, erythema, and bradycardia to accompany fever, headache, nausea, and malaise. | ||
* <u>Acute Schistoosomiasis (Katayama Fever)- </u>The signs of Katayama fever present about 4-8 weeks after exposure fresh water in a tropical region. Like Malaria, the patient may have fever, headache, and malaise, but will more than likely also present with a rash, urticaria, lymphadenopathy, and blood eosinophilia. | |||
<u>[ | * <u>[[Leptospirosis]]</u> | ||
* <u>African Tick Fever</u>- Also known as Rickettsia Africae, the Tick Fever can present with fever, headache, and myalgias. Unlike Malaria, it is likely that the patient will have lymphadenitis and inoculation eschars. | |||
<u> | * <u>East African Trypanosomiasis (Sleeping Sickness)- </u>Symptoms of fever, malaise, headache, and myalgia, are likely but the Sleeping Sickness can also present with a red rash because of the bite of a tsetse fly. Also, posterior cervical lymphadenopathy (rash) is a common sign of Trypanomiasis. | ||
* <u>Yellow Fever</u>- The Yellow Fever, like Malaria, is caused by a mosquito bite in a tropical region and both illnesses have similar symptoms. However, bradycardia can present in the patient with Yellow Fever and symptoms take effect within 3-6 days, unlike Malaria. | |||
<u> | |||
<u>[ | |||
<u> | |||
<u> | |||
<u> | |||
'' | == WHO Global technical strategy for malaria 2016-2030 == | ||
The WHO ''Global technical strategy for malaria 2016-2030'' – adopted by the World Health Assembly in May 2015 – provides a technical framework for all malaria-endemic countries. It is intended to guide and support regional and country programmes as they work towards malaria control and elimination. | |||
The Strategy sets ambitious but achievable global targets, including: | |||
* reducing malaria case incidence by at least 90% by 2030; | |||
* reducing malaria mortality rates by at least 90% by 2030; | |||
* eliminating malaria in at least 35 countries by 2030; | |||
* preventing a resurgence of malaria in all countries that are malaria-free. | |||
This Strategy was the result of an extensive consultative process that spanned 2 years and involved the participation of more than 400 technical experts from 70 Member States.<ref name=":0" /> | |||
== References == | == References == | ||
<references /> | <references /><br> | ||
[[Category:Medical]] | |||
[[Category:Global Health]] | |||
[[Category:Bellarmine Student Project]] | |||
[[Category:Womens Health]] | |||
[[Category:Communicable Diseases]] | |||
Latest revision as of 08:39, 5 January 2022
Original Editors - Aaron Hume from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Aaron Hume, Admin, Lucinda hampton, Dave Pariser, Kim Jackson, Tony Lowe, Wendy Walker, WikiSysop, Nupur Smit Shah, 127.0.0.1, Elaine Lonnemann and Evan Thomas
Definition/Description[edit | edit source]
Malaria is caused by Plasmodium parasites. The parasites are spread to people through the bites of infected female Anopheles mosquitoes, called "malaria vectors." There are 5 parasite species that cause malaria in humans, and 2 of these species – P. falciparum and P. vivax – pose the greatest threat.
- Malaria is a life-threatening disease.
- It is preventable and curable.
- In 2018, there were an estimated 228 million cases of malaria worldwide.[1]
Etiology[edit | edit source]
Five Plasmodium species possess the ability to infect humans: P. falciparum, P. ovale, P. vivax, P. malariae, and P. knowlesi.[2][3]
- Transmission can also occur by way of blood transfusion, organ transplant, the sharing of needles with contaminated blood, or by congenital means when a mother passes the infection to her unborn baby. Furthermore, “Airport” Malaria can occur when infected mosquitos are transported from a Malarious region to an area not affected by Malaria. Subsequently, civilians of the non-endemic region can be infected by Malaria without having travelled to a foreign country.[4]
- Once the parasites are inside your body, they travel to the liver, where they mature. After several days, the mature parasites enter the bloodstream and begin to infect red blood cells.
- Within 48 to 72 hours, the parasites inside the red blood cells multiply, causing the infected cells to burst open.
- The parasites continue to infect red blood cells, resulting in symptoms that occur in cycles that last two to three days at a time[5].
The below video describes the the sequence of events causing an infection by a Malarial parasite and also describes how the infection can spread throughout the body
Epidemiology[edit | edit source]
- According to the latest World malaria report, released in December 2019, there were 228 million cases of malaria in 2018 compared to 231 million cases in 2017. The estimated number of malaria deaths stood at 405 000 in 2018, compared with 416 000 deaths in 2017.
- The WHO African Region continues to carry a disproportionately high share of the global malaria burden. In 2018, the region was home to 93% of malaria cases and 94% of malaria deaths.
- In 2018, 6 countries accounted for more than half of all malaria cases worldwide: Nigeria (25%), the Democratic Republic of the Congo (12%), Uganda (5%), and Côte d’Ivoire, Mozambique and Niger (4% each).
- Those at highest risk include: children under age 5 (in 2018, they accounted for 67% of all malaria deaths worldwide); pregnant women; disease naïve populations (including refugee populations in Central and Eastern Africa); nonimmune civilian and military travelers; immigrants returning to their place of origin.
- Of the 125 million travelers who visit endemic locations each year, 10000 to 30000 develop malaria, and 1% of these will die from complications of their disease.
- Rising average global temperatures and changes in weather patterns are projected to expand the burden of malaria; a rise of 3 degrees Celsius is postulated to increase malaria incidence by 50 to 80 million[2][1]
Clinical Presentation[edit | edit source]
Malaria is an acute febrile illness. In a non-immune individual, symptoms usually appear 10–15 days after the infective mosquito bite.
- The first symptoms (fever, headache, and chills) may be mild and difficult to recognize as malaria.
- If not treated within 24 hours, P. falciparum malaria can progress to severe illness, often leading to death.
Children with severe malaria frequently develop one or more of the following symptoms: severe anaemia, respiratory distress in relation to metabolic acidosis, or cerebral malaria. In adults, multi-organ failure is also frequent. In malaria endemic areas, people may develop partial immunity, allowing asymptomatic infections to occur[1].
Associated Co-morbidities[edit | edit source]
Co-morbidities caused by severe Malaria (P. flaciparum) could include cerebral malaria, hypoglycemia, severe anaemia, pulmonary oedema, respiratory failure, renal failure, and metabolic acidosis.[7]
- Cerebral Malaria: This form of Malaria can only be caused by P. Flaciparum. It is characterized by “the intense sequestration of parasites in the cerebral microvasculature.” In other words, the parasite invades the blood vessels of the brain and disallows blood to circulate as it normally would. Furthermore, oxygen and glucose supply to the brain is compromised because of improper amounts of blood flow. Cerebral Malaria causes over 80% of the casualties caused by Malaria. Symptoms of cerebral Malaria include seizures, stupor and focal neurological symptoms.[7]
- Hypoglycemia :In children, hypoglycemia is caused by the inability of the liver to make new forms of glucose (hepatic gluconeogenesis) because the hepatocytes (liver cells) have been infected. In adults, hypoglycemia is caused by increased amounts of insulin in cells which is a result of stimulation of the islet cells in the pancreas, which are responsible for some insulin production.[7]
- Anaemia: Loss of red blood cells results not only from phagocytic removal of infected erythrocytes, but also removal of uninfected erythrocytes. The bone marrow, which is responsible for blood cell production, is defective in the Malaria infected individual and the result is a decreased level of erythroprotein production and an increased level of phagocytic activity within red blood cells. [7]
- Pulmonary Edema and Respiratory Failure: Inflammatory cytokines (substances that carry signals between cells) are produced in the lungs in response to erythrocyte sequestration (microvascular obstruction). As a result, capillary permeability is increased which can produce pulmonary oedema, dyspnea, hypoxia, or acute respiratory distress syndrome. [7]
- Metabolic Acidosis: Lack of oxygen to the tissues produces acidosis (High H+ concentration and low pH). The effects of anaemia, microvascular obstruction, and hypovolemia (reduced perfusion of the tissues) can cause this lack of oxygen.[7]
Antimalarial Drugs[edit | edit source]
Antimalarial medicines can also be used to prevent malaria. For travellers, malaria can be prevented through chemoprophylaxis, which suppresses the blood stage of malaria infections, thereby preventing malaria disease. For pregnant women living in moderate-to-high transmission areas, WHO recommends intermittent preventive treatment with sulfadoxine-pyrimethamine, at each scheduled antenatal visit after the first trimester. Similarly, for infants living in high-transmission areas of Africa, 3 doses of intermittent preventive treatment with sulfadoxine-pyrimethamine are recommended, delivered alongside routine vaccinations.
- Since 2012, WHO has recommended seasonal malaria chemoprevention as an additional malaria prevention strategy for areas of the Sahel sub-region of Africa. The strategy involves the administration of monthly courses of amodiaquine plus sulfadoxine-pyrimethamine to all children under 5 years of age during the high transmission season[1].
Prevention[edit | edit source]
Vector control is the main way to prevent and reduce malaria transmission. If coverage of vector control interventions within a specific area is high enough, then a measure of protection will be conferred across the community.
WHO recommends protection for all people at risk of malaria with effective malaria vector control. Two forms of vector control – insecticide-treated mosquito nets and indoor residual spraying – are effective in a wide range of circumstances.[1]
Vaccines[edit | edit source]
RTS,S/AS01 (RTS,S) is the first and, to date, the only vaccine to show that it can significantly reduce malaria, and life-threatening severe malaria, in young African children. It acts against P. falciparum, the most deadly malaria parasite globally and the most prevalent in Africa. Among children who received 4 doses in large-scale clinical trials, the vaccine prevented approximately 4 in 10 cases of malaria over a 4-year period.[1]
Evaluation[edit | edit source]
Initial evaluation of undifferentiated fever in stable patients with possible malaria exposure includes a complete blood count, comprehensive metabolic panel, coagulation panel, blood culture, urinalysis, chest radiograph, and thick and thin blood smears. In patients with altered mental status when cerebral malaria is suspected, a lactate level, arterial blood gas, and lumbar puncture may also be indicated.
- The picture shows malarial parasites within the red bed blood cell on a microscopic blood smear.
Diagnosing Severe Malaria: can be aided by the recognition of specific criteria designated by the World Health Organization. Any one of the following criteria along with a positive blood smear for the parasite P. falciparum establishes the diagnoses of severe or complicated Malari[7]a:
- Cerebral Malaria- symptoms include decreased consciousness and seizures
- Respiratory distress- symptoms include dyspnea and nasal flaring
- Prostation-lying in the prone position due to a decline in fluid and electrolytes
- Hyperparasitemia- parasite density greater than or equal to 500,000/mm3
- Severe anaemia- haemoglobin less than or equal to 5 g/dL
- Hypoglycemia- blood glucose less than or equal to 5 g/dL
- Jaundice/icterus- characterized by yellowing of the skin as a result of loss of red blood cells
- Renal Insufficiency- classified as anuria for at least 24 hours
- Hemoglobinuria- dark colored urine
- Shock- decreased perfusion of tissues due to infection of erythrocytes
- Cessation of eating and drinking
- Repetitive vomiting
- Hyperpyrexia- axillary temperature greater than or equal to 40 degrees celsius
Physical Therapy Management[edit | edit source]
The most important part of physical therapy management of Malaria is the ability to recognize the signs and symptoms of Malaria and quickly refer to a physician for treatment. An efficient diagnosis and treatment can help reduce morbidity and mortality associated with Malaria.[8] Therefore, a physical therapist should always be aware of a patient who has travelled to a Malarious region and Malaria should be considered in any traveller who experiences symptoms of fever within the first year of returning from a Malarious region.[8] However, fever does not have to present to diagnose Malaria. Therapists should be cognizant of other symptoms of Malaria including chills, headache, malaise, nausea, vomiting, diarrhoea, abdominal pain, myalgias, back pain, weakness, dizziness, confusion, cough, and/or coma.[8] A thorough history can help prevent the spread of infection and even death.
Furthermore, it may be necessary for a therapist to educate a patient who is planning on travelling to a Malarious region on the options for prevention. The best resource for explanation options would be the Center for Disease Control website
Prevention Advice[edit | edit source]
Alternative treatment for Malaria is based upon prevention of infection. Prophylaxis is not 100 % effective. Therefore, to prevent the bite of a female Anopheles mosquito one should always wear long sleeves and pants during dusk in Malarious regions and should also sleep under impregnated bed nets.
Bed nets not only prevent mosquitos from biting while an individual is sleeping, but they also kill the mosquitos, helping reduce the risk of infection to everyone in the surrounding community.[9] The nets are made out of either cotton, polyethylene, or polypropylene and are impregnated with the insecticide, pyrethroid.[9] These nets usually retain the insectiside for about 6-12 months, but a new line of bed nets called long-lasting insecticide treated nets (LLIS) can last for up to 3 years.[9][10]
According to the CDC, The use of insecticide treated bed nets has been proven to be effective in preventing deaths of children under the age of 5. Other clinical trials have proven that the nets are effective at reducing the rate morbidity and mortality among people living in Malarious regions.[11] [12] They are also effective for the prevention of Malaria in pregnant women, although coverage of bed nets is lacking in Malarial areas such as Kenya.[13] Therefore, programs have been established to help raise money for the funding of nets.
Differential Diagnosis[edit | edit source]
Malaria can be similar to multiple other illnesses because of its common symptoms of fever, chills, headache, and malaise. However, Malaria is considered the most likely cause of fever if the patient has recently returned from travel to a Malrious region. The following are other possible diagnoses.[7]
- Influenza- The flu is similar to Malaria in that they share multiple symptoms including fever, malaise, headache, and myalgia. However, upper respiratory symptoms are more likely to present in a patient who has the flu.
- Typhoid Fever- Similar symptoms including fever, headache, nausea, and malaise make it difficult to distinguish Malaria from enteric fever. The diagnosis is likely to be enteric fever if the patient has a history of unsanitary food or water intake as well as gastrointestinal symptoms.
- Sepsis
- Dengue Fever- Although this illness, like Malaria, is contracted from a Mosquito, symptoms arise more quickly compared to Malaria (4-7 days). The two infections have similar symptoms, but patients with Dengue fever will likely have a rash, erythema, and bradycardia to accompany fever, headache, nausea, and malaise.
- Acute Schistoosomiasis (Katayama Fever)- The signs of Katayama fever present about 4-8 weeks after exposure fresh water in a tropical region. Like Malaria, the patient may have fever, headache, and malaise, but will more than likely also present with a rash, urticaria, lymphadenopathy, and blood eosinophilia.
- Leptospirosis
- African Tick Fever- Also known as Rickettsia Africae, the Tick Fever can present with fever, headache, and myalgias. Unlike Malaria, it is likely that the patient will have lymphadenitis and inoculation eschars.
- East African Trypanosomiasis (Sleeping Sickness)- Symptoms of fever, malaise, headache, and myalgia, are likely but the Sleeping Sickness can also present with a red rash because of the bite of a tsetse fly. Also, posterior cervical lymphadenopathy (rash) is a common sign of Trypanomiasis.
- Yellow Fever- The Yellow Fever, like Malaria, is caused by a mosquito bite in a tropical region and both illnesses have similar symptoms. However, bradycardia can present in the patient with Yellow Fever and symptoms take effect within 3-6 days, unlike Malaria.
WHO Global technical strategy for malaria 2016-2030[edit | edit source]
The WHO Global technical strategy for malaria 2016-2030 – adopted by the World Health Assembly in May 2015 – provides a technical framework for all malaria-endemic countries. It is intended to guide and support regional and country programmes as they work towards malaria control and elimination.
The Strategy sets ambitious but achievable global targets, including:
- reducing malaria case incidence by at least 90% by 2030;
- reducing malaria mortality rates by at least 90% by 2030;
- eliminating malaria in at least 35 countries by 2030;
- preventing a resurgence of malaria in all countries that are malaria-free.
This Strategy was the result of an extensive consultative process that spanned 2 years and involved the participation of more than 400 technical experts from 70 Member States.[1]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 WHO Malaria Available from:https://www.who.int/news-room/fact-sheets/detail/malaria (last accessed 14.11.2020)
- ↑ 2.0 2.1 Buck E, Finnigan NA. Malaria. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from:https://www.ncbi.nlm.nih.gov/books/NBK551711/ (last accessed 14.11.2020)
- ↑ Picture courtesy of http://qspace.library.queensu.ca/dspace/html/1974/421/pfalcip01.htm
- ↑ Malaria. Centers for Disease Control and Prevention Web Site. http://www.CDC.gov/malaria. Updated June, 2009. Accessed March 1st, 2010.
- ↑ Healthline Malaria Available from:https://www.healthline.com/health/malaria (last accessed 14.11.2020)
- ↑ You Tube. HHMI -- Life Cycle of Malaria Parasite in Human Host.http://www.youtube.com/watch?v=qvlTOhCmxvY. Accessed Feb 12th, 2019.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 Fairhurst R, Wellems T: Plasmodium Species (Malaria). In: Mandell G, Bennett J, Dolin R. Principles and Practice of Infectious Diseases. 6th Edition. Philadelphia, Pennsylvania: Elsevier Inc; 2005: 3121-3144.
- ↑ 8.0 8.1 8.2 Griffith K, Lewis L, Mali S, Parise M. Treatment of Malaria in the United States. JAMA: Journal of the American Medical Association [serial online]. May 23, 2007;297(20):2264-2277. Available from: Academic Search Premier, Ipswich, MA. Accessed April 1, 2010.
- ↑ 9.0 9.1 9.2 Center for Disease Control: Insecticide-Treated Bed Nets. http://www.cdc.gov/malaria/malaria_worldwide/reduction/itn.html. Accessed April 5th, 2010.
- ↑ Picture courtesy of the President's Malarial Initiative http://www.pmi.gov/technical/itn/index.html
- ↑ D'Alessandro U. Insecticide treated bed nets to prevent malaria. BMJ (Clinical Research Ed.) [serial online]. February 3, 2001;322(7281):249-250. Available from: MEDLINE, Ipswich, MA. Accessed April 5, 2010.
- ↑ Enserink M. Bed Nets Prove Their Mettle Against Malaria. Science [serial online]. December 14, 2001;294(5550):2271. Available from: Academic Search Premier, Ipswich, MA. Accessed April 5, 2010.
- ↑ van Eijk A, Blokland I, Slutsker L, et al. Use of intermittent preventive treatment for malaria in pregnancy in a rural area of western Kenya with high coverage of insecticide-treated bed nets. Tropical Medicine & International Health [serial online]. November 2005;10(11):1134-1140. Available from: Academic Search Premier, Ipswich, MA. Accessed April 5, 2010.