Coccygodynia (Coccydynia, Coccalgia, Tailbone Pain)
Original Editor - Maxime Tuerlinckx as part of the Vrije Universiteit Brussel's Evidence-based Practice project
Top Contributors - Victoria Geropoulos, Maxime Tuerlinckx, Nicole Hills, Evan Thomas, Kim Jackson, Vidya Acharya, Redisha Jakibanjar, Admin, Daphne Jackson, Rosie Swift, Pacifique Dusabeyezu, Laura Ritchie, WikiSysop and Aminat Abolade
Definition[edit | edit source]
Coccygodynia, sometimes referred to as coccydynia, coccalgia, coccygeal neuralgia or tailbone pain, is the term used to describe the symptoms of pain that occur in the region of the coccyx.[1][2][3][4] The pain is most commonly triggered in a sitting position, but may also occur when the individual changes from a sitting to standing position.[3] Most cases will resolve within a few weeks to months, however for some patients the pain can become chronic, having negative impacts on quality of life.[3][4] For these individuals, management can be difficult due to the complex nature of coccygeal pain.[4]
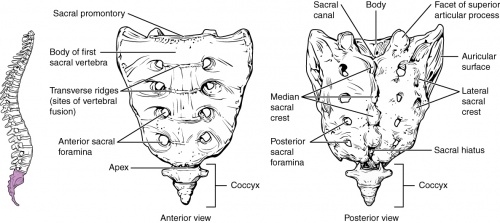
Clinically Relevant Anatomy[edit | edit source]
The coccyx is a triangular bone that forms the most distal segment of the spine.[1][3] It is composed of 3 to 5 coccygeal segments.[2] These segments fuse together to form a single bone, with the exception of the first coccygeal segment.[2][3] The first coccygeal segment might not fuse together with the second coccygeal segment.[2][3]The ventral aspect of the coccyx is concave in shape, while the dorsal aspect of the coccyx is convex in shape.[1]The first coccygeal segment is composed of articular processes that form the coccygeal cornua.[1][2][4] The coccygeal cornua articulates with the sacral cornua of the inferior sacral apex of S5.[1][2][4] This articulation creates a symphysis or synovial joint, which forms one of the borders of the foramen for the dorsal branch of the fifth sacral nerve route (S5).[1][4]
The coccyx serves as an attachment site for several muscles and ligaments.[4] Anteriorly, the coccyx is bordered by the levator ani muscle and the sacro-coccygeal ligament.[4] In an anterior (front) to posterior (back) direction, the lateral border of the coccyx serves as an insertion point for the coccygeal muscles, the sacrospinous ligament, the sacrotuberous ligament and the gluteus maximus.[4] Inferiorly, the tendon of the iliococcygeus muscle inserts onto the tip of the coccyx.[4]Together, these ligaments and muscles contribute to voluntary bowel control, as well, provide support to the pelvic floor.[4]
In addition to being an insertion site, the coccyx, in conjunction with the ischial tuberosities, provides weight-bearing support to an individual in a seated position.[4] For this reason, increased stress and pressure can be placed on the coccyx while a person leans back in a seated position.[4] The coccyx also functions in providing support to the anus.[4]
Postascchini and Massobrio (1983)[5] classified the variations in morphology of the coccyx into four different configurations:[5]
- Type I: The coccyx is slightly curved forward, with its apex positioned downward.[5]
- Type II: The forward curvature of the coccyx is more exaggerated, with the apex positioned in a straightforward direction.[5]
- Type III: Sharp angulation of the coccyx forward.[5]
- Type IV: Subluxation of the coccyx at the sacrococcygeal or intercoccygeal joint.[5]
Epidemiology and Etiology[edit | edit source]
Currently, the incidence of coccygodynia is unknown.[4] Certain factors can increase an individual's risk for developing coccygodynia, such as body mass, age, gender.[1][4] With obesity, the coccyx is more vulnerable to increases in intrapelvic pressure while sitting, increasing the risk of posterior subluxation (displacement backward) of the coccyx.[1][6] With rapid weight loss, the cushioning around the coccyx may be lost,[4] and the coccyx is at an increased risk for anterior subluxation (displacement forward).[1][6] The risk of coccygodynia is 5 times higher in females than it is in males[4], which may be a result of the increased pressure that occurs during pregnancy and delivery.[7] Furthermore, adults and adolescents are more likely to present with coccygodynia than children.[4][6]
Coccygodynia may be classified as post-traumatic, non-traumatic or idiopathic.[3][4] Post-traumatic coccygodynia is usually a result of internal or external trauma.[4] For example, external trauma could result from a backwards fall that might dislocate or break the coccyx,[4][8] and internal trauma could result from a difficult childbirth or a childbirth with an assistive delivery.[4] Minor trauma, such as repetitive sitting on hard surfaces can also lead to coccygodynia.[4][9] Non-traumatic coccygodynia can result from degenerative disc disease, hyper and/or hypo-mobility of the sacrococcygeal joint, infectious diseases and different variations in the configuration of the coccyx.[4] Type II, III, and IV configurations typically cause more pain than type I configurations.[1][5] Postacchini and Massobrio (1983)[5] stated that individuals with coccygodynia are more likely than the general population to have a configuration of Type II,III and IV.[5] Idiopathic coccygodynia occurs in the absence of any pathology in the coccyx.[1] This is typically a diagnosis of exclusion, and may result from spasticity or other abnormalities that affect the musculature of the pelvic floor.[1] For example, over-extension of the levator ani muscle can shift the coccyx into an abnormal position.[10]
Clinical Presentation[edit | edit source]
The most common complaint of coccygodynia is pain in and around the coccyx without any reports of severe low back pain or radiating pain.[1][2] The pain is typically localised to the sacrococcygeal joint[2] and is described as a “pulling” or “cutting” sensation.[3] Individuals will commonly report tenderness on palpation of the coccyx.[1][2]
Patients will usually exhibit a guarding seated posture, whereby one buttock will be elevated to take weight off of the coccyx.[3] Pain is usually exacerbated with repeated sitting or with transition from sitting to standing position.[1][2] Individuals will report that pain is alleviated with sitting on the legs or buttock.[2] Patients may also report pain with defecation or the frequent need to defecate.[1][2] Other complaints may include pain with coughing or increased pain during menstruation in females.[7][11]
Although not a hallmark sign of coccygodynia, low back pain may still arise in individuals with coccygodynia due to the morphological variations in the shape of the coccyx and it’s forward curvature.[1][2][5]
Diagnosis[edit | edit source]
Physical Exam[edit | edit source]
Palpation over the sacrococcygeal joint will display tenderness.[1][3][4] The coccyx should also be palpated to detect the presence of swelling, bone spicules or fragments, and coccygeal masses.[1][2] The soft tissues around the coccyx should be examined for the presence of pilonidal cysts (in-grown hairs).[1][2]
Palpating the coccyx can be used to differentiate between true coccygodynia, which is localised pain over the area of the coccyx, and pseudo coccygodynia, which is characterised by pain that is referred to the coccygeal area from visceral organs, a peripheral nerve, nerve root or plexus.[3] If referred pain is present, pain will radiate around the buttocks, thigh and back, and reports of pain will be present with lumbar movements.[7][11] Referred pain may also be indicative of psychogenic coccygodynia, in which pain will be more diffuse and pain will be experienced with lumbar and hip movements.[7][11]
Increased pain may also be reported during a straight leg raise test.[7][11]
Upon rectal examination, pain will be present when the tip of the coccyx is manipulated.[1][2]An internal mass, referred to as a chordoma, might also be present on the anterior surface of the sacrum.[2]
Imaging[edit | edit source]
Although primarily a clinical diagnosis, dynamic radiographs can be used in diagnosis.[1][2] Dynamic radiographs taken in both sitting and standing positions can provide measurements of coccygeal displacement.[2] Single-position radiographs are usually not used for diagnosis as they are unable to identify any morphological differences between individuals with and without coccygodynia.[1][2][5] Radiographs are usually taken if the pain persists for a duration that is greater than 8 weeks.[2]
Differential Diagnosis[edit | edit source]
The following differential diagnoses should be ruled out:[3][12]
- Coccyx fracture
- Lumbar spondylosis or disc herniation
- Levator ani syndrome
- Piriformis syndrome
- Descending perineal syndrome
- Perianal abscess
- Rectal tumour or teratoma
- Aclock canal syndrome
- Proctalgia Fugax
Outcome Measures[edit | edit source]
Pain Measures[edit | edit source]
- 4-Item Pain Intensity Measure (P4)
- Brief Pain Inventory - Short Form
- Numeric Pain Rating Scale
- Short-form McGill Pain Questionnaire
- Visual Analogue Scale
Level of Function in Activities of Daily Living[edit | edit source]
Condition Specific[edit | edit source]
Management[edit | edit source]
Conservative or non-surgical treatments are typically the gold standard when treating coccygodynia, being successful for 90% of cases.[1][2][3][4] Non-operative treatments may range from the recommendation of non-steroidal anti-inflammatory drugs (NSAIDs), activity modification, ergonomic adjustments, and physical therapy.[1][2][3][4] Surgery is usually only considered when patients continue to complain of coccygeal pain after the use of conservative treatments.[1][2][3][4]A coccygectomy, which is the removal of a section or all of the coccyx, is the most common surgical treatment performed.[1][2][3][4]
Physical Therapy Management[edit | edit source]
Ergonomic Adjustments[edit | edit source]
The initial goal of treatment should be focused on providing postural education.[13] Individuals should be taught to correct their sitting posture by sitting more erectly on a firm chair.[13][14] A proper sitting posture ensures weight is taken off the coccyx and is instead loaded onto the ischial tuberosities and the thighs.[13][14] Patients should be advised to avoid any positions or movements that might exacerbate their symptoms.[13]
Physiotherapists may also recommend the use of cushions. Modified wedge-shaped cushions (coccygeal cushions), which can be purchased over the counter, help to relieve the pressure placed on the coccyx during sitting.[4] Donut shaped or circular cushions may also be used.[3][4][13] Donut shaped cushions may actually increase pressure over the coccyx, but are more beneficial for rectal pain.[4]The use of cushions can be recommended over a 6-8 week period.[13] Although commonly recommended, the therapeutic outcomes of these conservative recommendations have not been evaluated in the literature.[13]
Manual Therapy[edit | edit source]
The manual therapy techniques suggested in the literature range from massage, stretching, mobilisation and manipulation, and may either involve internal or external contact with the coccyx.[2][15]
Internal techniques may include massage of the levator ani muscle or the coccygeus muscle,[15][16] joint mobilisation while the coccyx is hyperextended to stretch the levator ani,[15][17][18] or repeated mobilisations while the coccyx is rotated.[15][19]
External techniques may include manipulations of either the coccyx or sacroiliac joint,[15][20][21][22] mobilisations of the sacrococcygeal or intercoccygeal joints,[19] posterior mobilisations to the thoracic spine,[23] and stretching of the piriformis or iliopsoas.[23]Including thoracic spine mobilisations can help address compensatory patterns that affect the entire spine and pelvis, potentially influencing coccygeal pain. Additionally, mobilisations focusing on the lumbar spine are also beneficial as this area has a more direct relationship with pelvic tilt and alignment, impacting the position and stress on the coccyx.
The technique chosen will vary depending on what the originating cause of the coccygodynia is.[15] For example, massage or stretching of the levator ani might be chosen if the underlying cause is due to spasm of the pelvic floor musculature.[15][16][18] . Mobilisation techniques may be the preferred technique when the goal of treatment is to increase coccygeal mobility.[15][19]Manipulation techniques are helpful when the goal of treatment is to improve extension of the coccyx.[15][20]
A study by Maigne and Chatellier (2001)[15], who compared the effectiveness of various massage, mobilisation and manipulation techniques, reported that manual treatments were helpful for ~ 26% of cases with coccygodynia at 6 months and ~ 24% of the cases of coccygodynia at 2 years post treatment.[15] The findings of this study also reported that massage and stretching techniques of the levator ani muscle were more effective than joint mobilisation techniques.[15]
In support of manipulation, Maigne and colleagues (2006)[24] reported mild effectiveness of intrarectal manipulation in managing chronic coccygodynia when compared to shortwave diathermy.[24] Chakraborty (2012)[25] reported that combined manipulation and corticosteroid injection was more effective in treating coccygodynia than either technique alone.[25]
Mohanty and Pattnaik (2017)[23] reported that individuals with coccygodynia may benefit from stretching of the piriformis or iliopsoas muscles.[23] In this study, piriformis and iliopsoas stretches, as well as Maitland’s mobilisation of hypomobile thoracic spine, had a beneficial effect in increasing pain free sitting duration and pressure pain threshold.[23] Tightness of either the piriformis or iliopsoas can cause excessive anterior tilting of the pelvis and consequently place an excessive load on the coccyx.[23] Stretching these muscles can help to correct the load that is placed on the coccyx.[23] By increasing thoracic extension, thoracic mobilisations may also help to reduce the load on the coccyx.[23]In this study, stretching was performed for 2 minutes on each side of the hip, 5 times per week.[23]
Based on the work of Maigne and chatellier (2001)[15] and Wray (1991),[26]Fogel and Colleagues (2004)[2] designed a treatment algorithm for coccygodynia. When a patient is presenting with acute coccygodynia (less than 2 months in duration), 8 weeks of rest and adjustable seating should be recommended in conjunction with stool softener and NSAIDs.[2] When a patient presents with chronic coccygodynia (greater than 2 months in duration), massage and stretching techniques should be initiated in conjunction with corticosteroid injections.[2]
Physical Modalities[edit | edit source]
Lin and colleagues (2015)[27], who compared the benefits of extracorporeal shockwave therapy (ESWT) with other physical modalities, reported that ESWT was more effective in decreasing visual analogue scale pain scores than shortwave diathermy and IFC.[27] Patients who received ESWT reported greater subjective satisfaction scores following treatment, with ~ 70% reporting good to excellent satisfaction.[27] In this study, 2000 shots of ESWT were applied to the coccyx area per session for 4 sessions at 5 Hz and a pressure of 3-4 bar.[27]The findings of this study can be supported by a case report by Marwan and colleagues (2014)[28], who reported the effectiveness of ESWT to relieve pain over 3 sessions in 2 cases of coccygodynia.[28] A quasi-experimental study by Haghighat and Mashayekhi (2016),[29] involving 10 patients with cocycgodynia, stated that ESWT significantly decreased visual analogue scale pain scores at 4 weeks and 2 months post treatment.[29] ESWT was delivered to the coccygeal area at 3000 shock waves per session, with a frequency of 21 Hz and pressure of 2 bar.[29]
Although the mechanism is still being debated in the literature, it is proposed that ESWT decreases the inflammatory response and the expression of inflammatory mediators present in coccygodynia through the induction of neovascularisation.[27][29]
When considering the effects of other modalities, Lin and Colleagues (2015)[27] reported that IFC and shortwave diathermy were able to decrease pain scores but not to the same extent as ESWT.[27] Wray and colleagues (1991)[26] reported minimal benefits with a combined treatment of ultrasound and shortwave diathermy. After receiving 2 weeks of ultrasound and 2 weeks of shortwave diathermy, only 16% of patients in the study report relief in their symptoms.[26] Given these discrepancies, more evidence regarding which modalities provide the greatest benefit to patients with coccygodynia.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 Patel R, Appannagari A, Whang PG. Coccydynia. Current reviews in musculoskeletal medicine. 2008 Dec;1(3):223-6.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 2.25 2.26 2.27 2.28 Fogel GR, Cunningham III PY, Esses SI. Coccygodynia: evaluation and management. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2004 Jan 1;12(1):49-54.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 Kerr EE, Benson D, Schrot RJ. Coccygectomy for chronic refractory coccygodynia: clinical case series and literature review. Journal of Neurosurgery: Spine. 2011 May 1;14(5):654-63.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 4.23 4.24 4.25 4.26 4.27 4.28 4.29 4.30 4.31 4.32 Lirette LS, Chaiban G, Tolba R, Eissa H. Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain. Ochsner Journal. 2014 Mar 20;14(1):84-7.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 Postacchini FR, Massobrio MA. Idiopathic coccygodynia. Analysis of fifty-one operative cases and a radiographic study of the normal coccyx. The Journal of bone and joint surgery. American volume. 1983 Oct 1;65(8):1116-24.
- ↑ 6.0 6.1 6.2 Maigne JY, Doursounian L, Chatellier G. Causes and mechanisms of common coccydynia: role of body mass index and coccygeal trauma. Spine. 2000 Dec 1;25(23):3072-9.
- ↑ 7.0 7.1 7.2 7.3 7.4 Ombregt L, Bisschop P, ter Veer JH. A System of Orthopaedic Medicine. Elsevier Science Limited, 2003, p.968-969.
- ↑ Schapiro S. Low back and rectal pain from an orthopedic and proctologic viewpoint with a review of 180 cases. The American Journal of Surgery. 1950 Jan 1;79(1):117-28.
- ↑ Pennekamp PH, Kraft CN, Stütz A, Wallny T, Schmitt O, Diedrich O. Coccygectomy for coccygodynia: does pathogenesis matter?. Journal of Trauma and Acute Care Surgery. 2005 Dec 1;59(6):1414-9.
- ↑ Maigne R. Douleurs d’origine vertébrale et traitements par manipulations, medicine orthopédique des derangements intervertébraux mineurs, 2e editie, p. 473-476.
- ↑ 11.0 11.1 11.2 11.3 Gregory P. Grieve, De wervelkolom, veel voorkomende aandoeningen (The spine), 1984, p. 320-321.
- ↑ Schrot RJ. Coccygodynia. Epocrates Online (https://online. epocrates. com/u/29411067/Coccygodynia)[Accessed December 15 2010] Search Google Scholar Export Citation. 2010.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 Chiarioni G, Asteria C, Whitehead WE. Chronic proctalgia and chronic pelvic pain syndromes: new etiologic insights and treatment options. World Journal of Gastroenterology: WJG. 2011 Oct 28;17(40):4447.
- ↑ 14.0 14.1 Thiele GH. Coccygodynia: cause and treatment. Diseases of the Colon & Rectum. 1963 Nov;6(6):422-36.
- ↑ 15.00 15.01 15.02 15.03 15.04 15.05 15.06 15.07 15.08 15.09 15.10 15.11 15.12 Maigne JY, Chatellier G. Comparison of three manual coccydynia treatments: a pilot study. Spine. 2001 Oct 15;26(20):E479-83.
- ↑ 16.0 16.1 Thiele GH. Coccygodynia and pain in the superior gluteal region: and down the back of the thigh: causation by tonic spasm of the levator ani, coccygeus and piriformis muscles and relief by massage of these muscles. Journal of the American Medical Association. 1937 Oct 16;109(16):1271-5.
- ↑ Maigne R, Nieves WL. Diagnosis and treatment of pain of vertebral origin. CRC Press; 2005 Sep 1.
- ↑ 18.0 18.1 Maigne R. Les Manipulations Vertébrales. 3rd ed. Paris: Expansion Scientifique Française, 1961: 180.
- ↑ 19.0 19.1 19.2 Mennell JB. The science and Art of Joint Manipulation. London: Churchill, 1952.
- ↑ 20.0 20.1 Bergmann TF, Petersen DH, Lawrence DJ. Chiropractic Technique-Principals and Procedures. New York: Churchill Livingston Inc. 803p. ISBN 0-443-0872-0; 1993.
- ↑ Polkinghorn BS, Colloca CJ. Chiropractic treatment of coccygodynia via instrumental adjusting procedures using activator methods chiropractic technique. Journal of manipulative and physiological therapeutics. 1999 Jul 1;22(6):411-6.
- ↑ Plaugher G, editor. Textbook of clinical chiropractic: a specific biomechanical approach. Williams & Wilkins; 1993.
- ↑ 23.0 23.1 23.2 23.3 23.4 23.5 23.6 23.7 23.8 Mohanty PP, Pattnaik M. Effect of stretching of piriformis and iliopsoas in coccydynia. Journal of bodywork and movement therapies. 2017 Jul 1;21(3):743-6.
- ↑ 24.0 24.1 Maigne JY, Chatellier G, Le Faou M, Archambeau M. The treatment of chronic coccydynia with intrarectal manipulation: a randomized controlled study. Spine. 2006 Aug 15;31(18):E621-7.
- ↑ 25.0 25.1 Chakraborty S. Nonoperative Management of Coccydynia: A Comparative Study Comparing Three Methods. The Spine Journal. 2012 Sep 1;12(9):S69-70.
- ↑ 26.0 26.1 26.2 Wray CC, Easom S, Hoskinson J. Coccydynia. Aetiology and treatment. The Journal of Bone and Joint Surgery. British volume. 1991 Mar;73(2):335-8.
- ↑ 27.0 27.1 27.2 27.3 27.4 27.5 27.6 Lin SF, Chen YJ, Tu HP, Lee CL, Hsieh CL, Wu WL, Chen CH. The effects of extracorporeal shock wave therapy in patients with coccydynia: a randomized controlled trial. PloS one. 2015 Nov 10;10(11):e0142475.
- ↑ 28.0 28.1 Marwan Y, Husain W, Alhajii W, Mogawer M. Extracorporeal shock wave therapy relieved pain in patients with coccydynia: a report of two cases. The Spine Journal. 2014 Jan 1;14(1):e1-4.
- ↑ 29.0 29.1 29.2 29.3 Haghighat S, Asl MM. Effects of extracorporeal shock wave therapy on pain in patients with chronic refractory coccydynia: A quasi-experimental study. Anesthesiology and pain medicine. 2016 Aug;6(4).