Crohn's Disease: Difference between revisions
Kim Jackson (talk | contribs) No edit summary |
mNo edit summary |
||
| (14 intermediate revisions by 4 users not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
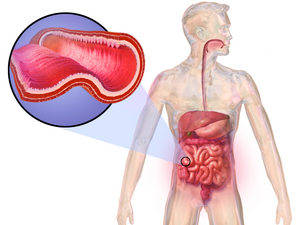
[[File:Crohn's Disease.png|thumb|CD chronic inflammation GI tract]] | |||
Crohn disease (CD) and ulcerative colitis (UC) are both conditions commonly referred to as [[Irritable Bowel Syndrome|inflammatory bowel disease]] (IBD). CD causes chronic inflammation of the gastrointestinal tract. In Crohn disease, the inflammation extends through the entire thickness of the bowel wall from the mucosa to the serosa. | |||
CD is a serious chronic inflammatory disorder that is difficult to diagnose and manage. The disease has a relapsing and remitting course. Many relapses can cause Crohn disease to progress from mild to moderate to severe penetrating (fistulization) or stricturing disease. There is no cure and most patients experience a poor quality of life..<ref name=":0">Ranasinghe IR, Hsu R. Crohn disease. Available: https://www.ncbi.nlm.nih.gov/books/NBK436021/<nowiki/>(accessed 1.10.2022)</ref> | |||
The | == Etiology == | ||
The cause of CD is not known but genetics seem to play a role as does the environmental affects on the immune system. | |||
The gut bacteria of people with Crohn’s disease changes but it still isn’t clear if the change is caused by inflammation. | |||
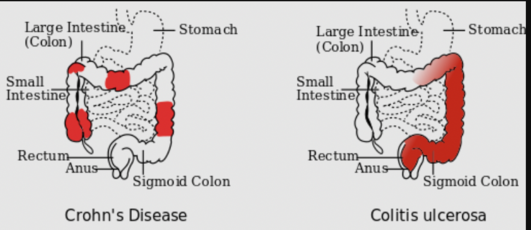
Possibly a diet full of highly processed foods like sugary drinks and fast food, may increase the risk of developing Crohn’s. Crohn’s is not infectious. <ref name=":1">Crohns and Colitis Australia CD Available:https://crohnsandcolitis.org.au/about-crohns-colitis/crohns-disease/about-crohns-disease/ (accessed 1.10.2022)</ref>[[File:Crohn.png|thumb|531x531px|The 3 most common sites of intestinal involvement in CD (L) compared to the areas affected by ''ulcerative colitis'' (''R'').|alt=|center]] | |||
== Epidemiology == | |||
[[Image:CD map.jpeg|World Distribution of CD|alt=|thumb]] | |||
CD is most prevalent in the western developed world in North America, northern Europe, and New Zealand. | |||
The incidence of CD is bimodal with the onset occurring most frequently between ages 15 to 30 years and 40 to 60 years old. | |||
While Crohn’s is a chronic disease, the patients will experience bouts of flare ups and remission with the absence of symptoms <ref name="CCFA" />. | It is more prominent in urban than rural areas.<ref name=":0" /> | ||
== Symptoms of Crohn’s Disease == | |||
[[File:Diarrhea.png|thumb|Diarrhea a symptom]] | |||
While Crohn’s is a chronic disease, the patients will experience bouts of flare ups and remission with the absence of symptoms <ref name="CCFA">Crohn’s and Colitis Foundation of America (CCFA). About Crohn’s Disease. http://ccfa.org/info/about/crohns (accessed 4 March 2010)</ref>. | |||
Patients with flare-ups of CD usually present with abdominal pain (right lower quadrant), flatulence/bloating, diarrhea (can include mucus and blood), fever, weight loss, anemia. In acute cases, perianal abscess, perianal Crohn disease, and cutaneous fistulas can be seen.<ref name=":0" /> | |||
About 50% of individuals with Crohn’s Disease will have mild symptoms. The other half may experience more severe symptoms and pain that appears to come and go. These patients undergo painful exacerbations and potentially symptom free remissions. The remissions might last for months to years but the symptoms will eventually return<ref name="CCFA" />. | |||
The below viewing is a 5 minute presentation from a clients viewpoint. | |||
{| class="FCK__ShowTableBorders" width="40%" cellspacing="1" cellpadding="1" border="0" align="centre" | |||
|- | |||
| align="right" | | |||
{{#ev:youtube|Npda8xr2G-Y|300}}<ref name="Thomas">Thomas Craig. A Frank discussion on Crohn's Disease. Available at http://www.youtube.com/watch?v=Npda8xr2G-Y (last accessed 4/510)</ref> | |||
|} | |||
== Types of Crohn's Disease == | |||
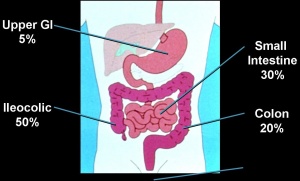
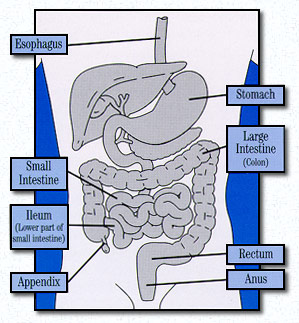
[[Image:Crohn's distribution.jpg|thumb|right|300x200px|Distribution of Crohn's Disease within the Gastrointestinal tract]][[Image:What is Crohn's disease.jpg|frame|right|200px|Gastrointestinal Tract in which Crohn's Disease affects]]There are different types of Crohn’s Disease dependent upon the location and disease pattern within the GI tract. The different locations of Crohn’s Disease include: | |||
' | |||
[[Image:Crohn's | |||
<ref name="John">Crohn’s Disease: Introduction. John Hopkins Medicine. Available at http://www.hopkins-gi.org/GDL_Disease.aspx?CurrentUDV=31&GDL_Disease_ID=291F2209-F8A9-4011-8094-11EC9BF3100E&GDL_DC_ID=D03119D7-57A3-4890-A717-CF1E7426C8BA (accessed 5 April 2010).</ref> | |||
# '''Gastroduodenal Crohn’s Disease:''' Located in the upper gastrointenstinal tract and affects the stomach and first part of the small intestine (duodenum). This is uncommon and symptoms occur in 5% of those diagnosed with Crohn’s. | |||
# '''Jejunoileitis''': This is also uncommon in the general population of those diagnosed with Crohn’s disease. Inflammation is located in the Jejunum or Second part of small intestines. | |||
# '''Ileitis:''' Inflammation located in the last part of small intestine or ileum and affects 30% of individuals diagnosed with Crohn’s disease. | |||
# '''Ileocolitis:''' This is the most common form of Crohn’s disease and affects 50% of those diagnosed with inflammation located in the ileum and colon. | |||
# '''Crohn’s Colitis:''' This affects 20% of individuals diagnosed with Crohn’s disease with inflammation located in the colon. The perianal disease and extraintestinal complications are more commonly associated in these individuals. | |||
# '''Perianal Disease:''' This occurs in 1/3 of individuals diagnosed with Crohn’s disease. These individuals can have fistulae, fissures, abscesses or skin tags (fleshy growths outside the anus) <ref name="Knol">Cheifetz Adam, Moss Alan, Peppercorn Mark. Crohn’s Disease. Knol Beta. Available at http://knol.google.com/k/crohn-s-disease#. Accessed 5 April 2010.</ref> | |||
= | <ref name="Knol" /> | ||
== Complications == | |||
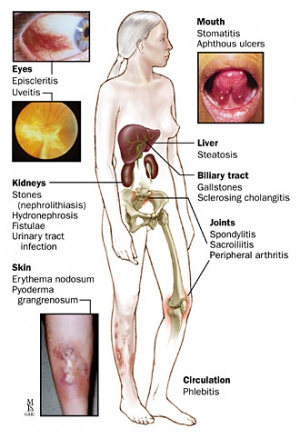
[[Image:Body complications.jpg|thumb|right|300px|Extraintestinal manifestations of Crohn's disease]]CD is a systemic disease and has manifold intestinal and extra-intestinal complications. Examples include: | |||
* Stricture formation, fistulae and abscesses | |||
* Colorectal carcinoma | |||
* Ankylosing spondylitis | |||
* Erythema nodosum, pyoderma gangrenosum | |||
* Kidney and gall stones | |||
* Anemia | |||
* Hypercoagulable state | |||
* Osteoporosis | |||
* Eye inflammation<ref name=":0" /><br> | |||
== Diagnosis == | |||
The diagnosis is made by ruling out other potential causes. Investigations include: blood tests, fecal occult blood test, colonoscopy, flexible sigmoidoscopy, barium enema or small bowel imaging, CT of the GI tract, or a capsule endoscopy.<ref name="Knol" /> | |||
Many CD patients who develop complications require surgery and possibly multiple procedures in time. Once a patient has had surgery, surveillance endoscopy is recommended in six to 12 months. If there is no endoscopic recurrence, ileocolonoscopy should be repeated in 1 to 3 years.<ref name=":0" /> | |||
== Treatment/Management == | |||
[[File:Methotrexate.jpg|thumb|Methotrexate]] | |||
The medical treatment is roughly grouped into two classes: | |||
# Mild to moderate disease can be treated by oral mesalamine, [[DMARDs in the Management of Rheumatoid Arthritis|immunomodulators]], methotrexate, and [[Corticosteroid Medication|steroids]]. | |||
# Moderate to severe disease will be best treated using a combination of immunomodulators and [[BDMARDs in the Management of Rheumatoid Arthritis|biologics]] or biologics alone. | |||
< | * Dietician involvement is recommended and nutritional supplementation are highly recommended before and during the treatment of Crohn disease. | ||
* Poor pregnancy outcomes are associated with active CD. Disease flares should be treated aggressively in pregnancy<ref>Kalla R, Ventham NT, Satsangi J, Arnott ID. Crohn’s disease. Bmj. 2014 Nov 19;349. Available:https://www.bmj.com/content/349/bmj.g6670 (accessed 1.10.2022)</ref> | |||
* Mental health counseling for may be needed depression | |||
* Sound education about CD and best ways to live with the conditions, for example: Avoid NSAIDs as they may exacerbate disease; Manage mild diarrhea with antidiarrheals; Avoid smoking; heed dietician advice.<ref name=":0" /> | |||
== Physical Therapy Management == | |||
Individuals may need physiotherapy to treat the following. | |||
# Crohn’s disease is associated with [[arthritis]], notably arthritis of the [[Spondyloarthritis|lumbar spine]] and [[Sacroiliac Joint Syndrome|sacroiliac joints]]. Though arthritis usually affects [[Older People - An Introduction|older people]], Crohn's-related arthritis is common in young people with the disease.<ref>Enzine articles The Link Between Crohn's Disease And Lower Back Pain Available:https://ezinearticles.com/?The-Link-Between-Crohns-Disease-And-Lower-Back-Pain&id=7654760 (accessed 1.10.2022)</ref> When a patient presents to physical therapy with low back, sacroiliac or hip pain, it is vital for the therapist to screen for potential organic sources of the pain and for a history of inflammatory bowel disease. See links re treatment. | |||
# CD prevents correct absorption of [[Nutrition|nutrient]]<nowiki/>s through the intestines into the body. [[Vitamin D Deficiency|Vitamin D]] and calcium are key nutrients for bone health, and deficiency can lead to [[osteoporosis]]. Osteoporosis often leads to [[Insufficiency Fracture|insufficiency fractures]] eg in the vertebrae. Vertebral fractures can cause changes in [[Thoracic Hyperkyphosis|spinal curvature]], leaving other vertebrae more susceptible to fracture. Pain may result from the fracture itself, inflammation and/or [[Biomechanics|biomechanical]] changes. Educate clients regarding osteoporosis. | |||
# Hydration is very important in patient’s with Crohn’s disease so the therapist should be aware of signs of dehydration when exercising, for example headache, dry lips, disorientation. | |||
# Exercise prescriptions have the ability to boost the immune system, reduce depression, and improve the body image of the patient. In addition to providing this exercise program, therapists can better create coping mechanisms as well as techniques to manage the unexpectedness of Crohn’s Disease<ref name="Patho">Goodman CC, Fuller KS. Pathophysiology: Implications for the Physical Therapist. 3rd ed. St. Louis, MO: Saunders-Elsevier; 2009.</ref>. | |||
== | == Outcome Measures == | ||
An outcome measure has been created to track the progress or lack of progress for individuals affected with Crohn’s disease called Crohn’s Disease Activity Index (CDAI). A score below 150 indicates a better prognosis than higher scores. This measure helps to track an individual’s progress from week to week to determine if the symptoms are better or worse. This is more of a gauge of progress and not a prognosis tool<ref name="CDAI">Crohn’s Disease Activity Index (CDAI) calculator. CDAI Online Calculator. &lt;ref="http://www.ibdjohn.com/cdai/"Crohn's Disease Activity Index, CDAI (accessed 4 March 2010)</ref>.<br> | |||
== Dietary Management == | |||
Diet is a confusing topic with a lot of conflicting information. Patients need talk with an accredited dietitian to find what’s right for them and their CD.<ref name=":1" /> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
The symptoms above are not specific to Crohn’s disease and have potential to be seen in other conditions. Differential diagnoses can include the following: | The symptoms above are not specific to Crohn’s disease and have potential to be seen in other conditions. Differential diagnoses can include the following: | ||
* | * Infection with amoebas | ||
* [[Behcet Disease|Behcet disease]] | |||
* [[Celiac Disease (Coeliac Disease)|Celiac]] disease | |||
* Intestinal carcinoid | |||
* Intestinal [[tuberculosis]] | |||
* Mesenteric ischemia | |||
* Ulcerative colitis | |||
== Viewing == | |||
*[[ | |||
* | |||
* | |||
* | |||
== | |||
<div class="coursebox"> | <div class="coursebox"> | ||
14 minutes of informative viewing below | |||
{| class="FCK__ShowTableBorders" width="100%" cellspacing="4" cellpadding="4" border="0" | {| class="FCK__ShowTableBorders" width="100%" cellspacing="4" cellpadding="4" border="0" | ||
|- | |- | ||
| Line 327: | Line 142: | ||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
[[Category:Autoimmune Disorders]] | [[Category:Autoimmune Disorders]] | ||
[[Category:Non Communicable Diseases]] | [[Category:Non Communicable Diseases]] | ||
[[Category:Genetic Disorders]] | |||
[[Category:Rheumatology]] | |||
Latest revision as of 16:43, 9 September 2023
Original Editors - Sarah Bailey from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Sarah Bailey, Laura Ritchie, Lucinda hampton, Admin, Kim Jackson, Dave Pariser, Elaine Lonnemann, WikiSysop, Sehriban Ozmen, 127.0.0.1, Wendy Walker and Manisha Shrestha
Introduction[edit | edit source]
Crohn disease (CD) and ulcerative colitis (UC) are both conditions commonly referred to as inflammatory bowel disease (IBD). CD causes chronic inflammation of the gastrointestinal tract. In Crohn disease, the inflammation extends through the entire thickness of the bowel wall from the mucosa to the serosa.
CD is a serious chronic inflammatory disorder that is difficult to diagnose and manage. The disease has a relapsing and remitting course. Many relapses can cause Crohn disease to progress from mild to moderate to severe penetrating (fistulization) or stricturing disease. There is no cure and most patients experience a poor quality of life..[1]
Etiology[edit | edit source]
The cause of CD is not known but genetics seem to play a role as does the environmental affects on the immune system.
The gut bacteria of people with Crohn’s disease changes but it still isn’t clear if the change is caused by inflammation.
Possibly a diet full of highly processed foods like sugary drinks and fast food, may increase the risk of developing Crohn’s. Crohn’s is not infectious. [2]
Epidemiology[edit | edit source]
CD is most prevalent in the western developed world in North America, northern Europe, and New Zealand.
The incidence of CD is bimodal with the onset occurring most frequently between ages 15 to 30 years and 40 to 60 years old.
It is more prominent in urban than rural areas.[1]
Symptoms of Crohn’s Disease[edit | edit source]
While Crohn’s is a chronic disease, the patients will experience bouts of flare ups and remission with the absence of symptoms [3].
Patients with flare-ups of CD usually present with abdominal pain (right lower quadrant), flatulence/bloating, diarrhea (can include mucus and blood), fever, weight loss, anemia. In acute cases, perianal abscess, perianal Crohn disease, and cutaneous fistulas can be seen.[1]
About 50% of individuals with Crohn’s Disease will have mild symptoms. The other half may experience more severe symptoms and pain that appears to come and go. These patients undergo painful exacerbations and potentially symptom free remissions. The remissions might last for months to years but the symptoms will eventually return[3].
The below viewing is a 5 minute presentation from a clients viewpoint.
| [4] |
Types of Crohn's Disease[edit | edit source]
There are different types of Crohn’s Disease dependent upon the location and disease pattern within the GI tract. The different locations of Crohn’s Disease include:
- Gastroduodenal Crohn’s Disease: Located in the upper gastrointenstinal tract and affects the stomach and first part of the small intestine (duodenum). This is uncommon and symptoms occur in 5% of those diagnosed with Crohn’s.
- Jejunoileitis: This is also uncommon in the general population of those diagnosed with Crohn’s disease. Inflammation is located in the Jejunum or Second part of small intestines.
- Ileitis: Inflammation located in the last part of small intestine or ileum and affects 30% of individuals diagnosed with Crohn’s disease.
- Ileocolitis: This is the most common form of Crohn’s disease and affects 50% of those diagnosed with inflammation located in the ileum and colon.
- Crohn’s Colitis: This affects 20% of individuals diagnosed with Crohn’s disease with inflammation located in the colon. The perianal disease and extraintestinal complications are more commonly associated in these individuals.
- Perianal Disease: This occurs in 1/3 of individuals diagnosed with Crohn’s disease. These individuals can have fistulae, fissures, abscesses or skin tags (fleshy growths outside the anus) [6]
Complications[edit | edit source]
CD is a systemic disease and has manifold intestinal and extra-intestinal complications. Examples include:
- Stricture formation, fistulae and abscesses
- Colorectal carcinoma
- Ankylosing spondylitis
- Erythema nodosum, pyoderma gangrenosum
- Kidney and gall stones
- Anemia
- Hypercoagulable state
- Osteoporosis
- Eye inflammation[1]
Diagnosis[edit | edit source]
The diagnosis is made by ruling out other potential causes. Investigations include: blood tests, fecal occult blood test, colonoscopy, flexible sigmoidoscopy, barium enema or small bowel imaging, CT of the GI tract, or a capsule endoscopy.[6]
Many CD patients who develop complications require surgery and possibly multiple procedures in time. Once a patient has had surgery, surveillance endoscopy is recommended in six to 12 months. If there is no endoscopic recurrence, ileocolonoscopy should be repeated in 1 to 3 years.[1]
Treatment/Management[edit | edit source]
The medical treatment is roughly grouped into two classes:
- Mild to moderate disease can be treated by oral mesalamine, immunomodulators, methotrexate, and steroids.
- Moderate to severe disease will be best treated using a combination of immunomodulators and biologics or biologics alone.
- Dietician involvement is recommended and nutritional supplementation are highly recommended before and during the treatment of Crohn disease.
- Poor pregnancy outcomes are associated with active CD. Disease flares should be treated aggressively in pregnancy[7]
- Mental health counseling for may be needed depression
- Sound education about CD and best ways to live with the conditions, for example: Avoid NSAIDs as they may exacerbate disease; Manage mild diarrhea with antidiarrheals; Avoid smoking; heed dietician advice.[1]
Physical Therapy Management[edit | edit source]
Individuals may need physiotherapy to treat the following.
- Crohn’s disease is associated with arthritis, notably arthritis of the lumbar spine and sacroiliac joints. Though arthritis usually affects older people, Crohn's-related arthritis is common in young people with the disease.[8] When a patient presents to physical therapy with low back, sacroiliac or hip pain, it is vital for the therapist to screen for potential organic sources of the pain and for a history of inflammatory bowel disease. See links re treatment.
- CD prevents correct absorption of nutrients through the intestines into the body. Vitamin D and calcium are key nutrients for bone health, and deficiency can lead to osteoporosis. Osteoporosis often leads to insufficiency fractures eg in the vertebrae. Vertebral fractures can cause changes in spinal curvature, leaving other vertebrae more susceptible to fracture. Pain may result from the fracture itself, inflammation and/or biomechanical changes. Educate clients regarding osteoporosis.
- Hydration is very important in patient’s with Crohn’s disease so the therapist should be aware of signs of dehydration when exercising, for example headache, dry lips, disorientation.
- Exercise prescriptions have the ability to boost the immune system, reduce depression, and improve the body image of the patient. In addition to providing this exercise program, therapists can better create coping mechanisms as well as techniques to manage the unexpectedness of Crohn’s Disease[9].
Outcome Measures[edit | edit source]
An outcome measure has been created to track the progress or lack of progress for individuals affected with Crohn’s disease called Crohn’s Disease Activity Index (CDAI). A score below 150 indicates a better prognosis than higher scores. This measure helps to track an individual’s progress from week to week to determine if the symptoms are better or worse. This is more of a gauge of progress and not a prognosis tool[10].
Dietary Management[edit | edit source]
Diet is a confusing topic with a lot of conflicting information. Patients need talk with an accredited dietitian to find what’s right for them and their CD.[2]
Differential Diagnosis[edit | edit source]
The symptoms above are not specific to Crohn’s disease and have potential to be seen in other conditions. Differential diagnoses can include the following:
- Infection with amoebas
- Behcet disease
- Celiac disease
- Intestinal carcinoid
- Intestinal tuberculosis
- Mesenteric ischemia
- Ulcerative colitis
Viewing[edit | edit source]
14 minutes of informative viewing below
 |
Crohn's Disease Pt 1 of 2 |
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Ranasinghe IR, Hsu R. Crohn disease. Available: https://www.ncbi.nlm.nih.gov/books/NBK436021/(accessed 1.10.2022)
- ↑ 2.0 2.1 Crohns and Colitis Australia CD Available:https://crohnsandcolitis.org.au/about-crohns-colitis/crohns-disease/about-crohns-disease/ (accessed 1.10.2022)
- ↑ 3.0 3.1 Crohn’s and Colitis Foundation of America (CCFA). About Crohn’s Disease. http://ccfa.org/info/about/crohns (accessed 4 March 2010)
- ↑ Thomas Craig. A Frank discussion on Crohn's Disease. Available at http://www.youtube.com/watch?v=Npda8xr2G-Y (last accessed 4/510)
- ↑ Crohn’s Disease: Introduction. John Hopkins Medicine. Available at http://www.hopkins-gi.org/GDL_Disease.aspx?CurrentUDV=31&GDL_Disease_ID=291F2209-F8A9-4011-8094-11EC9BF3100E&GDL_DC_ID=D03119D7-57A3-4890-A717-CF1E7426C8BA (accessed 5 April 2010).
- ↑ 6.0 6.1 6.2 Cheifetz Adam, Moss Alan, Peppercorn Mark. Crohn’s Disease. Knol Beta. Available at http://knol.google.com/k/crohn-s-disease#. Accessed 5 April 2010.
- ↑ Kalla R, Ventham NT, Satsangi J, Arnott ID. Crohn’s disease. Bmj. 2014 Nov 19;349. Available:https://www.bmj.com/content/349/bmj.g6670 (accessed 1.10.2022)
- ↑ Enzine articles The Link Between Crohn's Disease And Lower Back Pain Available:https://ezinearticles.com/?The-Link-Between-Crohns-Disease-And-Lower-Back-Pain&id=7654760 (accessed 1.10.2022)
- ↑ Goodman CC, Fuller KS. Pathophysiology: Implications for the Physical Therapist. 3rd ed. St. Louis, MO: Saunders-Elsevier; 2009.
- ↑ Crohn’s Disease Activity Index (CDAI) calculator. CDAI Online Calculator. <ref="http://www.ibdjohn.com/cdai/"Crohn's Disease Activity Index, CDAI (accessed 4 March 2010)