Coccyx Fractures: Difference between revisions
Kim Jackson (talk | contribs) (Created page with "<div class="editorbox">'''Original Editors ''' User Name '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> == Definition...") |
Rosie Swift (talk | contribs) (Added to treatment) |
||
| (11 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editors ''' [[User: | <div class="editorbox">'''Original Editors ''' [[User:Lucinda_hampton|Lucinda hampton]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
[[File:Coccyx - animation02.gif|right|frameless|200x200px]] | |||
A coccyx [[fracture]] is a break in the tailbone. This is the lowest part of the spine. A fractured coccyx can be a very [[Pain Mechanisms|painful]] acute or chronic ordeal and may not resolve for a long duration. Furthermore, due to the nature of the coccyx structure, many tailbone fractures are not immediately diagnosed. The coccyx can be composed of several sections of 2 or more bones each. This segmented anatomy can conceal minor fractures occurring at natural bone faults and make positive diagnosis of a break difficult without prior imaging studies available.<ref name=":0">[https://www.cure-back-pain.org/fractured-coccyx.html Types of fractured coccyx]. The Back Pain Authority. Available from: https://www.cure-back-pain.org/fractured-coccyx.html (last accessed 4.12.2019)</ref> | |||
This page should be read alongside our [[Coccygodynia (Coccydynia, Coccalgia, Tailbone Pain)|Coccydynia]] page. Coccydynia is a term used to describe a painful coccyx. Individuals who have experienced direct trauma to the coccyx and a suspected or confirmed fracture, may also experience Coccydynia. | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
[[File:Coccyx.png|right|frameless|599x599px]] | |||
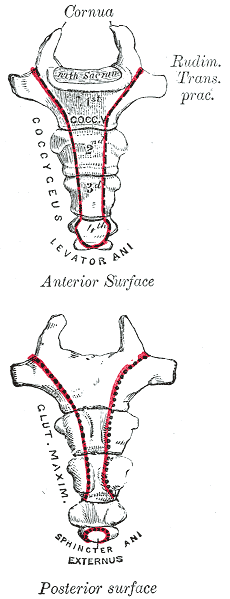
The coccyx is a triangular bone consisting of three to five segments: the first and largest of these vertebral segments articulates with the [[sacrum]] (see image). The last three segments diminish in size and usually form a single piece of bone. The anterior surface presents three transverse grooves indicating the lines of fusion of these segments. Attached to the anterior surface are the anterior sacrococcygeal ligaments and the fibres of the levator ani muscle. On either side of the posterior surface are the coccygeal cornua, which articulate with the cornua of the sacrum to form the posterior sacral foramen, occupied by the posterior division of the fifth sacral nerve. The flattened lateral edge of the first segment of the coccyx ascends to join the similar border of the last sacral vertebra, thereby completing the fifth anterior sacral foramen, which accommodates the anterior division of the fifth sacral nerve. The lateral borders of the coccyx are very thin and provide attachments to the sacrosciatic ligaments and attachments for the coccygeus muscles anterior to the ligaments and fibres of the gluteus maximus posterior to the ligaments. The tendon of the iliococcygeus muscle attaches to the tip of the coccyx, protecting the rectum and supporting it via the coccyx<ref>Nathan ST, Fisher BE, Roberts CS. [https://online.boneandjoint.org.uk/doi/full/10.1302/0301-620X.92B12.25486 Coccydynia: a review of pathoanatomy, aetiology, treatment and outcome]. The Journal of bone and joint surgery. British volume. 2010 Dec;92(12):1622-7. Available from: https://online.boneandjoint.org.uk/doi/full/10.1302/0301-620X.92B12.25486 (last accessed 4.12.2019)</ref>. | |||
== Aetiology and Risk Factors == | |||
External trauma causing a fracture usually occurs due to a backward [[Falls|fall]] on the buttock eg a fall off the stairs on the tailbone, or by an impact directly applied to coccyx. | |||
== | The location of the coccyx makes it particularly susceptible to internal injury, including fractures, during childbirth, especially during a difficult or instrumented delivery. <ref name=":1">Lirette LS, Chaiban G, Tolba R, Eissa H. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3963058/ Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain.] Ochsner Journal. 2014 Mar 20;14(1):84-7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3963058/ (last accessed 4.12.2019)</ref> Childbirth is rarely responsible for actually causing a fracture of the tailbone. The possibility exists, but more often, birth-related coccyx pain is the result of bruising, rather than fracture<ref name=":0" /> | ||
Fracture | Fracture can also occur from repetitive or prolonged sitting on hard, narrow, or uncomfortable surfaces, particularly with [[Osteoporotic Vertebral Fractures|osteoporotic]] bones. | ||
Risk factors include | |||
* Having a health problem that may result in falls, such as weak [[Muscle|muscles]] | |||
* Having a health problem that may weaken bones, such as [[osteoporosis]] | |||
* Playing contact sports, such as hockey<ref name=":2">Winchester Hospital [https://www.winchesterhospital.org/health-library/article?id=11953 Coccyx fracture] Available from: https://www.winchesterhospital.org/health-library/article?id=11953 (last accessed 4.12.2019)</ref> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
* The classic presentation of a coccyx fracture is localized pain over the coccyx. | |||
* Patients present complaining of “tailbone pain.” | |||
* The pain will usually be worse with prolonged sitting, leaning back while seated, prolonged standing, and rising from a seated position. | |||
* Pain may also be present with sexual intercourse or defecation. | |||
* History may be significant for a recent trauma with an acute onset of pain, or the onset of pain may have been insidious with no clear inciting factor. Physical examination will reveal tenderness over the coccyx.<ref name=":1" /> | |||
== Differential Diagnosis == | |||
Other causes of coccyx pain should be ruled out, looking out for [[The Flag System|red flags]]. | |||
* Infection aetiologies (eg, pilonidal cyst), | |||
* Masses in region | |||
* Pelvic floor muscle spasms | |||
* Sacrococcygeal joint hypermobility or hypomobility with degenerative changes causing pain | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Can include: | |||
A rectal examination by a qualified health professional (grasps the coccyx between the forefinger and thumb and by moving it, they can tell if there's too much or too little mobility in the coccyx). The normal range of motion is about 13 degrees. Too much more or too much less, can be a sign of a problem. | |||
< | [[X-Rays|X-rays]] are done in both standing and sitting positions. Comparing the angle of the coccyx in the two positions helps your doctor determine the degree of motion.<ref>Healthline [https://www.healthline.com/health/broken-tailbone#symptoms Fracture coccyx] Available from: https://www.healthline.com/health/broken-tailbone#symptoms (last accessed 4.12.2019)</ref> | ||
== | == Medical Management == | ||
The fracture will need time to heal on its own. This can take eight to twelve weeks. Medicine can help ease pain and swelling. | |||
Treatment may include: | |||
* [[Therapeutic Corticosteroid Injection|Steroid Injections]] | |||
* Surgery for this injury is rare. It may be done to remove the coccyx when all other options have been tried.<ref name=":2" /> Coccyx repair surgery may be indicated for complex fractures involving surrounding tissue damage or compound fractures where the bone might break through the skin. These cases are rare and represent the gross exception to the normally experienced minor cracks seen in most tailbone fractures. | |||
* Coccyx removal surgery can be a treatment for a badly damaged coccyx, but is more often used for patients with long-term chronic coccyx pain conditions.<ref name=":0" /> | |||
= | |||
< | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
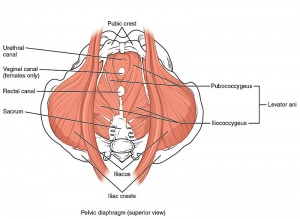
Treatment can include<ref name=":1" />:[[File:Pelvic Floor Muscles.jpg|right|frameless]] | |||
* Modified wedge-shaped cushions (coccygeal cushions) can relieve the pressure on the coccyx while the patient is seated | |||
* Training patients to adopt proper sitting posture ensures that weight in distributed through the ischial tuberosities, therefore decreasing the pressure transmitting through the coccyx. | |||
* Modified activities of daily living<ref name=":3">Livingstone L. Post-natal management in: Sapsford R, Bullock-Saxton J, Markwell S. Women’s health: a textbook for physiotherapists. WB Saunders Co. Ltd., London1998: 220-246</ref>, specifically: side-lying/ crawling technique for getting in and out of bed; side-lying/ prone-lying for resting; avoiding forward flexion techniques for lifting | |||
* The application of heat and cold over the site also may be beneficial. | |||
* Exercises that stretch the ligaments and strengthen the muscles supporting the lower spine. | |||
* Pelvic floor exercises, with particular focus on the relaxation of Levator ani | |||
* Use of TENS | |||
* Topical NSAIDs application. Studies have shown that these preparations are useful for other painful conditions such as osteoarthritis. Topical creams are generally well tolerated and can be associated with fewer systemic side effects than oral medications. | |||
* Advice on bowel habits: staying hydrated and consuming fibre to prevent constipation; adopting a optimal posture for emptying bowels completely<ref name=":3" />. | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category: | [[Category:Vrije_Universiteit_Brussel_Project]] | ||
[[Category:Fractures]] | [[Category:Fractures]] | ||
Latest revision as of 10:15, 20 May 2022
Top Contributors - Kim Jackson, Lucinda hampton, Rosie Swift and Admin
Introduction[edit | edit source]
A coccyx fracture is a break in the tailbone. This is the lowest part of the spine. A fractured coccyx can be a very painful acute or chronic ordeal and may not resolve for a long duration. Furthermore, due to the nature of the coccyx structure, many tailbone fractures are not immediately diagnosed. The coccyx can be composed of several sections of 2 or more bones each. This segmented anatomy can conceal minor fractures occurring at natural bone faults and make positive diagnosis of a break difficult without prior imaging studies available.[1]
This page should be read alongside our Coccydynia page. Coccydynia is a term used to describe a painful coccyx. Individuals who have experienced direct trauma to the coccyx and a suspected or confirmed fracture, may also experience Coccydynia.
Clinically Relevant Anatomy[edit | edit source]
The coccyx is a triangular bone consisting of three to five segments: the first and largest of these vertebral segments articulates with the sacrum (see image). The last three segments diminish in size and usually form a single piece of bone. The anterior surface presents three transverse grooves indicating the lines of fusion of these segments. Attached to the anterior surface are the anterior sacrococcygeal ligaments and the fibres of the levator ani muscle. On either side of the posterior surface are the coccygeal cornua, which articulate with the cornua of the sacrum to form the posterior sacral foramen, occupied by the posterior division of the fifth sacral nerve. The flattened lateral edge of the first segment of the coccyx ascends to join the similar border of the last sacral vertebra, thereby completing the fifth anterior sacral foramen, which accommodates the anterior division of the fifth sacral nerve. The lateral borders of the coccyx are very thin and provide attachments to the sacrosciatic ligaments and attachments for the coccygeus muscles anterior to the ligaments and fibres of the gluteus maximus posterior to the ligaments. The tendon of the iliococcygeus muscle attaches to the tip of the coccyx, protecting the rectum and supporting it via the coccyx[2].
Aetiology and Risk Factors[edit | edit source]
External trauma causing a fracture usually occurs due to a backward fall on the buttock eg a fall off the stairs on the tailbone, or by an impact directly applied to coccyx.
The location of the coccyx makes it particularly susceptible to internal injury, including fractures, during childbirth, especially during a difficult or instrumented delivery. [3] Childbirth is rarely responsible for actually causing a fracture of the tailbone. The possibility exists, but more often, birth-related coccyx pain is the result of bruising, rather than fracture[1]
Fracture can also occur from repetitive or prolonged sitting on hard, narrow, or uncomfortable surfaces, particularly with osteoporotic bones.
Risk factors include
- Having a health problem that may result in falls, such as weak muscles
- Having a health problem that may weaken bones, such as osteoporosis
- Playing contact sports, such as hockey[4]
Characteristics/Clinical Presentation[edit | edit source]
- The classic presentation of a coccyx fracture is localized pain over the coccyx.
- Patients present complaining of “tailbone pain.”
- The pain will usually be worse with prolonged sitting, leaning back while seated, prolonged standing, and rising from a seated position.
- Pain may also be present with sexual intercourse or defecation.
- History may be significant for a recent trauma with an acute onset of pain, or the onset of pain may have been insidious with no clear inciting factor. Physical examination will reveal tenderness over the coccyx.[3]
Differential Diagnosis[edit | edit source]
Other causes of coccyx pain should be ruled out, looking out for red flags.
- Infection aetiologies (eg, pilonidal cyst),
- Masses in region
- Pelvic floor muscle spasms
- Sacrococcygeal joint hypermobility or hypomobility with degenerative changes causing pain
Diagnostic Procedures[edit | edit source]
Can include:
A rectal examination by a qualified health professional (grasps the coccyx between the forefinger and thumb and by moving it, they can tell if there's too much or too little mobility in the coccyx). The normal range of motion is about 13 degrees. Too much more or too much less, can be a sign of a problem.
X-rays are done in both standing and sitting positions. Comparing the angle of the coccyx in the two positions helps your doctor determine the degree of motion.[5]
Medical Management[edit | edit source]
The fracture will need time to heal on its own. This can take eight to twelve weeks. Medicine can help ease pain and swelling.
Treatment may include:
- Steroid Injections
- Surgery for this injury is rare. It may be done to remove the coccyx when all other options have been tried.[4] Coccyx repair surgery may be indicated for complex fractures involving surrounding tissue damage or compound fractures where the bone might break through the skin. These cases are rare and represent the gross exception to the normally experienced minor cracks seen in most tailbone fractures.
- Coccyx removal surgery can be a treatment for a badly damaged coccyx, but is more often used for patients with long-term chronic coccyx pain conditions.[1]
Physical Therapy Management[edit | edit source]
Treatment can include[3]:
- Modified wedge-shaped cushions (coccygeal cushions) can relieve the pressure on the coccyx while the patient is seated
- Training patients to adopt proper sitting posture ensures that weight in distributed through the ischial tuberosities, therefore decreasing the pressure transmitting through the coccyx.
- Modified activities of daily living[6], specifically: side-lying/ crawling technique for getting in and out of bed; side-lying/ prone-lying for resting; avoiding forward flexion techniques for lifting
- The application of heat and cold over the site also may be beneficial.
- Exercises that stretch the ligaments and strengthen the muscles supporting the lower spine.
- Pelvic floor exercises, with particular focus on the relaxation of Levator ani
- Use of TENS
- Topical NSAIDs application. Studies have shown that these preparations are useful for other painful conditions such as osteoarthritis. Topical creams are generally well tolerated and can be associated with fewer systemic side effects than oral medications.
- Advice on bowel habits: staying hydrated and consuming fibre to prevent constipation; adopting a optimal posture for emptying bowels completely[6].
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Types of fractured coccyx. The Back Pain Authority. Available from: https://www.cure-back-pain.org/fractured-coccyx.html (last accessed 4.12.2019)
- ↑ Nathan ST, Fisher BE, Roberts CS. Coccydynia: a review of pathoanatomy, aetiology, treatment and outcome. The Journal of bone and joint surgery. British volume. 2010 Dec;92(12):1622-7. Available from: https://online.boneandjoint.org.uk/doi/full/10.1302/0301-620X.92B12.25486 (last accessed 4.12.2019)
- ↑ 3.0 3.1 3.2 Lirette LS, Chaiban G, Tolba R, Eissa H. Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain. Ochsner Journal. 2014 Mar 20;14(1):84-7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3963058/ (last accessed 4.12.2019)
- ↑ 4.0 4.1 Winchester Hospital Coccyx fracture Available from: https://www.winchesterhospital.org/health-library/article?id=11953 (last accessed 4.12.2019)
- ↑ Healthline Fracture coccyx Available from: https://www.healthline.com/health/broken-tailbone#symptoms (last accessed 4.12.2019)
- ↑ 6.0 6.1 Livingstone L. Post-natal management in: Sapsford R, Bullock-Saxton J, Markwell S. Women’s health: a textbook for physiotherapists. WB Saunders Co. Ltd., London1998: 220-246