Groin Strain: Difference between revisions
No edit summary |
No edit summary |
||
| Line 13: | Line 13: | ||
== Introduction == | == Introduction == | ||
Groin pain is a common injury with varied clinical presentations and diagnostic term which makes it a difficult injury to manage. In a systematic review on the treatment of a groin pain in athletes, more than 30 diagnostic terminologies were used to describe groin pain which add up to the complexity of groin injuries in athletes. | Groin pain is a common injury with varied clinical presentations and diagnostic term which makes it a difficult injury to manage. In a systematic review on the treatment of a groin pain in athletes, more than 30 diagnostic terminologies were used to describe groin pain which add up to the complexity of groin injuries in athletes.<ref>Serner A, van Eijck CH, Beumer BR, Hölmich P, Weir A, de Vos RJ. [https://pubmed.ncbi.nlm.nih.gov/25633830/ Study quality on groin injury management remains low: a systematic review on treatment of groin pain in athletes. British journal of sports medicine]. 2015 Jun 1;49(12):813-.</ref> | ||
In attempt to address the terminology challenge, a consensus meeting was held in Doha, Qatar during the first World Conference of Grain Pain in Athletes , in November 2014. A group of 24 experts from 14 different countries were invited to agree on a standard terminology, along with accompanying definitions. ( | In attempt to address the terminology challenge, a consensus meeting was held in Doha, Qatar during the first World Conference of Grain Pain in Athletes , in November 2014. A group of 24 experts from 14 different countries were invited to agree on a standard terminology, along with accompanying definitions. <ref name=":2">Weir A, Brukner P, Delahunt E, Ekstrand J, Griffin D, Khan KM, Lovell G, Meyers WC, Muschaweck U, Orchard J, Paajanen H. [https://bjsm.bmj.com/content/49/12/768.short Doha agreement meeting on terminology and definitions in groin pain in athletes. British journal of sports medicine]. 2015 Jun 1;49(12):768-74.</ref> | ||
A classification system were groin pain was described in three main subheading was agreed on during the Doha agreement meeting; | A classification system were groin pain was described in three main subheading was agreed on during the Doha agreement meeting; | ||
| Line 31: | Line 31: | ||
== Definition/Description == | == Definition/Description == | ||
An adductor-related groin pain/[[Muscle Strain|strain]] is an injury to the muscle-tendon unit that produces pain on palpation of the adductor tendons or its insertion on the pubic bone and pain in the adductor region on resistance testing of the adductors. | An adductor-related groin pain/[[Muscle Strain|strain]] is an injury to the muscle-tendon unit that produces pain on palpation of the adductor tendons or its insertion on the pubic bone and pain in the adductor region on resistance testing of the adductors.<ref name=":2" /> Groin muscle strains are encountered more frequently in ice hockey and soccer.<ref name=":3">Orchard JW. [https://bjsm.bmj.com/content/49/12/798.short Men at higher risk of groin injuries in elite team sports: a systematic review]. British journal of sports medicine. 2015 Jun 1;49(12):798-802.</ref> | ||
[[File:Adductor magnus.png|right|frameless|263x263px]] | [[File:Adductor magnus.png|right|frameless|263x263px]] | ||
These sports require a strong eccentric contraction of the adductor musculature during competition and practice.<ref name="'Tyler'">Tyler TF, Fukunaga T, Gellert J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4223288/ Rehabilitation of soft tissue injuries of the hip and pelvis.] International journal of sports physical therapy 2014;9(6):785.</ref> The underlying injury is most often a muscle or tendon strain at the insertion of the tendon of the adductor muscle to the bone.<ref name="'Gino'">Kerkhoffs GM, Servien E, editors. [https://link.springer.com/book/10.1007%2F978-3-319-03722-6 Acute muscle injuries.] Springer International Publishing; 2014.</ref> The [[Adductor Longus|adductor longus]] is most commonly injured.<ref>Kiel J, Kaiser K. [https://europepmc.org/article/NBK/NBK493166 Adductor Strain.] StatPearls Publishing, Treasure Island; 2018.</ref> | These sports require a strong eccentric contraction of the adductor musculature during competition and practice.<ref name="'Tyler'">Tyler TF, Fukunaga T, Gellert J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4223288/ Rehabilitation of soft tissue injuries of the hip and pelvis.] International journal of sports physical therapy 2014;9(6):785.</ref> The underlying injury is most often a muscle or tendon strain at the insertion of the tendon of the adductor muscle to the bone.<ref name="'Gino'">Kerkhoffs GM, Servien E, editors. [https://link.springer.com/book/10.1007%2F978-3-319-03722-6 Acute muscle injuries.] Springer International Publishing; 2014.</ref> The [[Adductor Longus|adductor longus]] is most commonly injured.<ref name=":4">Kiel J, Kaiser K. [https://europepmc.org/article/NBK/NBK493166 Adductor Strain.] StatPearls Publishing, Treasure Island; 2018.</ref> | ||
The difference between groin tendinopathy and strain are: | The difference between groin tendinopathy and strain are: | ||
| Line 52: | Line 52: | ||
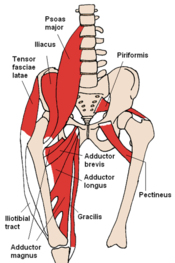
* The adductor group: The adductors of the hip joint include 6 muscles: the [[Adductor Longus|adductor longus]], [[Adductor Magnus|magnus]] and [[Adductor Brevis|brevis]], [[gracilis]], [[Obturator Externus|obturator externus]], and [[Pectinus Muscle|pectineus]]. All these are innervated by the [[Obturator Nerve|obturator nerve]], with the exception of the [[Pectinus Muscle|pectineus]], which receives innervation from the femoral nerve. The adductors all originate on the [[Pubis|pubic]] ramus as almost all insert on the linea aspera of the posterior femur. The posterior head of the [[Adductor Magnus|adductor magnus]] has a proximal attachment on the ischial tuberosity anteroinferiorly and attaches distally on the medial distal femur at the adductor tubercle. The gracilis insertion is on the medial border of the tuberosity of the tibia. The primary function of this muscle group is adduction of the thigh in open-chain motions and stabilization of the lower extremity and pelvis in closed chain motion. | * The adductor group: The adductors of the hip joint include 6 muscles: the [[Adductor Longus|adductor longus]], [[Adductor Magnus|magnus]] and [[Adductor Brevis|brevis]], [[gracilis]], [[Obturator Externus|obturator externus]], and [[Pectinus Muscle|pectineus]]. All these are innervated by the [[Obturator Nerve|obturator nerve]], with the exception of the [[Pectinus Muscle|pectineus]], which receives innervation from the femoral nerve. The adductors all originate on the [[Pubis|pubic]] ramus as almost all insert on the linea aspera of the posterior femur. The posterior head of the [[Adductor Magnus|adductor magnus]] has a proximal attachment on the ischial tuberosity anteroinferiorly and attaches distally on the medial distal femur at the adductor tubercle. The gracilis insertion is on the medial border of the tuberosity of the tibia. The primary function of this muscle group is adduction of the thigh in open-chain motions and stabilization of the lower extremity and pelvis in closed chain motion. | ||
In football, majority of groin injuries are adductor related. <ref>Hölmich P, Thorborg K, Dehlendorff C, Krogsgaard K, Gluud C. [https://bjsm.bmj.com/content/48/16/1245.short Incidence and clinical presentation of groin injuries in sub-elite male soccer.] British journal of sports medicine. 2014 Aug 1;48(16):1245-50.</ref> The proximal attachment of the [[Adductor Longus|adductor longus]] contributes to an anatomical pathway across the anterior pubic symphysis that is likely required to withstand the transmission of large forces during multidirectional athletic activities. Its lack of mechanical advantage may make it more susceptible to strain.<ref name="'Norton-old'">Norton‐old KJ, Schache AG, Barker PJ, Clark RA, Harrison SM, Briggs CA. [https://d1wqtxts1xzle7.cloudfront.net/49700088/ca.2211620161018-8888-1l38i3h.pdf?1476835149=&response-content-disposition=inline%3B+filename%3DAnatomical_and_mechanical_relationship_b.pdf&Expires=1595263708&Signature=fAsRGkdBhCibLIz1y4BG8~wxqpBlOwVCviQxiz Anatomical and mechanical relationship between the proximal attachment of adductor longus and the distal rectus sheath.] Clinical Anatomy 2013;26(4):522-30.</ref> | |||
*The abdominal group: The abdominal musculature comprise the [[Rectus Abdominis|rectus abdominis]], the [[Internal Abdominal Oblique|obliques internus]] and [[External Abdominal Oblique|externus abdominis]]. (See page for [[Abdominal Muscles|abdominal muscles]]). | *The abdominal group: The abdominal musculature comprise the [[Rectus Abdominis|rectus abdominis]], the [[Internal Abdominal Oblique|obliques internus]] and [[External Abdominal Oblique|externus abdominis]]. (See page for [[Abdominal Muscles|abdominal muscles]]). | ||
| Line 60: | Line 60: | ||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
Groin strains are common amongst athletes who compete in sports that involve repetitive twisting, turning, sprinting and kicking. Groin injuries accounted for 4–19% of all injuries | Groin strains are common amongst athletes who compete in sports that involve repetitive twisting, turning, sprinting and kicking such as football, ice hokey, Australian and Gaelic football.<ref name=":3" /> Groin injuries are reported more in male compared to female football athletes. Injuries in men accounted for 4–19% of all injuries and 2–14% in women.<ref>Waldén M, Hägglund M, Ekstrand J. [https://bjsm.bmj.com/content/49/12/792.short The epidemiology of groin injury in senior football: a systematic review of prospective studies.] British journal of sports medicine. 2015 Jun 1;49(12):792-7.</ref> | ||
The exact incidence of groin muscle strains in most sports is unknown because athletes often play through minor groin pain and the injury goes unreported. In addition, overlapping diagnoses can skew the incidence.<ref name="'Tyler, T.'" /> Cumulative or single injury seem to be important etiological factors. Chronic tendinitis of the adductor muscles/tendons, especially that of the [[Adductor Longus|adductor longus]], is the most frequently diagnosed.<ref name=":4" /> | |||
The exact incidence of groin muscle strains in most sports is unknown because athletes often play through minor groin pain and the injury goes unreported. In addition, overlapping diagnoses can skew the incidence. | |||
Injury mechanism can be divided into 3 groups: | Injury mechanism can be divided into 3 groups: | ||
# Direct blunt trauma: An acute injury, typically a direct injury to the soft tissues resulting in muscle hematoma. | # Direct blunt trauma: An acute injury, typically a direct injury to the soft tissues resulting in muscle hematoma. | ||
# Forceful contraction: The most common groin injury in athletes is muscle and tendon strain of the adductor muscle group. Change of direction and kicking have been described as the main actions resulting in [[Adductor Longus|adductor longus]] injury. Videos analysis of acute [[Adductor Longus|adductor longus]][ | # Forceful contraction: The most common groin injury in athletes is muscle and tendon strain of the adductor muscle group. Change of direction and kicking have been described as the main actions resulting in [[Adductor Longus|adductor longus]] injury. Videos analysis of acute [[Adductor Longus|adductor longus]] <ref>Serner A, Mosler AB, Tol JL, Bahr R, Weir A. [https://bjsm.bmj.com/content/53/3/158.abstract Mechanisms of acute adductor longus injuries in male football players: a systematic visual video analysis]. British journal of sports medicine. 2019 Feb 1;53(3):158-64.</ref> injuries in 17 professional male football players showed most injuries occurred in non-contact situations (71%), following a quick reaction to a change in play (53%). Injury actions were: change of direction (35%), kicking (29%), reaching (24%) and jumping (12%). Change of direction and reaching injuries were categorised as closed chain movements (59%), characterised by [[hip]] extension and abduction with external rotation. Kicking and jumping injuries were categorised as an open chain (41%), characterised by a change from hip extension to hip flexion, and hip abduction to adduction, with external rotation. So a rapid muscle activation during a rapid muscle lengthening appears to be the fundamental injury mechanism for acute [[Adductor Longus|adductor longus]] injuries. The adductors attempt to decelerate an extending, abducting leg by using an eccentric contraction to adduct and flex the hip was the main cause of injury. The injury may also occur during a forceful concentric contraction of the muscle.<ref name="'Mc'" /> Lower-extremity athletes such as ice hockey and soccer players are naturally more prone to this pathology due to the repetitive twisting, turning, sprinting and kicking.<ref name=":3" /> | ||
# Microtrauma by repetitive injury: musculotendinous injuries to the groin are mainly a consequence of cumulative microtraumas (overuse trauma, repeated minor injuries) leading to chronic groin pain. | # Microtrauma by repetitive injury: musculotendinous injuries to the groin are mainly a consequence of cumulative microtraumas (overuse trauma, repeated minor injuries) leading to chronic groin pain. | ||
And subsequently result in muscle contusions, avulsions, tears and strains. | And subsequently result in muscle contusions, avulsions, tears and strains. | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
The main sign of the adductor-related groin injury is intense pain in the groin area. [[Muscle Strain|Muscle strain]] injuries often arise from excessive stretching or stretching when the muscle is being activated. When there is a strain in the muscle, the damage is often localized near the muscle-tendon junction. Acute adductor longus injuries may also involve tendinous rupture/ avulsion, primarily at the proximal insertions. | The main sign of the adductor-related groin injury is intense pain in the groin area. [[Muscle Strain|Muscle strain]] injuries often arise from excessive stretching or stretching when the muscle is being activated. When there is a strain in the muscle, the damage is often localized near the muscle-tendon junction. Acute adductor longus injuries may also involve tendinous rupture/ avulsion, primarily at the proximal insertions. <ref>Serner A, Weir A, Tol JL, Thorborg K, Roemer F, Guermazi A, Yamashiro E, Hölmich P. [https://onlinelibrary.wiley.com/doi/abs/10.1111/sms.12936 Characteristics of acute groin injuries in the adductor muscles: a detailed MRI study in athletes]. Scandinavian journal of medicine & science in sports. 2018 Feb;28(2):667-76.</ref> | ||
Clinically for an adductor strain, the patient presents with pain in the inner thigh and tenderness along the muscle belly, tendon or insertion. The pain is exacerbated by adduction.[16]. Tears frequently occur at the myotendinous junction, which is the weakest part of the muscle-tendon unit but is also commonly seen in the muscle belly. The same mechanism of injury that results in a muscle tear in an adult may cause an apophyseal avulsion in an adolescent. There is a well-established clinical grading system for muscle tears, which has 3 components:<ref>Davies AG, Clarke AW, Gilmore J, Wotherspoon M, Connell DA. [https://link.springer.com/article/10.1007/s00256-009-0768-9 imaging of groin pain in the athlete. Skeletal radiology]. 2010 Jul;39(7):629-44.</ref> | |||
* Grade 1: no loss of function or strength. Muscle tears can show normal appearances or a small area of focal disruption (<5% of the muscle volume), with hematoma and perifascial fluid relatively common on imaging with US and MRI. | |||
* Grade 2: severe, with some weakness. Injury corresponds to a partial tear, with muscle fibre disruption seen (>5% of the muscle volume) but not affecting the whole muscle belly. In '''acute''' grade 1 or 2 strains of the adductor muscle, there is intense pain in the groin area, like a sudden stab with a knife, if the athlete attempts to continue the activity. Locally a haemorrhage and swelling can be seen a few days after the injury. A typical trauma history, localized tenderness and difficulties to contract the hip abductors. | |||
* Grade 3: complete muscle tear and complete functional loss. Injuries are complete muscle tears with frayed margins and bunching and/or retraction of the torn muscle fibres.<span class="reference" id="cite_ref-.27Mc.27_11-1"></span> Complete muscle tears or grade 3 strains are most often found in the distal musculotendinous junction located toward the insertion on the femur. | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Traditionally, groin pain has thought to be complex with various definition and no diagnostic criteria [8] until the recently. The Doha agreement meeting on groin pain has provided a classification system for the definition and diagnosis of the various causes of groin pain [doha]. The table below presents the | Traditionally, groin pain has thought to be complex with various definition and no diagnostic criteria [8] until the recently. The Doha agreement meeting on groin pain has provided a classification system for the definition and diagnosis of the various causes of groin pain [doha]. The table below presents the | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+The Doha agreement on diagnostic classification <ref name=":2" /> | ||
!Defined Entities. | !'''Defined Entities.''' | ||
!Other musculoskeletal causes. | !'''Other musculoskeletal causes.''' | ||
!Not to be missed. | !'''Not to be missed.''' | ||
|- | |- | ||
| | | | ||
| Line 105: | Line 100: | ||
* Hip-related groin pain | * Hip-related groin pain | ||
| Line 142: | Line 138: | ||
#* Anterior inferior iliac spine | #* Anterior inferior iliac spine | ||
#* Pubic bone | #* Pubic bone | ||
# Referred pain | # Referred pain | ||
| Line 158: | Line 154: | ||
| | | | ||
Stress fracture | Stress fracture | ||
| Line 167: | Line 162: | ||
* Acetabulum | * Acetabulum | ||
[[Hip Anatomy|Hip joint]] | [[Hip Anatomy|Hip joint]] | ||
| Line 178: | Line 172: | ||
* Arthritis of the hip joint (reactive or infectious) | * Arthritis of the hip joint (reactive or infectious) | ||
Inguinal lymphadenopathy Intra-abdominal abnormality | Inguinal lymphadenopathy Intra-abdominal abnormality | ||
| Line 190: | Line 183: | ||
* Diverticulitis | * Diverticulitis | ||
Gynaecological conditions Spondyloarthropathies | Gynaecological conditions Spondyloarthropathies | ||
| Line 202: | Line 194: | ||
* Urinary tract cancer ▸ Digestive tract cancer ▸ Soft tissue tumours | * Urinary tract cancer ▸ Digestive tract cancer ▸ Soft tissue tumours | ||
| Line 210: | Line 204: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
First of all, there needs to be a patient history and an identification of the pain by the examination of the physiotherapist. On evaluation, there is tenderness to palpation with focal swelling of the adductors and decreased adductor strength and pain with resisted adduction. The diagnosis can be made with focal findings on examination using the guidelines from the Doha agreement classification system | First of all, there needs to be a patient history and an identification of the pain by the examination of the physiotherapist. On evaluation, there is tenderness to palpation with focal swelling of the adductors and decreased adductor strength and pain with resisted adduction. The diagnosis can be made with focal findings on examination using the guidelines from the Doha agreement classification system without the need for imaging. <ref name=":2" /><ref>Branci S, Thorborg K, Nielsen MB, Hölmich P. [https://bjsm.bmj.com/content/47/10/611.short Radiological findings in symphyseal and adductor-related groin pain in athletes: a critical review of the literature.] British journal of sports medicine. 2013 Jul 1;47(10):611-9.</ref> However, imaging can be useful to rule out or in differential diagnosis after a comprehensive clinical examination. Abnormal radiological findings around the pubic symphysis such as pubic bone marrow oedema are common of athletes with adductor and pubic related pain. These radiological findings are also common in the asymptomatic athletes. Radiological findings alone should not be used in making diagnostic decisions as morphology does not necessarily mean pathology. <ref>Branci S, Thorborg K, Bech BH, Boesen M, Nielsen MB, Hölmich P. [https://bjsm.bmj.com/content/49/10/681.short MRI findings in soccer players with long-standing adductor-related groin pain and asymptomatic controls]. British journal of sports medicine. 2015 May</ref> | ||
== Outcome Measures == | == Outcome Measures == | ||
The Copenhagen hip and groin outcome score (HAGOS)[ | The Copenhagen hip and groin outcome score (HAGOS)<ref>Thorborg K, Hölmich P, Christensen R, Petersen J, Roos EM. T[https://bjsm.bmj.com/content/45/6/478.short he Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist]. British journal of sports medicine. 2011 May 1;45(6):478-91.</ref> | ||
== Examination == | == Examination == | ||
1) Bilateral evaluation of adductor muscle-related pain and strength: palpation at the adductor insertion at the pubic bone, adduction against resistance ([[Adductor Squeeze Test|squeeze tests]] in 0° and 45°), and passive stretching of the adductor muscles.[17] | 1) Bilateral evaluation of adductor muscle-related pain and strength: palpation at the adductor insertion at the pubic bone, adduction against resistance ([[Adductor Squeeze Test|squeeze tests]] in 0° and 45°), and passive stretching of the adductor muscles.[17] | ||
{{#ev:youtube|https://www.youtube.com/watch?v= | {{#ev:youtube|https://www.youtube.com/watch?v=GwxrgZ_XgOU|200}}[20] | ||
| Line 306: | Line 303: | ||
== Physiotherapy Management == | == Physiotherapy Management == | ||
The treatment of musculotendinous groin injuries is generally conservative. Surgical treatment in acute groin injuries is rarely indicated.<ref name="'Jarvinen'" />[9] | The treatment of musculotendinous groin injuries is generally conservative. Surgical treatment in acute groin injuries is rarely indicated.<ref name="'Jarvinen'">Järvinen M, Orava S, Kujala UM. [https://www.sciencedirect.com/science/article/abs/pii/S1060187297800330 Groin pain (adductor syndrome).] Operative Techniques in Sports Medicine. 1997;5(3):133-7.</ref>[9] | ||
In the treatment of muscle-tendon injuries, immobilization should be limited to as short a period as possible to avoid the harmful effects of immobilization including muscle atrophy and loss of function. Immediate rest after the injury should be used until a diagnosis is secured. | In the treatment of muscle-tendon injuries, immobilization should be limited to as short a period as possible to avoid the harmful effects of immobilization including muscle atrophy and loss of function. Immediate rest after the injury should be used until a diagnosis is secured. | ||
Revision as of 00:21, 13 November 2021
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (13/11/2021)
Original Editor - Els Van Haver
Top Contributors - Vidya Acharya, Astrid Lahousse, Geubels Kaat, Nele Kiekens, Mats Vandervelde, Prince Wilson, Kim Jackson, Admin, Laure Lievens, Wanda van Niekerk, Lucinda hampton, Joao Costa, Kai A. Sigel, Uchechukwu Chukwuemeka, 127.0.0.1, Leana Louw, George Prudden, Claire Knott, Rachael Lowe, Els Van Haver and Naomi O'Reilly
Introduction[edit | edit source]
Groin pain is a common injury with varied clinical presentations and diagnostic term which makes it a difficult injury to manage. In a systematic review on the treatment of a groin pain in athletes, more than 30 diagnostic terminologies were used to describe groin pain which add up to the complexity of groin injuries in athletes.[1]
In attempt to address the terminology challenge, a consensus meeting was held in Doha, Qatar during the first World Conference of Grain Pain in Athletes , in November 2014. A group of 24 experts from 14 different countries were invited to agree on a standard terminology, along with accompanying definitions. [2]
A classification system were groin pain was described in three main subheading was agreed on during the Doha agreement meeting;
- Defined clinical entities for groin pain:
- Adductor-related
- iliopsoas-related
- inguinal-related
- pubic-related groin pain
- Hip–related groin pain
- Other causes of groin pain in athletes
In this article, the focus will be on adductor-related groin pain/strain.
Definition/Description[edit | edit source]
An adductor-related groin pain/strain is an injury to the muscle-tendon unit that produces pain on palpation of the adductor tendons or its insertion on the pubic bone and pain in the adductor region on resistance testing of the adductors.[2] Groin muscle strains are encountered more frequently in ice hockey and soccer.[3]
These sports require a strong eccentric contraction of the adductor musculature during competition and practice.[4] The underlying injury is most often a muscle or tendon strain at the insertion of the tendon of the adductor muscle to the bone.[5] The adductor longus is most commonly injured.[6]
The difference between groin tendinopathy and strain are:
- First of all, strains are acute and tendinosis is chronic. Tendinosis is a repetitive strain.
- The second difference is that acute injuries are more often localized in the myotendon junctions and chronic injuries are localized at the tendinous insertions on the pubic bone.
See page for adductor tendinitis.
Clinically Relevant Anatomy[edit | edit source]
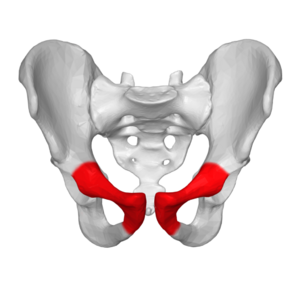
In human anatomy, the groin is the junctional area between the abdomen and the thigh on either side of the pubic bone. This is also known as the medial compartment of the thigh.
The groin muscles consist of three large groups of muscles that can be injured: the abdominal, iliopsoas and adductor group.
Image: Anterior view pelvis, pubic bone in red
- The adductor group: The adductors of the hip joint include 6 muscles: the adductor longus, magnus and brevis, gracilis, obturator externus, and pectineus. All these are innervated by the obturator nerve, with the exception of the pectineus, which receives innervation from the femoral nerve. The adductors all originate on the pubic ramus as almost all insert on the linea aspera of the posterior femur. The posterior head of the adductor magnus has a proximal attachment on the ischial tuberosity anteroinferiorly and attaches distally on the medial distal femur at the adductor tubercle. The gracilis insertion is on the medial border of the tuberosity of the tibia. The primary function of this muscle group is adduction of the thigh in open-chain motions and stabilization of the lower extremity and pelvis in closed chain motion.
In football, majority of groin injuries are adductor related. [8] The proximal attachment of the adductor longus contributes to an anatomical pathway across the anterior pubic symphysis that is likely required to withstand the transmission of large forces during multidirectional athletic activities. Its lack of mechanical advantage may make it more susceptible to strain.[9]
- The abdominal group: The abdominal musculature comprise the rectus abdominis, the obliques internus and externus abdominis. (See page for abdominal muscles).
- The iliopsoas group: The iliopsoas, comprised of iliacus and psoas major muscles, is the only muscle directly connecting the spine and the lower limb. (See page for hip anatomy).[4]
Epidemiology /Etiology[edit | edit source]
Groin strains are common amongst athletes who compete in sports that involve repetitive twisting, turning, sprinting and kicking such as football, ice hokey, Australian and Gaelic football.[3] Groin injuries are reported more in male compared to female football athletes. Injuries in men accounted for 4–19% of all injuries and 2–14% in women.[10]
The exact incidence of groin muscle strains in most sports is unknown because athletes often play through minor groin pain and the injury goes unreported. In addition, overlapping diagnoses can skew the incidence.[11] Cumulative or single injury seem to be important etiological factors. Chronic tendinitis of the adductor muscles/tendons, especially that of the adductor longus, is the most frequently diagnosed.[6]
Injury mechanism can be divided into 3 groups:
- Direct blunt trauma: An acute injury, typically a direct injury to the soft tissues resulting in muscle hematoma.
- Forceful contraction: The most common groin injury in athletes is muscle and tendon strain of the adductor muscle group. Change of direction and kicking have been described as the main actions resulting in adductor longus injury. Videos analysis of acute adductor longus [12] injuries in 17 professional male football players showed most injuries occurred in non-contact situations (71%), following a quick reaction to a change in play (53%). Injury actions were: change of direction (35%), kicking (29%), reaching (24%) and jumping (12%). Change of direction and reaching injuries were categorised as closed chain movements (59%), characterised by hip extension and abduction with external rotation. Kicking and jumping injuries were categorised as an open chain (41%), characterised by a change from hip extension to hip flexion, and hip abduction to adduction, with external rotation. So a rapid muscle activation during a rapid muscle lengthening appears to be the fundamental injury mechanism for acute adductor longus injuries. The adductors attempt to decelerate an extending, abducting leg by using an eccentric contraction to adduct and flex the hip was the main cause of injury. The injury may also occur during a forceful concentric contraction of the muscle.[13] Lower-extremity athletes such as ice hockey and soccer players are naturally more prone to this pathology due to the repetitive twisting, turning, sprinting and kicking.[3]
- Microtrauma by repetitive injury: musculotendinous injuries to the groin are mainly a consequence of cumulative microtraumas (overuse trauma, repeated minor injuries) leading to chronic groin pain.
And subsequently result in muscle contusions, avulsions, tears and strains.
Characteristics/Clinical Presentation[edit | edit source]
The main sign of the adductor-related groin injury is intense pain in the groin area. Muscle strain injuries often arise from excessive stretching or stretching when the muscle is being activated. When there is a strain in the muscle, the damage is often localized near the muscle-tendon junction. Acute adductor longus injuries may also involve tendinous rupture/ avulsion, primarily at the proximal insertions. [14]
Clinically for an adductor strain, the patient presents with pain in the inner thigh and tenderness along the muscle belly, tendon or insertion. The pain is exacerbated by adduction.[16]. Tears frequently occur at the myotendinous junction, which is the weakest part of the muscle-tendon unit but is also commonly seen in the muscle belly. The same mechanism of injury that results in a muscle tear in an adult may cause an apophyseal avulsion in an adolescent. There is a well-established clinical grading system for muscle tears, which has 3 components:[15]
- Grade 1: no loss of function or strength. Muscle tears can show normal appearances or a small area of focal disruption (<5% of the muscle volume), with hematoma and perifascial fluid relatively common on imaging with US and MRI.
- Grade 2: severe, with some weakness. Injury corresponds to a partial tear, with muscle fibre disruption seen (>5% of the muscle volume) but not affecting the whole muscle belly. In acute grade 1 or 2 strains of the adductor muscle, there is intense pain in the groin area, like a sudden stab with a knife, if the athlete attempts to continue the activity. Locally a haemorrhage and swelling can be seen a few days after the injury. A typical trauma history, localized tenderness and difficulties to contract the hip abductors.
- Grade 3: complete muscle tear and complete functional loss. Injuries are complete muscle tears with frayed margins and bunching and/or retraction of the torn muscle fibres. Complete muscle tears or grade 3 strains are most often found in the distal musculotendinous junction located toward the insertion on the femur.
Differential Diagnosis[edit | edit source]
Traditionally, groin pain has thought to be complex with various definition and no diagnostic criteria [8] until the recently. The Doha agreement meeting on groin pain has provided a classification system for the definition and diagnosis of the various causes of groin pain [doha]. The table below presents the
| Defined Entities. | Other musculoskeletal causes. | Not to be missed. |
|---|---|---|
|
|
Stress fracture
Inguinal lymphadenopathy Intra-abdominal abnormality
Gynaecological conditions Spondyloarthropathies
|
Diagnostic Procedures[edit | edit source]
First of all, there needs to be a patient history and an identification of the pain by the examination of the physiotherapist. On evaluation, there is tenderness to palpation with focal swelling of the adductors and decreased adductor strength and pain with resisted adduction. The diagnosis can be made with focal findings on examination using the guidelines from the Doha agreement classification system without the need for imaging. [2][16] However, imaging can be useful to rule out or in differential diagnosis after a comprehensive clinical examination. Abnormal radiological findings around the pubic symphysis such as pubic bone marrow oedema are common of athletes with adductor and pubic related pain. These radiological findings are also common in the asymptomatic athletes. Radiological findings alone should not be used in making diagnostic decisions as morphology does not necessarily mean pathology. [17]
Outcome Measures[edit | edit source]
The Copenhagen hip and groin outcome score (HAGOS)[18]
Examination[edit | edit source]
1) Bilateral evaluation of adductor muscle-related pain and strength: palpation at the adductor insertion at the pubic bone, adduction against resistance (squeeze tests in 0° and 45°), and passive stretching of the adductor muscles.[17]
[20]
A complete clinical examination should be performed for every patient with groin pain. The injured athlete should first be examined by inspection in a standing position to evaluate the alignment of extremities. The patient should then be asked to lie in a supine position in order to be able to check the motion of the hip joint and the flexibility of the groin and hip muscles. The diagnosis classification system provided by the Doha agreement should be used as a guideline to all groin injuries assessing the injury and classifying it into 1 of the 4 clinical entities. [doha]
Squeeze Test[edit | edit source]
- If adductor longus muscle is injured pain will be elucidated to the injured area by resisting leg adduction and in passive stretching at full abduction of the hip. Tenderness on palpation is localized to the injury site at the origin of the adductor longus tendon or at the musculotendinous junction.[doha]
- Evaluation of iliopsoas muscle-related pain, strength and flexibility: palpation above the inguinal ligament, isometric strength test in hip flexion and a modified Thomas test.[17] Thomas Test
- Abdominal muscle-related pain and strength: palpation of the abdominal muscle insertion at the pubic bone and a functional sit-up test and symphysis joint tenderness at palpation.[17]
- The location of the injury was based on a minimum of 1 positive finding on palpation, stretching, or muscle resistance testing[22]
Medical Management[edit | edit source]
Management is non-operative with rest, ice, compression, and gentle physical therapy or ROM. Patient with persistent symptoms even after conservative treatment may consider surgery. Surgery may be to tension structures around the groin, or to detention these structures. Detensioning interventions include adductor tenotomy, rectus aponeurosis tenotomy and inguinal ligament release.20 21.
Patients may return to sports or other activities after regaining full strength and ROM with the resolution of the pain.[20] Non-operative therapy should be tried for several months and is successful in most instances. However, if symptoms persist for more than 6 months after an appropriately administered physical therapy regimen and a period of protected weight bearing with crutches until the patient is pain-free, then surgical intervention should be considered. Adductor tenotomy has been suggested as a technique to improve symptoms. However, this is an end-stage option to be tried only after all conservative methods have failed.[21]
Prevention[edit | edit source]
Subsequent groin strains may occur, resulting in a recurrent problem. Hence primary and secondary prevention is equally important. To identify the athlete at risk and possibly correct the predisposing factor(s), the intrinsic and extrinsic risk factors for the injury type must be known.[7]
Previous groin injuries, reduced function scores, age, findings on clinical examination, and low isometric groin strength are associated with increased risk of new groin injuries. A history of a previous acute groin injury and weak adductor muscles are significant risk factors[7]. Previously injured players have more than twice as high a risk of sustaining a new groin injury, while players with weak adductor muscles have 4 times higher injury risk. Therefore it is important to have adequate rehabilitation before a full return to play. Preventing the first injury should be a high priority to keep players from entering the vicious cycle of recurrent injuries to the same body part. To accomplish this, the best method may be strength exercises of the adductors. Hölmich et al demonstrated that an 8 to 12-week active strengthening program, consisting of progressive resistive adduction and abduction exercises, balance training, abdominal strengthening and skating movements on a slide board, was effective in treating chronic groin strains.[7] Also coordination exercises (focused on the muscles related to the pelvis), core stability and eccentric exercises are a part of the prevention program.[24] Heat retainers and stretching of the adductors are also suggested to prevent injuries.[17]. Whereas a passive physical therapy program of massage, stretching, and modalities were ineffective in treating chronic groin strains.[5]
Adductor strain injury prevention program[11][25]
| Warm-up | Bike |
| Adductor stretching | |
| Sumo squats | |
| Side lunges | |
| Kneeling pelvic tilts | |
| Strengthening program | Ball squeezes (legs bent to legs straight) |
| Different ball sizes | |
| Concentric adduction with weight against gravity | |
| Adduction in standing on cable column or elastic resistance | |
| Seated adduction machine | |
| Standing with involved foot on sliding board moving in sagittal plane | |
| Bilateral adduction on sliding board moving in frontal plane (ie, simultaneous bilateral adduction) | |
| Unilateral lunges with reciprocal arm movements | |
| Sports-specific training | On ice kneeling adductor pull togethers |
| Standing resisted stride lengths on cable column to simulate skating | |
| Slide skating | |
| Cable column crossover pulls | |
| Clinical goal | Adduction strength at least 80% of the abduction strength |
Copenhagen Adductor Exercise
In a cluster-randomised controlled trial involving 35 semiprofessional Norwegian football teams, using a simple adductor strengthening exercise (Copenhagen Adductor Exercise ) with three progression levels, three times per week during the preseason (6-8 weeks), and once per week during the competitive season (28 weeks). There was significant reduction in the risk of groin problems compared to the controlled group who trained as normal during the season. The intervention group was made up of 18 teams, 339 players and controlled group 17 teams, 313 players. The prevalence of groin problems was measured weekly in both groups during the competitive season using the Oslo Sports Trauma Research Center Overuse Injury Questionnaire. [32]
Physiotherapy Management[edit | edit source]
The treatment of musculotendinous groin injuries is generally conservative. Surgical treatment in acute groin injuries is rarely indicated.[22][9]
In the treatment of muscle-tendon injuries, immobilization should be limited to as short a period as possible to avoid the harmful effects of immobilization including muscle atrophy and loss of function. Immediate rest after the injury should be used until a diagnosis is secured.
- The primary goal of the treatment program is to minimize the effects of immobilization, regain full range of motion, and restore full muscle strength, endurance and coordination. Therefore, crutches, local cold application, and anti-inflammatory medication are recommended in the initial phase. Muscle exercises can usually be started early, but training should be performed within the limits of pain with careful isometric contractions against resistance.
- After the initial phase, heat is usually valuable, especially when muscle training is started. In general, exercises are performed in a pain-free range of motion and increased pain should not occur after activity.
- As rehabilitation progresses, mild pain can be allowed during exercise, but it should subside immediately after the cessation of training.
- When full range of motion is accomplished, the injured muscle and tendon tolerates higher loads and the goal of rehabilitation should shift towards specific strength training exercises aiming for muscular recovery, increased endurance and a full range of motion.
- The final step is the gradual return to sports activity, which may in some cases take as long as 3 to 6 months.[13][11]
Adductor muscle strain injury program[11]: [25]
| Phase 1: Acute | First 48 hours after injury: RICE (rest, ice, compression, elevation) |
| Nonsteroidal anti-inflammatory drugs | |
| Massage | |
| Transcutaneous electrical nerve stimulation | |
| Ultrasound | |
| Submaximal isometric adduction with knees bent → with knees straight progressing to maximal isometric adduction, pain free | |
| Hip passive range of motion in pain-free range | |
| Non-weightbearing hip progressive resistance exercises without weight in antigravity position (all except abduction): pain free, low load, high repetition | |
| Upper body and trunk strengthening | |
| Contralateral lower extremity strengthening | |
| Flexibility program for noninvolved muscles | |
| Bilateral balance board | |
| Clinical milestone | Concentric adduction against gravity without pain |
| Phase 2: Subacute | Bicycling/swimming |
| Sumo squats | |
| Single-limb stance | |
| Concentric adduction with weight against gravity | |
| Standing with involved foot on sliding board moving in frontal plane | |
| Adduction in standing on cable column or resistance band | |
| Seated adduction machine | |
| Bilateral adduction on sliding board moving in frontal plane (ie, simultaneous bilateral adduction) | |
| Unilateral lunges (sagittal) with reciprocal arm movements | |
| Multiplane trunk tilting | |
| Balance board squats with throwbacks | |
| General flexibility program | |
| Clinical milestone | Lower extremity passive range of motion equal to that of the uninvolved side and involved adductor strength at least 75% that of the ipsilateral abductors |
| Phase 3: Sports-specific training | Phase II exercises with increase in load, intensity, speed and volume |
| Standing resisted stride lengths on cable column to simulate skating | |
| Slide board | |
| On ice kneeling adductor pull togethers | |
| Lunges (in all planes) | |
| Correct or modify ice skating technique | |
| Clinical milestone | Adduction strength at least 90-100% of the abduction strength and involved muscle strength equal to that of the contralateral side |
Progressing the patient through the phases of healing has been developed by Tyler et al. and anecdotally seems to be effective (table 1). This type of treatment and rehabilitation programme, which combines modalities and passive treatment immediately, followed by an active training programme emphasising eccentric resistive exercise, has been supported throughout the literature.[21][23]
The recently published study suggests that modified Hölmich protocol may be safer and more effective than the Hölmich protocol in athletes with longstanding adductor groin pain in promoting their return to sports activity. Hölmich et al. (1999) showed that therapeutic exercise (concentrated on hip and abdominal muscle strengthening) compared with physiotherapy including passive agents (stretching, TENS, transverse friction massage, and laser therapy) leads to better results in terms of reducing pain and returning to sports activity. The modified Hölmich protocol ten-week protocol that benefits from strengthening the muscles affecting the pelvis, core stabilization, hip adductor stretching and high-intensity eccentric exercise of the hip adductors may have a considerable effect on primary measured outcomes including pain, hip adductor and abductor muscle strength, hip ROM, functional ability, and returning to the sport.[23]
Stretching Exercises[edit | edit source]
Strengthening Exercises[edit | edit source]
Hip Adductors[edit | edit source]
- Side-lying hip-adduction and ball-squeeze exercises display the highest overall activation of adductor longus muscle.[25]
| [26] | [27] |
- Resisted training:
Resisted work with weights or elastic bands.
- Eccentric exercises:[29][31]
A simple adduction strengthening programme based on Copenhagen Adduction Exercise reduced the risk of a groin problem in footballer players according to the study published in the British Journal of Sports Medicine.[30][32]
- Squats:
Squats can help in strengthening hip and knee muscles including the adductors. Greater stance width in the squat and deadlift, and squeezing a medicine ball between the legs in the leg press may increase adductor longus muscle activity,The research shows that squats performed at 30° of hip external rotation and at least 90° of knee flexion significantly increased the activity of hip adductors.[31] [33]
Hip Abductors[edit | edit source]
Strengthening the hip abductors along with hip adductors is important as decreased strength in the hip abductors (gluteus medius) has been found in athletes who sustained a groin injury due to reduced activity.[33] [35]Ensuring that hip abductor strength training is included in the rehabilitation programme is another key factor in groin injury prevention.[34][36][35][37]
Conclusion[edit | edit source]
There is support for an association of precious injury and greater abductor to adductor strength ratios as well as sport specificity of training and pre-season sport-specific training, as individual risk factors for groin strain injury in athletes.[33] [35]Core muscle weakness or delayed onset of transversus abdominal muscle recruitment may increase the risk of groin strain injury. Debate does exist in the literature reviewed regarding the role of adductor strength and length as well as age and/or sport experience as risk factors for groin injury.[37][39]
References[edit | edit source]
- ↑ Serner A, van Eijck CH, Beumer BR, Hölmich P, Weir A, de Vos RJ. Study quality on groin injury management remains low: a systematic review on treatment of groin pain in athletes. British journal of sports medicine. 2015 Jun 1;49(12):813-.
- ↑ 2.0 2.1 2.2 2.3 Weir A, Brukner P, Delahunt E, Ekstrand J, Griffin D, Khan KM, Lovell G, Meyers WC, Muschaweck U, Orchard J, Paajanen H. Doha agreement meeting on terminology and definitions in groin pain in athletes. British journal of sports medicine. 2015 Jun 1;49(12):768-74.
- ↑ 3.0 3.1 3.2 Orchard JW. Men at higher risk of groin injuries in elite team sports: a systematic review. British journal of sports medicine. 2015 Jun 1;49(12):798-802.
- ↑ 4.0 4.1 Tyler TF, Fukunaga T, Gellert J. Rehabilitation of soft tissue injuries of the hip and pelvis. International journal of sports physical therapy 2014;9(6):785.
- ↑ Kerkhoffs GM, Servien E, editors. Acute muscle injuries. Springer International Publishing; 2014.
- ↑ 6.0 6.1 Kiel J, Kaiser K. Adductor Strain. StatPearls Publishing, Treasure Island; 2018.
- ↑ AnatomyZone Muscles of the Thigh Part 2 - Medial Compartment - Anatomy Tutorial Available from https://www.youtube.com/watch?time_continue=10&v=MjPAPTJdxa8
- ↑ Hölmich P, Thorborg K, Dehlendorff C, Krogsgaard K, Gluud C. Incidence and clinical presentation of groin injuries in sub-elite male soccer. British journal of sports medicine. 2014 Aug 1;48(16):1245-50.
- ↑ Norton‐old KJ, Schache AG, Barker PJ, Clark RA, Harrison SM, Briggs CA. Anatomical and mechanical relationship between the proximal attachment of adductor longus and the distal rectus sheath. Clinical Anatomy 2013;26(4):522-30.
- ↑ Waldén M, Hägglund M, Ekstrand J. The epidemiology of groin injury in senior football: a systematic review of prospective studies. British journal of sports medicine. 2015 Jun 1;49(12):792-7.
- ↑ 11.0 11.1 11.2 Tyler TF, Silvers HJ, Gerhardt MB, Nicholas SJ. Groin injuries in sports medicine. Sports health 2010;2(3):231-6.
- ↑ Serner A, Mosler AB, Tol JL, Bahr R, Weir A. Mechanisms of acute adductor longus injuries in male football players: a systematic visual video analysis. British journal of sports medicine. 2019 Feb 1;53(3):158-64.
- ↑ 13.0 13.1 McSweeney SE, Naraghi A, Salonen D, Theodoropoulos J, White LM. Hip and groin pain in the professional athlete. Canadian Association of Radiologists Journal 2012;63(2):87-99.
- ↑ Serner A, Weir A, Tol JL, Thorborg K, Roemer F, Guermazi A, Yamashiro E, Hölmich P. Characteristics of acute groin injuries in the adductor muscles: a detailed MRI study in athletes. Scandinavian journal of medicine & science in sports. 2018 Feb;28(2):667-76.
- ↑ Davies AG, Clarke AW, Gilmore J, Wotherspoon M, Connell DA. imaging of groin pain in the athlete. Skeletal radiology. 2010 Jul;39(7):629-44.
- ↑ Branci S, Thorborg K, Nielsen MB, Hölmich P. Radiological findings in symphyseal and adductor-related groin pain in athletes: a critical review of the literature. British journal of sports medicine. 2013 Jul 1;47(10):611-9.
- ↑ Branci S, Thorborg K, Bech BH, Boesen M, Nielsen MB, Hölmich P. MRI findings in soccer players with long-standing adductor-related groin pain and asymptomatic controls. British journal of sports medicine. 2015 May
- ↑ Thorborg K, Hölmich P, Christensen R, Petersen J, Roos EM. The Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist. British journal of sports medicine. 2011 May 1;45(6):478-91.
- ↑ British Journal of Sports Medicine (BJSM) 10 Squeeze test.Available from https://www.youtube.com/watch?time_continue=65&v=--W5G9lP7pM
- ↑ Tibor, Lisa M., and Jon K. Sekiya. "Differential diagnosis of pain around the hip joint." Arthroscopy: The Journal of Arthroscopic & Related Surgery 24.12 (2008): 1407-1421. Evidence Based Practise: 1A
- ↑ 21.0 21.1 Nicholas SJ, Tyler TF. Adductor muscle strains in sport. Sports Medicine 2002;32(5):339-44.
- ↑ Järvinen M, Orava S, Kujala UM. Groin pain (adductor syndrome). Operative Techniques in Sports Medicine. 1997;5(3):133-7.
- ↑ Yousefzadeh A, Shadmehr A, Olyaei GR, Naseri N, Khazaeipour Z. The Effect of Therapeutic Exercise on Long-Standing Adductor-Related Groin Pain in Athletes: Modified Hölmich Protocol. Rehabilitation research and practice 2018;1-10.
- ↑ The Prehab Guys. 3 Exercises to Prehab your Adductor Strain / Groin Pain. Available from https://www.youtube.com/watch?v=f2e_oi2FbPM
- ↑ Delmore RJ, Laudner KG, Torry MR. Adductor longus activation during common hip exercises. Journal of sport rehabilitation 2014;23(2):79-87.
- ↑ Natalie Wetzel.Adductor isometric exercise. Available from https://www.youtube.com/watch?time_continue=6&v=bmjGd7z7fHc
- ↑ Jason Craig Hip Adductor Strengthening in Side Lying. Available from https://www.youtube.com/watch?v=bP9W4-vgSgA
- ↑ Upright Health An exercise to safely strengthen your adductors.Available from https://www.youtube.com/watch?time_continue=4&v=jn22rqsaeV8
- ↑ Jensen J, Hölmich P, Bandholm T, Zebis MK, Andersen LL, Thorborg K. Eccentric strengthening effect of hip-adductor training with elastic bands in soccer players: a randomised controlled trial. British Journal of Sports Medicine 2014;48(4):332-8.
- ↑ Harøy J, Clarsen B, Wiger EG, Øyen MG, Serner A, Thorborg K, Hölmich P, Andersen TE, Bahr R. The adductor strengthening programme prevents groin problems among male football players: a cluster-randomised controlled trial. British journal of sports medicine 2019;53(3):150-7.
- ↑ Pereira GR, Leporace G, das Virgens Chagas D, Furtado LF, Praxedes J, Batista LA. Influence of hip external rotation on hip adductor and rectus femoris myoelectric activity during a dynamic parallel squat. The Journal of Strength & Conditioning Research 2010;24(10):2749-54.
- ↑ 2Fitathome.com Sumo Squats: Works your inner thighs, quads and glutes! Multiple Fitness Level Tutorial. Available from https://www.youtube.com/watch?v=MSC4X5k1QC4
- ↑ 33.0 33.1 Niemuth PE, Johnson RJ, Myers MJ, Thieman TJ. Hip muscle weakness and overuse injuries in recreational runners. Clinical Journal of Sport Medicine 2005;15(1):14-21.
- ↑ Krommes K, Bandholm T, Jakobsen MD, Andersen LL, Serner A, Hölmich P, Thorborg K. Dynamic hip adduction, abduction and abdominal exercises from the Holmich groin-injury prevention program are intense enough to be considered strengthening exercises–a cross-sectional study. International journal of sports physical therapy 2017;12(3):371.
- ↑ Kloskowska P, Morrissey D, Small C, Malliaras P, Barton C. Movement patterns and muscular function before and after onset of sports-related groin pain: a systematic review with meta-analysis. Sports Medicine 2016;46(12):1847-67.
- ↑ eHowFitness How to Do Thigh Abduction & Adduction Exercises With Bands : Stretching & Exercise. Available from https://www.youtube.com/watch?time_continue=6&v=HE-8qeIZo3o
- ↑ Maffey L, Emery C. What are the risk factors for groin strain injury in sport? Sports Medicine. 2007;37(10):881-94.