Pelvic Floor Distress Inventory (PFDI - 20)
Original Editor - Kirsten Ryan
Top Contributors - Kirsten Ryan, Admin, Laura Ritchie, Michelle Walsh, Tony Lowe, Kim Jackson, WikiSysop, Evan Thomas, Oyemi Sillo and Nicole Hills
Objective[edit | edit source]
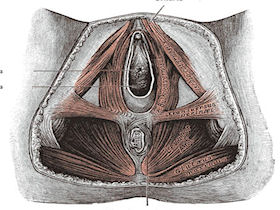
The Pelvic Floor Distress Inventory Questionnaire-20 (PFDI-20) is the short-form version of the Pelvic Floor Distress Inventory (PFDI).[1] Similar to the PFIQ-7, it is a health-related quality of life questionnaire for women with pelvic floor conditions to fill out.[1] The PFDI-20 is comprised of 3 scales, which include the Urinary Distress Inventory-6 (UDI-6), Pelvic Organ Prolapse Distress Inventory-6 (POPDI-6), and the Colorectal-Anal Distress Inventory-8 (CRADI-8).[1]
Intended Population[edit | edit source]
Women over the age of 18 with disorders of the pelvic floor including urinary incontinence, pelvic organ prolapse, and fecal incontinence.[1]
Method of Use[edit | edit source]
Since it is comprised of the UDI-6, POPDI-6, and the CRADI-8, the PFDI-20 includes 20 questions.[1] Each question begins with a "yes" or "no" response. If "yes," the patient must indicate how much bowl, bladder, or pelvic symptoms have been bothering them in the past 3 months on a 4-point scale that ranges from "not at all" (0) to "quite a bit" (4).[1] The scale scores are found individually by calculating the mean value of their corresponding questions and then multiplying by 25 to obtain a value that ranges from 0 to 100.[1] The sum of the 3 scales are added together to get the PFDI-20 summary score, which ranges from 0 to 300.[1]
Evidence[edit | edit source]
Correlation[edit | edit source]
Correlation, represented by r, ranges from -1.0 to +1.0. If the r value is 0 that means there is no correlation. If the r value is close to -1.0 that means that both values will decrease linearly. If the r value is close to +1.0 that means that both values will increase linearly.
Correlation of the short-form versions with the long-form versions:[1]
Reliability[edit | edit source]
The test-retest reliability, represented by intraclass correlation coefficients (ICC):[1]
Validity[edit | edit source]
The PFDI-20 demonstrates construct validity as it demonstrates a significant association with appropriate measures of symptom severity and pelvic floor diagnoses.[1]
Responsiveness[edit | edit source]
Each of the 3 scales of the PFDI-20 demonstrated moderate to excellent responsiveness with effect size and standardized response mean values ranging from 0.70 to 1.28.[1] The sensitivity of the PFDI-20 as a whole was excellent with an effect size of 1.48 P < .0001 and standardized response mean of 1.09 P < .0001.[1] The ability of the PFDI-20 to discriminate between subjects who indicated that they were "worse" after surgery from those who indicated they were "better" was excellent with c-statistic of .95.[1]
Clinically Meaningful Change[edit | edit source]
At the time of creation, the clinically meaningful change in quality of life (MCID)[2] needed to be studied in larger populations.[1] Studies have found minimal importance changes (MIC) ranging from 23 to 45.[1][3][4] For example, in their small sample size, Barber and colleagues (2004)[1] found a change in the summary score of 45 points or more to be meaningful after surgery.[1] However, it is important to consider that patients undergoing surgery also generally have higher scores at baseline.[5]
More recently, Wiegersma and colleagues (2017)[5] aimed to determine the MIC in women undergoing conservative pelvic organ prolapse treatments for mild symptoms.[5] They found that an improvement of 13.5 points to be helpful when evaluating the effects of conservative treatment strategies.[5]
Miscellaneous[edit | edit source]
The strength of the PFDI-20 is that it is a short form that gives a comprehensive assessment of the effect of pelvic floor disorders on the quality of life of women, rather than assessing just one aspect of pelvic floor function such as urinary incontinence. A more generic quality-of-life form as the SF-36 has demonstrated poor responsiveness in patients undergoing treatment for urinary incontinence. In these patient populations, it may be important to use both a generic quality-of-life instrument and a condition-specific instrument that has demonstrated responsiveness. The PFDI-20 is easy to use in both clinical and research settings.[1]
Links[edit | edit source]
- Overview of PFDI-20 on the Rehabilitation Measures Database.
- Paper by Barber et al 2005 describing the development of the PFIQ-7
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 adn PFIQ-7). Am J Obstet Gynecol 2005;193:103-113.
- ↑ Crosby RD, Kolotkin RL, Williams GR. Defining clinically meaningful change in health-related quality of life. Journal of clinical epidemiology. 2003 May 1;56(5):395-407.
- ↑ Gelhorn HL, Coyne KS, Sikirica V, Gauld J, Murphy M. Psychometric evaluation of health-related quality-of-life measures after pelvic organ prolapse surgery. Female pelvic medicine & reconstructive surgery. 2012 Jul 1;18(4):221-6.
- ↑ Utomo E, Blok BF, Steensma AB, Korfage IJ. Validation of the pelvic floor distress inventory (PFDI-20) and pelvic floor impact questionnaire (PFIQ-7) in a Dutch population. International urogynecology journal. 2014 Apr 1;25(4):531-44.
- ↑ 5.0 5.1 5.2 5.3 Wiegersma M, Panman CM, Berger MY, De Vet HC, Kollen BJ, Dekker JH. Minimal important change in the pelvic floor distress inventory-20 among women opting for conservative prolapse treatment. American journal of obstetrics and gynecology. 2017 Apr 1;216(4):397-e1.