Diverticulitis: Difference between revisions
(replaced and added new references, extended Epidemiology) |
No edit summary |
||
| (6 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editors '''- [[Pathophysiology of Complex Patient Problems|Cate Hurst and Katie Countryman from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | <div class="editorbox">'''Original Editors '''- [[Pathophysiology of Complex Patient Problems|Cate Hurst and Katie Countryman from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> | ||
</div> | |||
== Introduction == | == Introduction == | ||
[[Image:Diverticula.jpg|400x300px|alt=|thumb|Showing multiple pouches (diverticula) colon]]Colonic diverticulitis is a possible adverse result of colonic diverticulosis that develops adjacent to blood vessels that penetrate these layers. Colonic diverticulosis is characterized by the protrusion of both mucosa and submucosa layers of the colon | [[Image:Diverticula.jpg|400x300px|alt=|thumb|Showing multiple pouches (diverticula) colon]]Colonic diverticulitis is a possible adverse result of colonic diverticulosis that develops adjacent to blood vessels that penetrate these layers. Colonic diverticulosis is characterized by the protrusion of both mucosa and submucosa layers of the colon and the sigmoid colon is the most affected segment of the colon<ref>Imaeda H, Hibi T. The burden of diverticular disease and its complications: west versus east. Inflammatory intestinal diseases. 2018 Aug 7;3(2):61-8.</ref>. However, in recent studies its prevalence is more common in younger ages for years it was believed to be associated with old age above 50 years old as it was in the united Kingdom<ref>Painter NS, Burkitt DP. Diverticular disease of the colon: a deficiency disease of Western civilization. British medical journal. 1971 May 5;2(5759):450.</ref><ref name=":2">Bhatia M, Mattoo A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10410187/ Diverticulosis and diverticulitis: epidemiology, pathophysiology, and current treatment trends]. Cureus. 2023 Aug 8;15(8).</ref>. | ||
Diverticulosis is mainly asymptomatic whilst acute diverticulitis is a potentially life-threatening illness. It develops in approximately 10-25% of individuals with diverticulosis<ref>Jacobs DO. Diverticulitis. New England Journal of Medicine. 2007 Nov 15;357(20):2057-66.</ref>. | Diverticulosis is mainly asymptomatic whilst acute diverticulitis is a potentially life-threatening illness. It develops in approximately 10-25% of individuals with diverticulosis<ref>Jacobs DO. Diverticulitis. New England Journal of Medicine. 2007 Nov 15;357(20):2057-66.</ref>. However recent data, utilizing colonoscopy and CT scans, suggest the actual risk is below 5%<ref name=":1">Strate LL, Morris AM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6716971/ Epidemiology, pathophysiology, and treatment of diverticulitis.] Gastroenterology. 2019 Apr 1;156(5):1282-98.</ref>. | ||
{{#ev:youtube|K64v_V2Z3QE|412}}<ref>NutritionFacts.org. Diverticulosis: When Our Most Common Gut Disorder Hardly Existed. Available from: http://www.youtube.com/watch?v=K64v_V2Z3QE[last accessed 19/3/2024]</ref> | |||
== Epidemiology == | == Epidemiology == | ||
[[Image:ColonPouches.jpg|Colon pouches|right|alt=|frameless]] | [[Image:ColonPouches.jpg|Colon pouches|right|alt=|frameless]]and the demographics of both are very similar. It seems to be more prevalent in the western part of the globe than in Asian countries; however, recently there has been a rise of 0.5% in Asian countries too. But despite sophisticated colonoscopy and CT scans, diverticulitis still remains common in the US, where more than half of Americans aged above 60 have diverticulosis<ref name=":1" />. The prevalence of diverticulitis usually rises along with the age of the patient; however, during recent years, there has been an increase in the occurrence of diverticulitis even among young people, which reached a 132% growth rate in diverticulitis cases among the 40-49-year-old population between 1980 and 2007. The highest rates of hospitalization for diverticulitis are found in whites (62 out of 100,000), followed by similar rates among African Americans and Hispanics (approximately 30 out of 100,000), and Asians have the lowest rates (10 per 100,000)<ref name=":1" />. | ||
On | On the other hand compared to natives of Western countries immigrants from non-Western countries initially exhibit a lower risk of being hospitalized for diverticular disease however this risk increases with the length of their stay in the new country<ref name=":1" />. A study found that diverticular disease of the colon is typically an acquired disorder and that a change in lifestyle may have an effect on the diseases development<ref>Hjern F, Johansson C, Mellgren A, Baxter NN, Hjern A. [https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2036.2006.02805.x Diverticular disease and migration–the influence of acculturation to a Western lifestyle on diverticular disease]. Alimentary pharmacology & therapeutics. 2006 Mar;23(6):797-805.</ref>. | ||
== Etiology == | == Etiology == | ||
Colonic diverticular development may involve bowel wall abnormality, increased intraluminal pressure, and lack of dietary fibre. Diverticulitis is the result of obstruction of the neck of the diverticulum (outpouch), with consequential inflammation, perforation, and infection. A walled region of soft tissue may later progress to abscess formation and generalised peritonitis.<ref name=":0">Radiopedia [https://radiopaedia.org/articles/colonic-diverticulosis?lang=gb Colonic diverticulosis] Available:https://radiopaedia.org/articles/colonic-diverticulosis?lang=gb (accessed 22.1.20230</ref> | |||
'''Risk Factors''':<ref>Strate LL, Morris AM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6716971/ Epidemiology, pathophysiology, and treatment of diverticulitis]. Gastroenterology. 2019 Apr 1;156(5):1282-98.</ref> | |||
* Increased age. | |||
* Constipation | |||
* [[Sedentary Behaviour|Sedentary lifestyle]] | |||
* [[Obesity]] (especially central obesity) | |||
* [[Smoking Cessation and Brief Intervention|Smoking]] | |||
* [[NSAIDs|NSAIDS]] | |||
* Dietary patterns that include (Red meat<ref name="patho">Goodman CC, Fuller KS. Pathology: implications for the physical therapist. 3rd ed. St. Louis: Saunders Elsevier, 2009.</ref>, processed grains, and fat) | |||
* Genetic factors<ref name=":3">Peery AF, Shaukat A, Strate LL. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10410187/ AGA clinical practice update on medical management of colonic diverticulitis: expert review.] Gastroenterology. 2021 Feb 1;160(3):906-11.</ref>. | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
| Line 29: | Line 33: | ||
The presentation and signs and symptoms can vary for each individual patient. Although many of the patients have the same side effects, they are usually experienced at different intensities and at various times. Some of the most common signs and symptoms that are present with the diverticulitis diagnosis include the following<ref name="DD">Goodman CC, Snyder TE. Differential diagnosis for physical therapists: screening for referral. 4th ed. St. Louis: Saunders Elsevier, 2007.</ref>: | The presentation and signs and symptoms can vary for each individual patient. Although many of the patients have the same side effects, they are usually experienced at different intensities and at various times. Some of the most common signs and symptoms that are present with the diverticulitis diagnosis include the following<ref name="DD">Goodman CC, Snyder TE. Differential diagnosis for physical therapists: screening for referral. 4th ed. St. Louis: Saunders Elsevier, 2007.</ref>: | ||
* Sudden abdominal pain, usually in the left lower quadrant abdomen, | * Sudden abdominal pain, usually in the left lower quadrant abdomen (49%), and is often associated with an increase in inflammatory markers and temperature. | ||
* Palpable mass | * Palpable mass | ||
* Irregular bowel movements | * Irregular bowel movements and changes in bowel habits. | ||
* Bowel sounds absent or decreased | * Bowel sounds absent or decreased | ||
* Flatulence | * Flatulence | ||
| Line 37: | Line 41: | ||
* Nausea/ Vomiting | * Nausea/ Vomiting | ||
* Bloody stools | * Bloody stools | ||
* Increased frequency of urination<ref name="patho" /> | * Increased frequency of urination<ref name="patho" /><ref name=":2" /> | ||
Possible complications include perforation of bowels, and abscess formation that seen in around 17% of patients<ref>Mali J, Mentula P, Leppäniemi A, Sallinen V. Determinants of treatment and outcomes of diverticular abscesses. World Journal of Emergency Surgery. 2019 Dec;14:1-9.</ref>, fistula formation, gastrointestinal hemorrhage, obstruction, bleeding, and perforative peritonitis in 1-2% of patients<ref>Edna TH, Jamal Talabani A, Lydersen S, Endreseth BH. Survival after acute colon diverticulitis treated in hospital. International journal of colorectal disease. 2014 Nov;29:1361-7.</ref>. | |||
{{#ev:youtube|WuCow8J1dIw|412}}<ref>Armando Hasud. Diverticular Disease (diverticulitis) - Overview. Available from: http://www.youtube.com/watch?v=WuCow8J1dIw[last accessed 19/3/2024]</ref> | |||
== Pathophysiology == | |||
== | * Formation of Diverticula: starts when a small pouches, known as diverticula, develop in the colon's lining, forms at weak points in the colon, often due to increased pressure inside, or diet low in fiber that cause straining and ear down with bowel movement. | ||
* Inflammation and Infection: sometimes these diverticula can become blocked with stool or food particles. This blockage and bacterial growth can cause the diverticula to become inflamed or infected, leading to the condition known as diverticulitis. | |||
* Altered microbiomes: The inflammation and infection can cause microscopic or macroscopic perforation of a diverticulum. This perforation can lead to a local abscess or more widespread infection in the abdominal cavity (peritonitis). | |||
* [[Immune System|Immune Response]]: the body's immune system responds to this infection and [[Inflammation Acute and Chronic|inflammation]], and can sometimes lead to the healing of the affected area. However, in sever cases this response can contribute to complications such as; scarring and significant inflammation leading to obstruction of bowel. | |||
* Possible Complications: if the inflammation is severe, it can cause a small tear in the pouch. This tear can lead to an infection spreading outside the colon (possibly leading to an abscess, which is a trapped pocket of infection) or cause other issues like scarring or narrowing of the colon<ref name=":1" />. | |||
== Diagnosis == | |||
Diverticulitis is typically diagnosed during an acute attack due to complaints of severe abdominal pain. Diverticulitis diagnosis is typically confirmed with the presence of constitutional symptoms, bloody stools, elevated white blood cell count, and with the use of imaging studies.<ref name="DD" /> Due to the prevalence of abdominal pain in several conditions, the physician may order a number of tests to rule out other causes of abdominal pain and associated symptoms. | |||
[[Ultrasound Scans|Ultrasound]]: good to detect simple cases of diverticular disease. | |||
[[CT Scans|CT scan]]: helps to provide detailed and specific results. This will be helpful in monitoring treatment progress and planning future interventions. Divergent disease classification depends on CT results<ref name=":2" />. | |||
Endoscopic evaluation: it can be used for tissue diagnostics and is useful for direct visualization, their use in acute attacks of diverticular disease is controversial because of the potential risks and is often avoided in these cases. In the post-attack setting, there is some debate as to whether a colonoscopy should be performed routinely. However, some experts recommend the use of flexible sigmoidsoscopy because of its less invasive nature and the fact that the sagittal region of the colon is the area most affected by diverticular disease.<ref>Agarwal AK, Karanjawala BE, Maykel JA, Johnson EK, Steele SR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4168084/ Routine colonic endoscopic evaluation following resolution of acute diverticulitis: is it necessary?.] World Journal of Gastroenterology: WJG. 2014 Sep 9;20(35):12509.</ref>. | |||
=== Classification of Diverticulitis Depending on CT scan === | |||
{| class="wikitable" | |||
| colspan="1" rowspan="1" |Class | |||
| colspan="1" rowspan="1" |CT findings | |||
|- | |||
| colspan="1" rowspan="1" |Mild disease | |||
| colspan="1" rowspan="1" |Bowel wall thickening, fat stranding | |||
|- | |||
| colspan="1" rowspan="1" |Moderate disease | |||
| colspan="1" rowspan="1" |Bowel wall thickness >3 mm, phlegmon/small abscess | |||
|- | |||
| colspan="1" rowspan="1" |Severe disease | |||
| colspan="1" rowspan="1" |Bowel wall thickening >5 mm, perforation with subdiaphragmatic free air, abscess >5 mm<ref name=":2" /> | |||
|} | |||
== Treatment == | |||
Treatment depends on a range of factors, in particular comorbidities and stage of the disease. Diverticulitis can be treated with rest, changes in diet, or antibiotics, and in severe cases may require surgery. | |||
* Localised disease: conservative management with intravenous antibiotics and rehydration usually is enough, the antibiotics should be for both aerobic and anaerobic bacteria especially for mild cases to avoid and reduce the risk of developing complications as advised by American Gastroenterology Association<ref name=":3" /><ref name=":4">Sartelli M, Weber DG, Kluger Y, Ansaloni L, Coccolini F, Abu-Zidan F, Augustin G, Ben-Ishay O, Biffl WL, Bouliaris K, Catena R. [https://wjes.biomedcentral.com/articles/10.1186/s13017-020-00313-4#Sec10 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting]. World Journal of Emergency Surgery. 2020 Dec;15:1-8.</ref>. | |||
* Surgery maybe required if a patient has a complication (abscess, fistula formation, bowel obstruction), has had multiple episodes of uncomplicated diverticulitis, or is immune-compromised. Surgery may be recommended or it may require emergency surgery<ref name=":4" />. however, instead of deciding on elective segmental resection just by counting the number of episodes, it's better to make a personalized choice. This should involve considering how severe the disease is, what the patient prefers and values, and the risks and benefits of the procedure<ref name=":3" />. | |||
* Hartmann’s procedure is the most common surgery used to treat complex diverticular disease. It is a type of surgery only used in very serious cases. Hartmann removes the diseased part of colon (usually called the “sigmoid” section) and creates a temporary colonostomy, in which the end of your remaining colon is pulled out to belly button. <ref name=":2" />. | |||
Prevention of diverticulitis is from a variety of lifestyle changes. Adherence to a high-fiber diet, decreased red meat intake, prevention of constipation with an adequate balance of fluids and fiber intake, cessation of smoking, and regular exercise during remission may decrease the risk of diverticulitis.<ref name="patho" /> | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
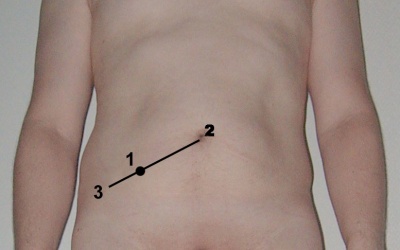
[[Image:McBurney's point.jpg|400x300px|McBurney's Point|alt=|thumb]]As a physical therapist, the optimal goal is to help a patient return moving in a functional way. Being active helps decrease the chances of developing diverticulitis because movement helps promote proper bowel movement. Therapists can help patients with proper exercise, strengthening, and positioning to help them get the best and safest movement possible. Patients with diverticulitis must be cautious about doing activities that increase the pressure on their abdomen so further herniation does not happen<ref name="DD" />. | [[Image:McBurney's point.jpg|400x300px|McBurney's Point|alt=|thumb]]As a physical therapist, the optimal goal is to help a patient return to moving in a functional way. Being active helps decrease the chances of developing diverticulitis because movement helps promote proper bowel movement. Therapists can help patients with proper exercise, strengthening, and positioning to help them get the best and safest movement possible. Patients with diverticulitis must be cautious about doing activities that increase the pressure on their abdomen so further herniation does not happen<ref name="DD" />. In addition, vigorous activity like running is associated with decrease risk of diverticular disease<ref name=":1" />. | ||
Exercise can be seen as a protective mechanism because it promotes movement to the body, but also the different systems that could be affected by a sedentary lifestyle<ref name="DD" />. Depending on the symptoms that the patients present with, it is up to the therapist to do appropriate screening or testing to identify what is involved and what is causing the issues. | |||
The can advise and encourage the patient to maintain a lower bod mass index, be physically active, and consume high-quality diet rich in in fruits, vegetables, and whole grains<ref name=":3" />. | |||
A common area of pain is the left lower quadrant, including referred pain to | A common area of pain is the left lower quadrant, including referred pain to the lower back or thigh from an abscess<ref name="Hammond">Hammond N. Left Lower-Quadrant Pain: Guidelines from the American College of Radiology Appropriateness Criteria. American Family Physician. 2010;82(7):766-770.</ref>. For example, the obturator test, manual muscle testing and palpation of the iliopsoas, or McBurney’s point palpation can be done to look at positive or negative testing of referred pain to the thigh<ref name="DD" /><ref name="Hammond" />. | ||
== References == | == References == | ||
<references /> | <references /> | ||
Latest revision as of 08:23, 19 March 2024
Introduction[edit | edit source]
Colonic diverticulitis is a possible adverse result of colonic diverticulosis that develops adjacent to blood vessels that penetrate these layers. Colonic diverticulosis is characterized by the protrusion of both mucosa and submucosa layers of the colon and the sigmoid colon is the most affected segment of the colon[1]. However, in recent studies its prevalence is more common in younger ages for years it was believed to be associated with old age above 50 years old as it was in the united Kingdom[2][3].
Diverticulosis is mainly asymptomatic whilst acute diverticulitis is a potentially life-threatening illness. It develops in approximately 10-25% of individuals with diverticulosis[4]. However recent data, utilizing colonoscopy and CT scans, suggest the actual risk is below 5%[5].
Epidemiology[edit | edit source]
and the demographics of both are very similar. It seems to be more prevalent in the western part of the globe than in Asian countries; however, recently there has been a rise of 0.5% in Asian countries too. But despite sophisticated colonoscopy and CT scans, diverticulitis still remains common in the US, where more than half of Americans aged above 60 have diverticulosis[5]. The prevalence of diverticulitis usually rises along with the age of the patient; however, during recent years, there has been an increase in the occurrence of diverticulitis even among young people, which reached a 132% growth rate in diverticulitis cases among the 40-49-year-old population between 1980 and 2007. The highest rates of hospitalization for diverticulitis are found in whites (62 out of 100,000), followed by similar rates among African Americans and Hispanics (approximately 30 out of 100,000), and Asians have the lowest rates (10 per 100,000)[5].
On the other hand compared to natives of Western countries immigrants from non-Western countries initially exhibit a lower risk of being hospitalized for diverticular disease however this risk increases with the length of their stay in the new country[5]. A study found that diverticular disease of the colon is typically an acquired disorder and that a change in lifestyle may have an effect on the diseases development[7].
Etiology[edit | edit source]
Colonic diverticular development may involve bowel wall abnormality, increased intraluminal pressure, and lack of dietary fibre. Diverticulitis is the result of obstruction of the neck of the diverticulum (outpouch), with consequential inflammation, perforation, and infection. A walled region of soft tissue may later progress to abscess formation and generalised peritonitis.[8]
Risk Factors:[9]
- Increased age.
- Constipation
- Sedentary lifestyle
- Obesity (especially central obesity)
- Smoking
- NSAIDS
- Dietary patterns that include (Red meat[10], processed grains, and fat)
- Genetic factors[11].
Characteristics/Clinical Presentation[edit | edit source]
The presentation and signs and symptoms can vary for each individual patient. Although many of the patients have the same side effects, they are usually experienced at different intensities and at various times. Some of the most common signs and symptoms that are present with the diverticulitis diagnosis include the following[12]:
- Sudden abdominal pain, usually in the left lower quadrant abdomen (49%), and is often associated with an increase in inflammatory markers and temperature.
- Palpable mass
- Irregular bowel movements and changes in bowel habits.
- Bowel sounds absent or decreased
- Flatulence
- Fever
- Nausea/ Vomiting
- Bloody stools
- Increased frequency of urination[10][3]
Possible complications include perforation of bowels, and abscess formation that seen in around 17% of patients[13], fistula formation, gastrointestinal hemorrhage, obstruction, bleeding, and perforative peritonitis in 1-2% of patients[14].
Pathophysiology[edit | edit source]
- Formation of Diverticula: starts when a small pouches, known as diverticula, develop in the colon's lining, forms at weak points in the colon, often due to increased pressure inside, or diet low in fiber that cause straining and ear down with bowel movement.
- Inflammation and Infection: sometimes these diverticula can become blocked with stool or food particles. This blockage and bacterial growth can cause the diverticula to become inflamed or infected, leading to the condition known as diverticulitis.
- Altered microbiomes: The inflammation and infection can cause microscopic or macroscopic perforation of a diverticulum. This perforation can lead to a local abscess or more widespread infection in the abdominal cavity (peritonitis).
- Immune Response: the body's immune system responds to this infection and inflammation, and can sometimes lead to the healing of the affected area. However, in sever cases this response can contribute to complications such as; scarring and significant inflammation leading to obstruction of bowel.
- Possible Complications: if the inflammation is severe, it can cause a small tear in the pouch. This tear can lead to an infection spreading outside the colon (possibly leading to an abscess, which is a trapped pocket of infection) or cause other issues like scarring or narrowing of the colon[5].
Diagnosis[edit | edit source]
Diverticulitis is typically diagnosed during an acute attack due to complaints of severe abdominal pain. Diverticulitis diagnosis is typically confirmed with the presence of constitutional symptoms, bloody stools, elevated white blood cell count, and with the use of imaging studies.[12] Due to the prevalence of abdominal pain in several conditions, the physician may order a number of tests to rule out other causes of abdominal pain and associated symptoms.
Ultrasound: good to detect simple cases of diverticular disease.
CT scan: helps to provide detailed and specific results. This will be helpful in monitoring treatment progress and planning future interventions. Divergent disease classification depends on CT results[3].
Endoscopic evaluation: it can be used for tissue diagnostics and is useful for direct visualization, their use in acute attacks of diverticular disease is controversial because of the potential risks and is often avoided in these cases. In the post-attack setting, there is some debate as to whether a colonoscopy should be performed routinely. However, some experts recommend the use of flexible sigmoidsoscopy because of its less invasive nature and the fact that the sagittal region of the colon is the area most affected by diverticular disease.[16].
Classification of Diverticulitis Depending on CT scan[edit | edit source]
| Class | CT findings |
| Mild disease | Bowel wall thickening, fat stranding |
| Moderate disease | Bowel wall thickness >3 mm, phlegmon/small abscess |
| Severe disease | Bowel wall thickening >5 mm, perforation with subdiaphragmatic free air, abscess >5 mm[3] |
Treatment[edit | edit source]
Treatment depends on a range of factors, in particular comorbidities and stage of the disease. Diverticulitis can be treated with rest, changes in diet, or antibiotics, and in severe cases may require surgery.
- Localised disease: conservative management with intravenous antibiotics and rehydration usually is enough, the antibiotics should be for both aerobic and anaerobic bacteria especially for mild cases to avoid and reduce the risk of developing complications as advised by American Gastroenterology Association[11][17].
- Surgery maybe required if a patient has a complication (abscess, fistula formation, bowel obstruction), has had multiple episodes of uncomplicated diverticulitis, or is immune-compromised. Surgery may be recommended or it may require emergency surgery[17]. however, instead of deciding on elective segmental resection just by counting the number of episodes, it's better to make a personalized choice. This should involve considering how severe the disease is, what the patient prefers and values, and the risks and benefits of the procedure[11].
- Hartmann’s procedure is the most common surgery used to treat complex diverticular disease. It is a type of surgery only used in very serious cases. Hartmann removes the diseased part of colon (usually called the “sigmoid” section) and creates a temporary colonostomy, in which the end of your remaining colon is pulled out to belly button. [3].
Prevention of diverticulitis is from a variety of lifestyle changes. Adherence to a high-fiber diet, decreased red meat intake, prevention of constipation with an adequate balance of fluids and fiber intake, cessation of smoking, and regular exercise during remission may decrease the risk of diverticulitis.[10]
Physical Therapy Management[edit | edit source]
As a physical therapist, the optimal goal is to help a patient return to moving in a functional way. Being active helps decrease the chances of developing diverticulitis because movement helps promote proper bowel movement. Therapists can help patients with proper exercise, strengthening, and positioning to help them get the best and safest movement possible. Patients with diverticulitis must be cautious about doing activities that increase the pressure on their abdomen so further herniation does not happen[12]. In addition, vigorous activity like running is associated with decrease risk of diverticular disease[5].
Exercise can be seen as a protective mechanism because it promotes movement to the body, but also the different systems that could be affected by a sedentary lifestyle[12]. Depending on the symptoms that the patients present with, it is up to the therapist to do appropriate screening or testing to identify what is involved and what is causing the issues.
The can advise and encourage the patient to maintain a lower bod mass index, be physically active, and consume high-quality diet rich in in fruits, vegetables, and whole grains[11].
A common area of pain is the left lower quadrant, including referred pain to the lower back or thigh from an abscess[18]. For example, the obturator test, manual muscle testing and palpation of the iliopsoas, or McBurney’s point palpation can be done to look at positive or negative testing of referred pain to the thigh[12][18].
References[edit | edit source]
- ↑ Imaeda H, Hibi T. The burden of diverticular disease and its complications: west versus east. Inflammatory intestinal diseases. 2018 Aug 7;3(2):61-8.
- ↑ Painter NS, Burkitt DP. Diverticular disease of the colon: a deficiency disease of Western civilization. British medical journal. 1971 May 5;2(5759):450.
- ↑ 3.0 3.1 3.2 3.3 3.4 Bhatia M, Mattoo A. Diverticulosis and diverticulitis: epidemiology, pathophysiology, and current treatment trends. Cureus. 2023 Aug 8;15(8).
- ↑ Jacobs DO. Diverticulitis. New England Journal of Medicine. 2007 Nov 15;357(20):2057-66.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Strate LL, Morris AM. Epidemiology, pathophysiology, and treatment of diverticulitis. Gastroenterology. 2019 Apr 1;156(5):1282-98.
- ↑ NutritionFacts.org. Diverticulosis: When Our Most Common Gut Disorder Hardly Existed. Available from: http://www.youtube.com/watch?v=K64v_V2Z3QE[last accessed 19/3/2024]
- ↑ Hjern F, Johansson C, Mellgren A, Baxter NN, Hjern A. Diverticular disease and migration–the influence of acculturation to a Western lifestyle on diverticular disease. Alimentary pharmacology & therapeutics. 2006 Mar;23(6):797-805.
- ↑ Radiopedia Colonic diverticulosis Available:https://radiopaedia.org/articles/colonic-diverticulosis?lang=gb (accessed 22.1.20230
- ↑ Strate LL, Morris AM. Epidemiology, pathophysiology, and treatment of diverticulitis. Gastroenterology. 2019 Apr 1;156(5):1282-98.
- ↑ 10.0 10.1 10.2 Goodman CC, Fuller KS. Pathology: implications for the physical therapist. 3rd ed. St. Louis: Saunders Elsevier, 2009.
- ↑ 11.0 11.1 11.2 11.3 Peery AF, Shaukat A, Strate LL. AGA clinical practice update on medical management of colonic diverticulitis: expert review. Gastroenterology. 2021 Feb 1;160(3):906-11.
- ↑ 12.0 12.1 12.2 12.3 12.4 Goodman CC, Snyder TE. Differential diagnosis for physical therapists: screening for referral. 4th ed. St. Louis: Saunders Elsevier, 2007.
- ↑ Mali J, Mentula P, Leppäniemi A, Sallinen V. Determinants of treatment and outcomes of diverticular abscesses. World Journal of Emergency Surgery. 2019 Dec;14:1-9.
- ↑ Edna TH, Jamal Talabani A, Lydersen S, Endreseth BH. Survival after acute colon diverticulitis treated in hospital. International journal of colorectal disease. 2014 Nov;29:1361-7.
- ↑ Armando Hasud. Diverticular Disease (diverticulitis) - Overview. Available from: http://www.youtube.com/watch?v=WuCow8J1dIw[last accessed 19/3/2024]
- ↑ Agarwal AK, Karanjawala BE, Maykel JA, Johnson EK, Steele SR. Routine colonic endoscopic evaluation following resolution of acute diverticulitis: is it necessary?. World Journal of Gastroenterology: WJG. 2014 Sep 9;20(35):12509.
- ↑ 17.0 17.1 Sartelli M, Weber DG, Kluger Y, Ansaloni L, Coccolini F, Abu-Zidan F, Augustin G, Ben-Ishay O, Biffl WL, Bouliaris K, Catena R. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World Journal of Emergency Surgery. 2020 Dec;15:1-8.
- ↑ 18.0 18.1 Hammond N. Left Lower-Quadrant Pain: Guidelines from the American College of Radiology Appropriateness Criteria. American Family Physician. 2010;82(7):766-770.