Gluteal Tendinopathy: Difference between revisions
m (isometric hip abd video clips added) |
No edit summary |
||
| Line 131: | Line 131: | ||
|- | |- | ||
| {{#ev:youtube|b2YAUfZITl0|350}}<ref>Physiohealth01: Isometric Hip Hitching. Available from: https://www.youtube.com/watch?v=b2YAUfZITl0[last accessed 03/04/2020]</ref> | | {{#ev:youtube|b2YAUfZITl0|350}}<ref>Physiohealth01: Isometric Hip Hitching. Available from: https://www.youtube.com/watch?v=b2YAUfZITl0[last accessed 03/04/2020]</ref> | ||
| {{#ev:youtube| | | {{#ev:youtube|aPbiOoNz2Ws|350}}<ref>NHS Ayrshire & Arran: Hip Isometric Hip Abduction In Standing. Available from: https://www.youtube.com/watch?v=aPbiOoNz2Ws[last accessed 03/04/2020]</ref> | ||
|} | |} | ||
Revision as of 13:03, 3 April 2020
Top Contributors - Mariam Hashem, Wendy Snyders, Tarina van der Stockt, Kim Jackson, Admin, Kai A. Sigel, Hannah Hassell, Simisola Ajeyalemi, Wanda van Niekerk, Robin Tacchetti, Rishika Babburu, Tony Lowe, Uchechukwu Chukwuemeka and Lucinda hampton
Page Owner - Wendy Snyders as part of the One Page Project
Introduction[edit | edit source]
Gluteal Tendinopathy (GT) is defined as moderate to severe disabling pain over the Greater Trochanter (lateral hip pain) with marked palpation tenderness over the greater trochanter[1]. The pain can at times prefer into the lateral thigh[2]. It is often referred to as Greater Trochanter Pain Syndrome (GTPS) and was traditionally diagnosed as Trochanteric Bursitis, however, recent research defines non-inflammatory tendinopathy of the gluteus medius(GMed) and/or gluteus minimus (GMin) muscles to be the main source of lateral hip pain[3].
This condition generally affects inactive people but can also be a problem in athletes, especially runners[3]. It is the most common tendinopathy in the lower limb[4][3] with one in four females over 50 years likely to be affected[5]. It is more common in females and outnumbers men 2.4 - 4: 1[6].
GT has significant impacts on the quality of life, with similar symptoms to those of hip OA and interferes with sleep (side lying) and common weight bearing tasks[3][1] Sadly, there is no optimal treatment approach for this condition[1].
Pathoanatomy/Pathomechanics[edit | edit source]
Tendon structure and loading capacity are influenced by mechanical loading which triggers physiological responses within the tendon. Under normal conditions, the tendon undergoes a cycle of balanced catabolic and anabolic processes[3]. Changes in loading type, intensity or frequency disrupt this harmony. Eccentric contractions in outer ranges (when the muscle is active and the tendon is lengthening simultaneously) and where potential compression can occur, represent the greatest form of loading[3]. Failure to adapt to loading, due to rapid increase in intensity and/or frequency with insufficient recovery time, results in a series of catabolic effects which in turn result in altering tenocyte behaviour, reducing load-bearing capacity and predisposing tendons to injury at relatively low tensile loads. A combination of both tensile loading and compression are found to be the most damaging[7].
GMed and GMin tendons are subjected to compression due to several factors:
1. Joint position
The Iliotibial Band (ITB) causes a compressive force on gluteal tendons that magnifies as the hip moves into further adduction[8]. Birnbaum et al. reported a change from 4N to 106N ITB compression as the angle of hip adduction increased from 0 to 40 degrees[9]. Based on this, adopting constant or repetitive hip adduction during static and dynamic tasks possibly contributes to the development of GT.
ITB tension also exerts loads on the GMed and GMin tendons at higher degrees of flexion through the fascial confluence of the ITB with the gluteal fascia[8]. This suggests that combining adduction and flexion, such as in sitting with knees crossed or adducted in a low chair, can cause pronounced compression on the GMed tendon[8]. People with GT may also experience pain after sitting for an extended period of time, especially if their hips were flexed above 90 degrees[8].
Examples of activities and positions that cause compression at the gluteal tendons[8]:
- standing with one hip in adduction
- sitting with knees together
- sitting with knees crossed in adduction
- excessive lateral pelvic tilt or shift during dynamic single leg loading tasks.
- running on a cambered road or in the same direction on an athletics track with a midline or cross-midline foot-ground contact pattern
2. Muscle Force
Kummer (1993) found that pelvic control in a single leg stance position was controlled 70% by the abductor muscles and that the ITB tensioners (GMax, TFL and vastus lateralis) then accounted for the remaining 30%[3]. This is seen as the abductor mechanism. It has also been shown that people with gluteal tendinopathy tend to have GMed and GMin atrophy and TFL hypertrophy. Weakness and/or muscle bulk changes impact the balance of the abductor mechanism and increase the compression of the gluteal tendons[3].
3. Bony Factors
A biomechanical study using cadaveric modelling showed increased compressive force associated with reduced femoral neck-shaft angle[10][3]. Another study related the severity of GT to lower femoral neck-shaft angle compared with pain-free subjects with hip OA[11]. Lower neck-shaft angle is likely to contribute to greater offset (the difference between the width of the iliac wings and that of the greater trochanters). All these bony factors are suggested to influence ITB compression against gluteal tendons[3].
It is postulated that women are more prone to GTPS because of pelvic biomechanics, different activity levels in the population and hormonal effects[12]. One study found that females have a smaller insertion of the GMed tendon, resulting in a smaller area across which tensile load could be dissipated. It also makes the moment arm shorter, causing reduced mechanical effeciency[6].
Clinical Presentation[edit | edit source]
Lateral hip pain with an insidious onset, that gradually worsens overtime[3] with different loads and tasks[13] is the main feature of GT. Other symptoms include:
- Tender lateral hip when palpated, especially near the greater trochanter[12][6]
- Pain with side-lying on the problematic side[6][12][14]. Pain at night when lying on the painful side is the hallmark sign for GT[15].
- Pain with weight-bearing activities such as walking, climbing stairs, standing and running[6][12][14]
- Pain may refer to the lateral thigh and knee[6][12]
- Pain with prolonged sitting[3]
- Sitting with crossed legs increases pain[3]
- Pain can also occur when lying on the non-painful side if the painful hip falls into adduction
- Weak hip abductors[3]
Fearon et al. (2012) proposed that being able to manipulate socks and shoes without pain differentiates GTPS (or gluteal tendinopathy) from hip osteoarthritis (OA)[16]
Diagnostic Procedures[edit | edit source]
A thorough hip examination is needed basically by obtaining patient's history to understand the nature of the symptoms and rule out Red Flags. Then the assessor should go into the physical exam with a hypothesis that to be confirmed with clinical tests. The tests below, although they have weak diagnostic properties, are commonly used in musculoskeletal settings to confirm GT diagnosis. Their diagnostic accuracy can be improved when the patient is able to report the site of symptoms during testing[6].
- FABER test: Flexion/Abduction/External Rotation. Tension in this test is specific to the anterior portions of the GMed and GMin. The test is positive when pain is experienced over the lateral hip. It assists with differentiating between hip OA and GTPS[16].
- (30 second) single leg stance test: The person being tested must stand, unassisted, on one leg with their eyes open and one finger on a wall. As soon as the person’s foot is lifted of the floor, the 30 seconds start. This test has been shown to have a specificity of 100%, sensitivity of 38% and positive predictive value of 100%, indicating that if the test was positive there was an extremely high likelihood that GT was present on MRI[17].Grimaldi and Fearon (2015) suggest holding the position for 30 seconds or until reproduction of symptoms[6].
- Resisted external de-rotation test and modified external de-rotation test:The patient lies in supine and the examiner then passively flexes the hip to 90° with external rotation. The hip should be in neutral abduction/adduction. Slightly reduce the external rotation to decrease the compression of the tendon. The patient then actively rotates their leg to neutral against the therapist’s resistance. The modified test is exactly the same, but done in full hip adduction[18].
- Hip FADER: (FADER=Flexion/Adduction/External Rotation)[17][19]. The therapist passively takes the limb into 90° hip flexion, adduction and external rotation to end of range. This test aims to position the ITB over the greater trochanter, and positions the GMed and GMin tendons under tension with the ITB fascia against the greater trochanter. Test is positive if the patient experienced pain (≥2/10) on the Numeric Rating Scale (NRS) over the lateral hip. The reported specificity and positive predictive value (PPV) of this test are 86.67% and 88.24% respectively when compared with an MRI imaging[20].
- Hip FADER-R: Flexion/Adduction/External Rotation with static resisted internal rotation of the hip. Grimaldi et al. (2014) found this test to have a sensitivity of 0.48 and a specificity of 0.86[19]
- Passive end-of-range hip adduction in side lying (ADD) test[17]: In the side lying position, the lowermost hip and knee flexed 80-90°, and the uppermost leg supported by the examiner with the knee extended, in neutral rotation, and the femur in line with the trunk. The anterior superior iliac spines are aligned vertically in the frontal plane. The examiner passively moves the hip into end range hip adduction with overpressure, while maintaining the pelvis stable with the other hand. This test compresses the lateral insertions of the gluteal tendons, and a positive response is felt over the lateral hip. It has been found to have a very low sensitivity but a high specificity (0.79)[19]
- ADD with resisted isometric abduction (ADD-R)[17][19]: In the end range of the previous test position (ADD test), the participant is asked to push the thigh up, against the resistance of the examiner’s hand at the lateral knee. This further compresses the tendons with pain experienced over the lateral hip. Similar to the FADER test, adding manual resistance has been shown to improve the the sensitivity, specificity, PPV and negative predictive value (NPV) of both of this test.
- Palpation: Palpation has been shown to be most sensitive (0.83), but least specific (0.43) for clinically diagnosing GT[19]. Palpation should be done over the anterior, lateral or posterosuperior facets of the greater trochanter (GMed and GMin tendon insertions) bilaterally. The patient should assume a side-lying position with the asymptomatic side at the bottom, hips flexed 60°and knees together. A positive test indicates pain and tenderness.
- Resisted hip abduction: A systematic review by Reiman et al. (2012) found this test to have a 71% sensitivity and 84% specificity[21].
Pain provocation and reproduction of symptoms by loading abductors are the aims of these tests. Assessing active abduction in a position of hip adduction may be more useful. Further provocation can be elicited by testing the gluteal muscles internal rotation function at a 90 degree hip flexion and maximal external rotation[3]. The traditional Trendelenburg test is useful in diagnosing partial and complete abductor tendon[20][3] and is considered positive when a drop of the pelvis on the contralateral side of the stance leg is seen.
Pain on palpation of the structures over the greater trochanter is considered a cardinal sign in diagnosing Greater Trochanter Pain Syndrome. If the direct compression over this area failed to elicit pain, then GT may be excluded and other conditions would be considered[22]. The available literature has not yet provided a clear combination of diagnostic tests to confirm GT diagnosis. Further research is required to reach accurate and objective set of criteria and/or tests.
Cook and Purdam[23] suggest functional loading tests to assess and track a tendon's response to therapy. Reduced pain on single leg standing (low-load test) and hopping on the affected leg (high-load test) indicates improved loading tolerance of the gluteal tendons[23]. Inadequate eccentric pelvic control in single leg loading tasks indicates a greater hip adduction moment arm and possible gluteal tendons compression. Video analysis of is suggested for athletes to observe pelvic tilt and femoral adduction in running and changing direction[3].
The combination of several tests is advisable because one positive clinical test helps in confirming diagnosis but doesn't necessarily refute it.
Imaging is only suggested in the following situations:
- When it comes to diagnosing gluteal tears. Ultrasound or MRI should be used to confirm the diagnosis if suspected clinically[25][12]. Cook (2020) reports that ultrasound is the most accurate when assessing a tendon where MRI is helpful for differential diagnosis[26].
- When conservative treatment has failed[6][12]
- When diagnosis is unclear[6][12]
Outcome measure[edit | edit source]
The Victorian Institute of Sport Assessment-Gluteal tendon (VISA-G) can be used to assess and track pain intensity and functional limitation[27].
Differential Diagnosis[edit | edit source]
- Hip OA
- Avascular Necrosis
- Femoral-acetabular Impingement (FAI)
- Greater Trochanter Pain Syndrome
- Lumbar Radiculopathy
- Trochanteric Bursitis (not a stand alone diagnosis, but rather a consequence of gluteal tendinopathy)
- Fluorquinolone-induced tendinopathy[28][29][30]
Management Strategies[edit | edit source]
Management of GT includes[3]:
- load management strategies
- isometric exercises
- strengthening
- shockwave therapy
- corticosteroid injections
- platelet-rich plasma injections
- tenocyte injections
- surgery .
Please see the Tendon Rehabilitation page for more information.
Load Management[edit | edit source]
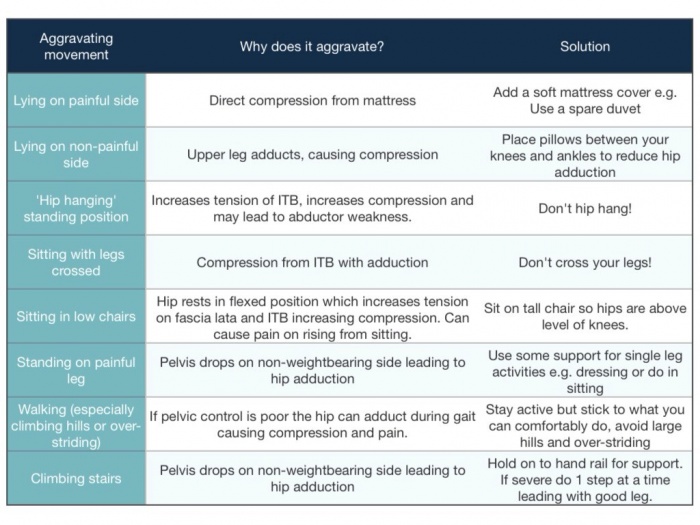
Loading management for GT should include education on positions and activities that can increase compressive load on the gluteal tendons. Patients with GT should:
- Avoid sitting with their legs crossed[6]
- Avoid sitting with knees together[6]
- Avoid standing while hanging on one hip[6]
- Avoid lying on the affected side[6]
- Place a pillow between their knees and shins when lying on the unaffected side to limit adduction of the affected hip[6]
- Stop adduction stretching (for glutes and ITB) to limit compression of the gluteal tendons[6]
Avoiding side-lying on the affected side or hip adduction when lying on the unaffected side will greatly help with reducing the common problem of night pain.
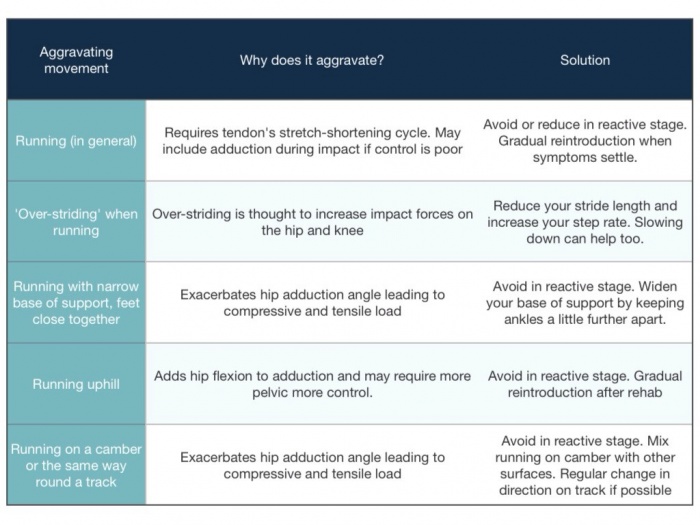
High tensile loads should be managed by teaching the patient not to rapidly increase activity. Sport and recreational activity volumes should be carefully monitored to prevent aggravation of pain. For the elderly, small changes like reducing walking distances, avoiding hills when walking and avoiding stairs may be sufficient in reducing the load on the gluteal tendons[6].
In athletes, complete rest is detrimental to tendon function. Training should be modified; activities combing high tensile and compressive loads should be avoided and quick changes in training should be restricted[3]. It is assumed that most tendinopathies that develop in season are due to a reactive response on an existing degenerative tendinopathy and based on this, removing high loads prevents further disruption of the matrix of the tendon if given enough time[23]. It is also important to progressively load the tendon to aid matrix remodeling[23].
An example of managing load would be to reduce training in the outer muscle range and in so doing reduce the compression on the tendon. This will allow the patient to then continue the existing tensile load as they will not be combining compressive and high tensile loads[23]. To reduce tensile loads, running over long distances, plyometric training and hill running should be stopped temporarily[6].
Very importantly, there are loads that can reduce pain in tendons. Sustained isometric contractions with a degree of load have been shown to activate the descending inhibitory pathways resulting in a mechanical analgesic effect in the tendon[23]. Isometric exercises will be discussed further in the exercise section below.
Isometric exercise[edit | edit source]
Isometric contractions are now commonly used as they release cortical inhibition targeting both peripheral and central pain drivers. This cortical inhibition causes immediate pain reduction and for 45 minutes afterwards[14]. Cook (2020) reported that the analgesic effect can last for 4 to 8 hours after isometrics[31]. Isometric contractions must be heavy to effectively achieve pain relief in the tendon[31][32]. The exact duration of the contraction is unknown, but 5 repetitions of 45 seconds has been found to be very effective[6][31][32]. A rest period of 2 minutes must occur between each of the isometric contractions[31].
| [33] | [34] |
Strengthening [edit | edit source]
Exercise should then progress to low velocity, high tensile loading to achieve gluteal tendons hypertrophy. Concentric-eccentric hip abductor exercises through mid to inner range of abduction allow for high tensile loading with minimal compression. Because this cannot be fully achieved in single-leg loading exercises, gradual and monitored progression are required with enough time between exercise sessions for recovery.
The overall hip abductors strength is not strongly correlated with hip adduction angle during functional tasks, therefore specific movement retraining in the frontal plane should be incorporated in GT management.
Feedback on reducing hip adduction moment during running can significantly reduce hip adduction and contralateral pelvic drop during running.
We should also identify associated mechanical dysfunctions in surrounding joints; lumbar, hip and knee and address them to correct the loading patterns on gluteal tendons.
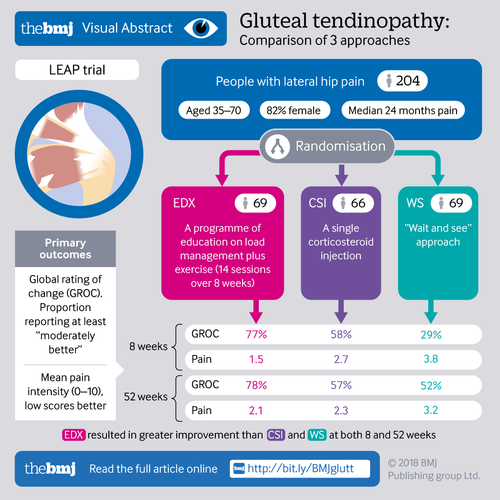
A randomised clinical trial by Mellor et al. compared the effectiveness of load management education plus exercise with corticosteroid injection and a ''wait-and see'' approach. Education and exercise resulted in 77.3% success rate on the global rating of change and hip pain intensity on both short and long terms[5].
The Mellor et al. study [5] also called the LEAP study, included education, load management and an exercise program. The participants received 14 physiotherapy sessions over 8 weeks and had to follow a daily exercise program that progressed the difficulty over 4-6 weeks to allow muscle strength and function improvement while limiting pain aggravation and was dependent on the response to loading. Motoring load appropriately is recommended by increasing load gradually without pain aggravation, particularly night pain. Slow and heavy loading similar to tendon rehab by cook, but it isn't an eccentric only approach. VAS during activity. Symptom response over next 24-48 hours and pain during tendon load tests. In this study they accepted 5/10 pain during the exercise as long as it decreased after the exercise and the patient had no increase in pain during the night or the next morning. Loading was increased depending on the response to the exercises.
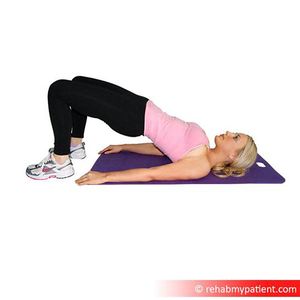
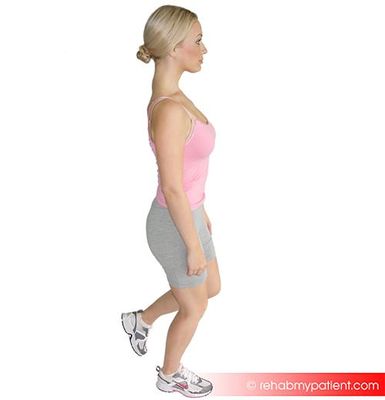
The home exercises (found here) in the LEAP study [5]focused on hip strengthening (mainly abductors), functional retraining and adduction control during functional tasks. Bridging variations, squatting and lunges were used for functional Loading progressions and pelvic control training. It is important to integrate functional exercises at different positions to optimize the motor control. To load abductors in frontal plane, subjects in exercise group performed different abduction exercises against spring resistance.
|
Summary of progression of exercises in the LEAP study[5]:
(">" means progression of previous exercise)
- Week 1-2
- Static abduction in supine against an elastic band (1-2 sets of 10 reps) and standing "imagine sliding your legs apart" (hold 5-10sec, 1 set of 3-5 reps) *Twice a day
- Double leg bridge > Offset bridge > Single foot hover bridge > Single leg extension bridge > Single leg bridge with dips (1 sets, 5 reps) *Daily
- Functional retraining: Double leg squats > Offset squats > Single leg standing > Single leg squats > Step ups (1 sets, 5 reps) *Daily
- Week 3-8
- Continue with week 1-2 static abduction exercises for low load activation as part of the warm up
- Continue with Double and single leg biased exercises (1-2 sets, 5-10 reps) *Daily
- Continue with Functional retraining: Double leg squats > Offset squats > Single leg standing > Single leg squats > Step ups (1-2 sets, 5-10 reps) *Daily
- Weight bearing abductor loading: Side stepping, Doorway side slides against elastic band (1-2 sets, 5-10 reps) *Daily
- Exercises supervised by physiotherapist in the clinic
- Abductor loading via frontal plane movement on an abductor slide against spring resistance with body upright > mini squat (1 set, 5-10 each way) *Twice a week
- Pelvic control during functional loading
This infographic summarizes the LEAP trial:
Following the LEAP study, Ganderton et al.[14] compared gluteal Loading to sham Exercises on pain and dysfunction in women with GTPS. the study found differences in symptoms but no significant differences in hip abductor muscle torque was found between the two groups. Although the study had several limitations regarding the utilised exercise program the psychological factors were highlighted. Pain and limitation severity were associated with higher pain catastrophising, pain self-efficacy and depression scores.
Fear and uncertainty are associated with Achilles[35] and gluteal tendinopathies[36]. Kinesiophobia is also a key factor influencing Achilles tendon recovery[37]. These findings support the need for utilising a bio-psychological management approach by addressing patients' concerns on returning to the basic level of activities, helping them identifying their barriers to recovery, exercise empathy, explaining tendinopathy in a positive way and knowing when to refer to other specialised healthcare professional[38].
| [39] | [40] |
Shockwave Therapy[edit | edit source]
A small study conducted in 2018 found that shockwave therapy was effective in providing short-term pain relief in chronic GTPS where gluteal tendinopathy was confirmed on MRI[41]. A systematic review published in 2014 found the following[42]
- Shockwave therapy is superior to interventions such as rest, non-steroidal anti-inflammatories and corticosteroid injections and stretching exercise when the aim is to reduce pain and improve function.
- It is more effective than exercise at home at 4 months
- It is more effective than corticosteroid injections in the long-term for pain relief
It is worth mentioning that the studies included in the above-mentioned review were old (published in 2009).
Corticosteroid injections[edit | edit source]
Corticosteroid injection is very effective for providing short-term pain relief in the early stages of GT[3]. It how ever id not effective in the long-term and leads to high recurrence rates[3]. GT is seen to be a degenerative condition rather than an inflammatory condition and the short-term analgesia of corticosteroids is most likely due to its interaction with neurotransmitters and local neuropeptides[3]. Corticosteroids may also carry the negative effect of down-regulation of collagen production by fibroblasts, impacting the tendon's ability to respond appropriately to load[3].
Tenocyte injections[edit | edit source]
A pilot study released in 2017 found that autologous tenocyte injection was safe and effective for managing pain in chronic gluteal tendinopathy, that had not responded to other conservative treatments. There were no persistent complications and improvement in clinical scores was still noted at 24 months post-intervention[43]
Surgical Intervention[edit | edit source]
Surgery is considered in patient's with persistent pain and who have failed conservative treatment[3] and when MRI and clinical findings are consistent with a tendon tear. A retrospective study by Davies et al. (2013) revealed that in most cases, substantial improvement in abductor tendon strength and clinical performance occurred with gluteal tendon repair[44]. A study published in 2016 found that a double-row endoscopic technique allowed the surgeon to visualize, debride and repair the tendon effectively[45]. There have also been cases where a GMax tendon transfer has been done to manage the tear[46]. A very recent study (2019) found that reinforcing the repair with an allograft increased the structural strength of the repaired tendon, preventing suture pullout. The authors also reported that this approach allowed for better graft compression to the bone, potentially allowing for an increased healing rate[46]. Please see Table 2 for a rehabilitation protocol for gluteal tendon repair on the GTPS page.
While open repairs are used for large tendon tears and tears where the tendon has retracted, endoscopic repairs are preferred as they are less invasive and allow for rehabilitation to begin sooner[3].
When there is no tendon tear and conservative management has failed, endoscopic arthroscopic bursectomy together with an ITB release as been shown to be effective by Mitchell et al. (2016)[46].
| [47] | [48] |
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Allison K, Vicenzino B, Wrigley TV, Grimaldi A, Hodges PW, Bennell KL. Hip Abductor Muscle Weakness in Individuals with Gluteal Tendinopathy. Medicine and science in sports and exercise. 2016 Mar;48(3):346-52.
- ↑ Redmond JM, Cregar WM, Gupta A, Hammarstedt JE, Martin TJ, Domb BG. Trochanteric micropuncture: Treatment for gluteus medius tendinopathy. Arthroscopy techniques. 2015 Feb 1;4(1):e87-90.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 3.23 3.24 Grimaldi A, Mellor R, Hodges P, Bennell K, Wajswelner H, Vicenzino B. Gluteal tendinopathy: a review of mechanisms, assessment and management. Sports Medicine. 2015 Aug 1;45(8):1107-19.
- ↑ Fitzpatrick J, Bulsara MK, O’Donnell J, Zheng MH. Leucocyte-rich platelet-rich plasma treatment of gluteus medius and minimus tendinopathy: a double-blind randomized controlled trial with 2-year follow-up. The American journal of sports medicine. 2019 Apr;47(5):1130-7.
- ↑ 5.0 5.1 5.2 5.3 5.4 Mellor, R., Bennell, K., Grimaldi, A., Nicolson, P., Kasza, J., Hodges, P., Wajswelner, H. and Vicenzino, B., 2018. Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial. bmj, 361, p.k1662.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 6.17 6.18 Grimaldi A, Fearon A. Gluteal tendinopathy: integrating pathomechanics and clinical features in its management. journal of orthopaedic & sports physical therapy. 2015 Nov;45(11):910-22.
- ↑ Almekinders LC, Weinhold PS, Maffulli N. Compression etiology in tendinopathy. Clinics in sports medicine. 2003 Oct 1;22(4):703-10.
- ↑ 8.0 8.1 8.2 8.3 8.4 Grimaldi A, Mellor R, Hodges P, Bennell K, Wajswelner H, Vicenzino B. Gluteal tendinopathy: a review of mechanisms, assessment and management. Sports Medicine. 2015 Aug 1;45(8):1107-19.
- ↑ Birnbaum K, Siebert CH, Pandorf T, Schopphoff E, Prescher A, Niethard FU. Anatomical and biomechanical investigations of the iliotibial tract. Surgical and Radiologic Anatomy. 2004 Dec 1;26(6):433-46.
- ↑ Birnbaum K, Prescher A, Niethard FU. Hip centralizing forces of the iliotibial tract within various femoral neck angles. Journal of Pediatric Orthopaedics B. 2010 Mar 1;19(2):140-9.
- ↑ Fearon AM, Stephens S, Cook JL, Smith PN, Neeman T, Cormick W, Scarvell JM. The relationship of femoral neck shaft angle and adiposity to greater trochanteric pain syndrome in women. A case control morphology and anthropometric study. Br J Sports Med. 2012 Sep 1;46(12):888-92.
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 12.7 Lin CY, Fredericson M. Greater Trochanteric Pain Syndrome: An Update on Diagnosis and Management. Curr Phys Med Rehabil Rep. 2015;3(1);60-66.
- ↑ Lequesne M. From “periarthritis” to hip “rotator cuff” tears. Trochanteric tendinobursitis. Joint Bone Spine. 2006;4(73):344-8.
- ↑ 14.0 14.1 14.2 14.3 Ganderton C, Semciw A, Cook J, Moreira E, Pizzari T. Gluteal Loading Versus Sham Exercises to Improve Pain and Dysfunction in Postmenopausal Women with Greater Trochanteric Pain Syndrome: A Randomized Controlled Trial. Journal of Women's Health. 2018 May 1.
- ↑ Cook JL, Purdam C. Is compressive load a factor in the development of tendinopathy?. Br J Sports Med. 2012 Mar 1;46(3):163-8.
- ↑ 16.0 16.1 Fearon AM, Scarvell JM, Neeman T, Cook JL, Cormick W, Smith PN. Greater trochanteric pain syndrome: defining the clinical syndrome. Br J Sports Med. 2013 Jul 1;47(10):649-53.
- ↑ 17.0 17.1 17.2 17.3 Grimaldi A, Mellor R, Nicolson P, Hodges P, Bennell K, Vicenzino B. Utility of clinical tests to diagnose MRI-confirmed gluteal tendinopathy in patients presenting with lateral hip pain. Br J Sports Med. 2016 Sep 15:bjsports-2016.
- ↑ Ganderton C, Semciw A, Cook J, Pizzari T. Demystifying the clinical diagnosis of greater trochanteric pain syndrome in women. Journal of Women's Health. 2017 Jun 1;26(6):633-43.
- ↑ 19.0 19.1 19.2 19.3 19.4 Grimaldi A, Mellor R, Vicenzino B, et al 66 Gluteal Tendinopathy – Clinical Diagnosis Vs. Mri Diagnosis? British Journal of Sports Medicine 2014;48:A43.
- ↑ 20.0 20.1 Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 2001 Sep;44(9):2138-45.
- ↑ Reiman MP, Goode AP, Hegedus EJ, Cook CE, Wright AA. Diagnostic accuracy of clinical tests of the hip: a systematic review with meta-analysis. British journal of sports medicine. 2013 Sep 1;47(14):893-902.
- ↑ Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 2001 Sep;44(9):2138-45.
- ↑ 23.0 23.1 23.2 23.3 23.4 23.5 Cook JL, Purdam CR. The challenge of managing tendinopathy in competing athletes. Br J Sports Med. 2013 May 9:bjsports-2012.
- ↑ Video gait running analysis: alignment, issues, rear view. Available from: https://www.youtube.com/watch?v=k1hlY0EMYJw
- ↑ Domb BG, Nasser RM, Botser IB. Partial-thickness tears of the gluteus medius: rationale and technique for trans-tendinous endoscopic repair. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2010 Dec 1;26(12):1697-705.
- ↑ Cook J. Lower Limb Tendinopathy. Lower Limb Tendinopathy course; 2020 Mar 9-10; Cape Town, South Africa. P1-102.
- ↑ Fearon AM, Ganderton C, Scarvell JM, Smith PN, Neeman T, Nash C, Cook JL. Development and validation of a VISA tendinopathy questionnaire for greater trochanteric pain syndrome, the VISA-G. Manual therapy. 2015 Dec 1;20(6):805-13.
- ↑ Shimatsu K, Subramaniam S, Sim H, Aronowitz P. Ciprofloxacin-induced tendinopathy of the gluteal tendons. Journal of general internal medicine. 2014 Nov 1;29(11):1559-62.
- ↑ Ganske CM, Horning KK. Levofloxacin-induced tendinopathy of the hip. Annals of Pharmacotherapy. 2012 May;46(5):e13.
- ↑ Goyal H, Dennehy J, Barker J, Singla U. Achilles is not alone!!! Ciprofloxacin induced tendinopathy of gluteal tendons. QJM: An International Journal of Medicine. 2016 Apr 1;109(4):275-6.
- ↑ 31.0 31.1 31.2 31.3 Cook J. Lower Limb Tendinopathy. Lower Limb Tendinopathy course; 2020 Mar 9-10; Cape Town, South Africa. P1-102.
- ↑ 32.0 32.1 Rio E, Kidgell D, Purdam C, Gaida J, Moseley GL, Pearce AJ, Cook J. Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. British journal of sports medicine. 2015 Oct 1;49(19):1277-83.
- ↑ Physiohealth01: Isometric Hip Hitching. Available from: https://www.youtube.com/watch?v=b2YAUfZITl0[last accessed 03/04/2020]
- ↑ NHS Ayrshire & Arran: Hip Isometric Hip Abduction In Standing. Available from: https://www.youtube.com/watch?v=aPbiOoNz2Ws[last accessed 03/04/2020]
- ↑ Mc Auliffe S, Synott A, Casey H, Mc Creesh K, Purtill H, O'Sullivan K. Beyond the tendon: Experiences and perceptions of people with persistent Achilles tendinopathy. Musculoskeletal Science and Practice. 2017 Jun 1;29:108-14.
- ↑ Plinsinga ML, Coombes BK, Mellor R, Nicolson P, Grimaldi A, Hodges P, Bennell K, Vicenzino B. Psychological factors not strength deficits are associated with severity of gluteal tendinopathy: A cross‐sectional study. European Journal of Pain. 2018 Jul.
- ↑ Silbernagel KG, Brorsson A, Lundberg M. The majority of patients with Achilles tendinopathy recover fully when treated with exercise alone: a 5-year follow-up. The American journal of sports medicine. 2011 Mar;39(3):607-13.
- ↑ Gluteal tendinopathy, are psychological factors more important than strength?Available from:https://www.running-physio.com/gt-factors/
- ↑ Isometric hip abduction. Available from: https://www.youtube.com/watch?v=2OZ8hLR-NxM
- ↑ Bridging with progressions tightness Available from: https://www.youtube.com/watch?v=qaoa9V-bL9c
- ↑ Seo KH, Lee JY, Yoon K, Do JG, Park HJ, Lee SY, Park YS, Lee YT. Long-term outcome of low-energy extracorporeal shockwave therapy on gluteal tendinopathy documented by magnetic resonance imaging. PloS one. 2018;13(7).
- ↑ Mani-Babu S, Morrissey D, Waugh C, Screen H, Barton C. The effectiveness of extracorporeal shock wave therapy in lower limb tendinopathy: a systematic review. The American journal of sports medicine. 2015 Mar;43(3):752-61.
- ↑ Bucher TA, Ebert JR, Smith A, Breidahl W, Fallon M, Wang T, Zheng MH, Janes GC. Autologous tenocyte injection for the treatment of chronic recalcitrant gluteal tendinopathy: a prospective pilot study. Orthopaedic journal of sports medicine. 2017 Feb 21;5(2):2325967116688866.
- ↑ Davies JF, Stiehl JB, Davies JA, Geiger PB. Surgical treatment of hip abductor tendon tears. JBJS. 2013 Aug 7;95(15):1420-5.
- ↑ Domb BG, Carreira DS. Endoscopic repair of full-thickness gluteus medius tears. Arthroscopy techniques. 2013 May 1;2(2):e77-81.
- ↑ 46.0 46.1 46.2 Suppauksorn S, Nwachukwu BU, Beck EC, Okoroha KR, Nho SJ. Superior Gluteal Reconstruction for Severe Hip Abductor Deficiency. Arthroscopy Techniques. 2019 Oct 1;8(10):e1255-61.
- ↑ New York Ortho: Endoscopic Gluteus Medius repair. Available from: https://www.youtube.com/watch?v=kv1ln5MwGzE [last accessed 02/04/2020]
- ↑ Dr Robert Rupp: HIP ARTHROSCOPY WITH ILIOTIBIAL BAND RELEASE AND TROCHANTERIC BURSECTOMY. Available from:https://www.youtube.com/watch?v=Y0x30_NRCxk [last accessed 02/04/2020]