Coccygodynia (Coccydynia, Coccalgia, Tailbone Pain): Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) (Expanded Differential Diagnosis) |
||
| Line 6: | Line 6: | ||
== Definition / Description == | == Definition / Description == | ||
Coccygodynia is considered a symptom not a diagnosis and is described as a disabling pain in and around the coccyx<ref name="Wray">Wray CC, Easom S, Hoskinson J. Coccydynia: aetiology and treatment. J Bone Joint Surg 1991;73(B):335-8.</ref><ref name="Kerr" />. The pain typically is triggered in a seat position and may intensify when the patient rises to a standing position.<ref name="Wray" /><ref name="Kerr" /> Coccygodynia may also be referred to as coccydynia or coccygeal neuralgia<ref name="Kerr">Kerr EE, Benson D, Schrot RJ. Coccygectomy for chronic refractory coccygodynia: clinical case series and literature review. J Neurosurg Spine 2011;14:654-663.</ref>. The pain caused by coccygodynia may have a significant impact on the patient's quality of life<ref name="Kerr" />. A patient may describe the pain as a pulling or lancinating sensation that may radiate to the sacrum, lumbar spine, buttocks, and occasionally into the thighs<ref name="Kerr" />. | Coccygodynia is considered a symptom not a diagnosis and is described as a disabling pain in and around the coccyx<ref name="Wray">Wray CC, Easom S, Hoskinson J. Coccydynia: aetiology and treatment. J Bone Joint Surg 1991;73(B):335-8.</ref><ref name="Kerr" />. The pain typically is triggered in a seat position and may intensify when the patient rises to a standing position.<ref name="Wray" /><ref name="Kerr" /> Coccygodynia may also be referred to as coccydynia or coccygeal neuralgia<ref name="Kerr">Kerr EE, Benson D, Schrot RJ. Coccygectomy for chronic refractory coccygodynia: clinical case series and literature review. J Neurosurg Spine 2011;14:654-663.</ref>. The pain caused by coccygodynia may have a significant impact on the patient's quality of life<ref name="Kerr" />. A patient may describe the pain as a pulling or lancinating sensation that may radiate to the sacrum, lumbar spine, buttocks, and occasionally into the thighs<ref name="Kerr" />. | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
| Line 24: | Line 24: | ||
== Epidemiology / Etiology == | == Epidemiology / Etiology == | ||
The prevalence for coccygodynia is five times greater in women than in men<ref name="Patel" />. This may be related to increased pressure during pregnancy or delivery (post-partum coccygodynia)<ref name="Ombregt">Ombregt L, Bisschop P, ter Veer JH. A System of Orthopaedic Medicine. Elsevier Science Limited, 2003, p.968-969.</ref>. | The prevalence for coccygodynia is five times greater in women than in men<ref name="Patel" />. This may be related to increased pressure during pregnancy or delivery (post-partum coccygodynia)<ref name="Ombregt">Ombregt L, Bisschop P, ter Veer JH. A System of Orthopaedic Medicine. Elsevier Science Limited, 2003, p.968-969.</ref>. The pain in the coccyx can be caused by radiation from a lumbosacral segment, a direct trauma or an overcharge<ref name="Gregory">Gregory P. Grieve, De wervelkolom, veel voorkomende aandoeningen (The spine), 1984, p. 320-321.</ref>. Congenital deviations can also cause complaints during long sitting<ref name="Gregory" />. <br><br>Coccygodynia may be classified as posttraumatic or idiopathic. Posttraumatic coccygodynia may be due to a fall onto the buttocks, or due to difficult childbirth<ref name="Kerr" />. Some studies question the possibility that coccygodynia could be caused by direct trauma, because of protection by the ischiadic bones. <br><br>Often, a positional change of the coccyx is caused by overtension of the anal levator muscle<ref name="Maigne">Maigne R. Douleurs d’origine vertébrale et traitements par manipulations, medicine orthopédique des derangements intervertébraux mineurs, 2e editie, p. 473-476.</ref>. In more than one-third of cases, coccygodynia has an idiopathic cause<ref name="Kerr" />.<br> | ||
== Characteristics / Clinical Presentation == | == Characteristics / Clinical Presentation == | ||
| Line 34: | Line 34: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
* Coccyx fracture | |||
* | * Rectal tumour | ||
* | * Perianal abscess | ||
* Lumbar spondylosis/disk herniation | |||
* [[Chronic proctalgia|Chronic proctalgia]] | |||
* [[Chronic Pelvic Pain|Chronic pelvic pain]] and pudendal neuralgia | |||
* [[Piriformis Syndrome|Piriformis syndrome]] | |||
[[Chronic proctalgia|Chronic proctalgia]] | |||
[[Chronic Pelvic Pain|Chronic pelvic pain]] and pudendal neuralgia | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 49: | Line 46: | ||
Local coccygodynia presents as pain felt in the coccyx during sitting, and does not spread in any direction. The pain can be relieved by sitting on a hard surface or with the buttocks over the border of the chair. Only pressure point pain is present. Depending on the exact location of the pain, walking, stair walking or getting up from sitting can be painful. | Local coccygodynia presents as pain felt in the coccyx during sitting, and does not spread in any direction. The pain can be relieved by sitting on a hard surface or with the buttocks over the border of the chair. Only pressure point pain is present. Depending on the exact location of the pain, walking, stair walking or getting up from sitting can be painful. | ||
Other movements are painless and examination of the lumbar spine and sacroiliac joints and hips are normal. Trauma or overtension of the levator ani muscle can shift the coccyx into an abnormal position. These contributing factors can be distinguished based on the affected tissues<ref name="Ombregt" /><ref name="Gregory" />.<br><br>Psychogenic coccydynia features a less specific pain location and usually a vague and radiating pain in various directions. Lumbar and hip movements are painful<ref name="Ombregt" />. | Other movements are painless and examination of the lumbar spine and sacroiliac joints and hips are normal. Trauma or overtension of the levator ani muscle can shift the coccyx into an abnormal position. These contributing factors can be distinguished based on the affected tissues<ref name="Ombregt" /><ref name="Gregory" />.<br><br>Psychogenic coccydynia features a less specific pain location and usually a vague and radiating pain in various directions. Lumbar and hip movements are painful<ref name="Ombregt" />. | ||
== Outcome Measures == | == Outcome Measures == | ||
=== Pain Measures === | |||
*[[4-Item Pain Intensity Measure (P4)]] | *[[4-Item Pain Intensity Measure (P4)]] | ||
*[[Brief Pain Inventory - Short Form]] | *[[Brief Pain Inventory - Short Form]] | ||
| Line 60: | Line 57: | ||
*[[Visual Analogue Scale]] | *[[Visual Analogue Scale]] | ||
=== Level of Function in Activities of Daily Living === | |||
* [[Oswestry Disability Index]] | * [[Oswestry Disability Index]] | ||
=== Condition Specific === | |||
*[[Pelvic Floor Distress Inventory (PFDI - 20)]] | *[[Pelvic Floor Distress Inventory (PFDI - 20)]] | ||
*[[Pelvic Girdle Questionnaire (PGQ)]] | *[[Pelvic Girdle Questionnaire (PGQ)]] | ||
== Examination == | == Examination == | ||
| Line 78: | Line 75: | ||
=== Mobilizations === | === Mobilizations === | ||
Mobilizations can be used to help realign the position of the coccyx. The first choice for mobilization is postero-anterior central vertebral pressure (first gently oscillating). Given that there is tenderness to palpation, it might be best to start with rotation mobilization. It is advised to begin mobilizing only one side at one treatment<ref name="Maitland">Maitland GD, Brewerton DA. Vertebral manipulation. Butterworths, 1973, p.236-239.</ref>.<br><br>Another option for manual therapy is to apply '''[[Deep friction massage|Deep transverse frictions]] (DTF)''' to the affected ligaments. The patient lies in a prone position with a pillow under the pelvis and the legs in slight abduction and internal rotation. The therapist places his thumb on the affected spot, and, depending on the location of the lesion (direction DTF), the DTF is administered. | Mobilizations can be used to help realign the position of the coccyx. The first choice for mobilization is postero-anterior central vertebral pressure (first gently oscillating). Given that there is tenderness to palpation, it might be best to start with rotation mobilization. It is advised to begin mobilizing only one side at one treatment<ref name="Maitland">Maitland GD, Brewerton DA. Vertebral manipulation. Butterworths, 1973, p.236-239.</ref>.<br><br>Another option for manual therapy is to apply '''[[Deep friction massage|Deep transverse frictions]] (DTF)''' to the affected ligaments. The patient lies in a prone position with a pillow under the pelvis and the legs in slight abduction and internal rotation. The therapist places his thumb on the affected spot, and, depending on the location of the lesion (direction DTF), the DTF is administered. | ||
=== Manipulation === | === Manipulation === | ||
Manipulation of the coccyx can be performed intrarectal with the patient in lateral position. With the index finger, the coccyx is repeatedly flexed and extended. This is performed for only one minute, to avoid damage or irritations of the rectal mucosa<ref name="Wray" />. | Manipulation of the coccyx can be performed intrarectal with the patient in lateral position. With the index finger, the coccyx is repeatedly flexed and extended. This is performed for only one minute, to avoid damage or irritations of the rectal mucosa<ref name="Wray" />. | ||
=== Massage === | === Massage === | ||
Massage of the levator ani muscle and coccygeus muscles has also been found to relieve pain<ref name="Thiele">Thiele GH. Coccygodynia: cause and treatment. Diseases of the Colon and Rectum, 1963, p.422-436.</ref><ref name="Wu">Wu C, et al. The application of infrared thermography in the assessment of patients with coccygodynia before and after manual therapy combined with diathermy. J Manipulative Physiol Ther 2009:287-293.</ref>. To exclude the possibility of muscles pulling on the os coccyx, relaxation of the pelvic floor muscles can be integrated by using '''biofeedback'''<ref name="Physiotherapist">Physiotherapist UZ Brussels, internal physiotherapy and gynaecology.</ref>. | Massage of the levator ani muscle and coccygeus muscles has also been found to relieve pain<ref name="Thiele">Thiele GH. Coccygodynia: cause and treatment. Diseases of the Colon and Rectum, 1963, p.422-436.</ref><ref name="Wu">Wu C, et al. The application of infrared thermography in the assessment of patients with coccygodynia before and after manual therapy combined with diathermy. J Manipulative Physiol Ther 2009:287-293.</ref>. To exclude the possibility of muscles pulling on the os coccyx, relaxation of the pelvic floor muscles can be integrated by using '''biofeedback'''<ref name="Physiotherapist">Physiotherapist UZ Brussels, internal physiotherapy and gynaecology.</ref>. | ||
== Evidence of Physical Therapy Treatments == | |||
* Stretching of piriformis and iliopsoas muscles and Maitland's rhythmic oscillatory thoracic mobilization for 3 weeks, 5 sessions per week showed significant improvement in pain pressure threshold.<ref>Mohanty PP, Pattnaik M. Effect of stretching of piriformis and iliopsoas in coccydynia. Journal of bodywork and movement therapies. 2017 Jul 1;21(3):743-6.</ref> | * Stretching of piriformis and iliopsoas muscles and Maitland's rhythmic oscillatory thoracic mobilization for 3 weeks, 5 sessions per week showed significant improvement in pain pressure threshold.<ref>Mohanty PP, Pattnaik M. Effect of stretching of piriformis and iliopsoas in coccydynia. Journal of bodywork and movement therapies. 2017 Jul 1;21(3):743-6.</ref> | ||
* Extracorporeal shortwave therapy was more effective and satisfactory in reducing discomfort and disability caused by coccydynia than the use of physical modalities. Thus, it was recommended as an alternative treatment option for patients with coccydynia.<ref>Lin SF, Chen YJ, Tu HP, Lee CL, Hsieh CL, Wu WL, Chen CH. The effects of extracorporeal shock wave therapy in patients with coccydynia: a randomized controlled trial. PloS one. 2015 Nov 10;10(11):e0142475.</ref> | * Extracorporeal shortwave therapy was more effective and satisfactory in reducing discomfort and disability caused by coccydynia than the use of physical modalities. Thus, it was recommended as an alternative treatment option for patients with coccydynia.<ref>Lin SF, Chen YJ, Tu HP, Lee CL, Hsieh CL, Wu WL, Chen CH. The effects of extracorporeal shock wave therapy in patients with coccydynia: a randomized controlled trial. PloS one. 2015 Nov 10;10(11):e0142475.</ref> | ||
* Combined manipulation and corticosteroid injection were more effective in the treatment of Coccydynia as compared to manipulation or corticosteroid injection alone. Patients following the treatment were completely pain free at the end of the year.<ref>Chakraborty S. Nonoperative Management of Coccydynia: A Comparative Study Comparing Three Methods. The Spine Journal. 2012 Sep 1;12(9):S69-70.</ref> | * Combined manipulation and corticosteroid injection were more effective in the treatment of Coccydynia as compared to manipulation or corticosteroid injection alone. Patients following the treatment were completely pain free at the end of the year.<ref>Chakraborty S. Nonoperative Management of Coccydynia: A Comparative Study Comparing Three Methods. The Spine Journal. 2012 Sep 1;12(9):S69-70.</ref> | ||
* In 16% of the patients (Wray et al) daily '''ultrasound''' followed by two weeks of short-wave diathermy (no settings were given) was found beneficial.<ref name="Wray" /><ref name="Wu" /> | * In 16% of the patients (Wray et al) daily '''ultrasound''' followed by two weeks of short-wave diathermy (no settings were given) was found beneficial.<ref name="Wray" /><ref name="Wu" /> | ||
== References == | == References == | ||
Revision as of 02:20, 16 June 2019
Original Editor - Maxime Tuerlinckx as part of the Vrije Universiteit Brussel's Evidence-based Practice project
Top Contributors - Victoria Geropoulos, Maxime Tuerlinckx, Nicole Hills, Evan Thomas, Kim Jackson, Vidya Acharya, Redisha Jakibanjar, Admin, Daphne Jackson, Laura Ritchie, WikiSysop, Aminat Abolade, Rosie Swift and Pacifique Dusabeyezu
Definition / Description[edit | edit source]
Coccygodynia is considered a symptom not a diagnosis and is described as a disabling pain in and around the coccyx[1][2]. The pain typically is triggered in a seat position and may intensify when the patient rises to a standing position.[1][2] Coccygodynia may also be referred to as coccydynia or coccygeal neuralgia[2]. The pain caused by coccygodynia may have a significant impact on the patient's quality of life[2]. A patient may describe the pain as a pulling or lancinating sensation that may radiate to the sacrum, lumbar spine, buttocks, and occasionally into the thighs[2].
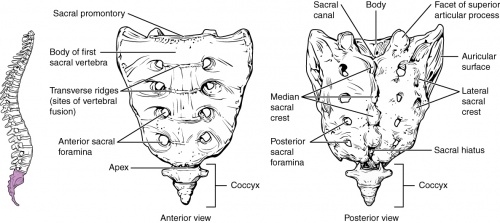
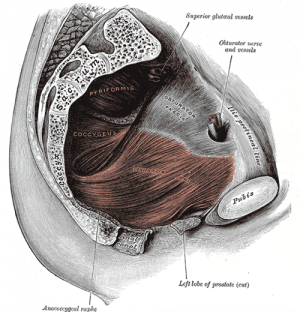
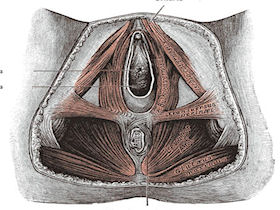
Clinically Relevant Anatomy[edit | edit source]
The coccyx is the most distal aspect of the vertebral column, and consists of three to five rudimentary vertebral units that are typically fused. The ventral part of the coccyx is concave, and the dorsal aspect is convex and features coccygeal articular processes[3]. The coccyx articulates with the sacral cornua of the inferior sacral apex at S5[3].
The anterior aspect of the coccyx serves as the attachment site of ligaments and muscles important for many functions of the pelvic floor. The levator ani muscle includes the coccygeus, pubococcygeus, and iliococcygeus. The coccyx supports the position of the anus. Attached to the posterior side of the coccyx is gluteus maximus. Muscle weakness disturbed tonus or damage to muscles or ligaments can cause abnormal positions of the coccyx[3].
Epidemiology / Etiology[edit | edit source]
The prevalence for coccygodynia is five times greater in women than in men[3]. This may be related to increased pressure during pregnancy or delivery (post-partum coccygodynia)[4]. The pain in the coccyx can be caused by radiation from a lumbosacral segment, a direct trauma or an overcharge[5]. Congenital deviations can also cause complaints during long sitting[5].
Coccygodynia may be classified as posttraumatic or idiopathic. Posttraumatic coccygodynia may be due to a fall onto the buttocks, or due to difficult childbirth[2]. Some studies question the possibility that coccygodynia could be caused by direct trauma, because of protection by the ischiadic bones.
Often, a positional change of the coccyx is caused by overtension of the anal levator muscle[6]. In more than one-third of cases, coccygodynia has an idiopathic cause[2].
Characteristics / Clinical Presentation[edit | edit source]
The patient may complain of pain in the coccyx region during, going into, or coming out of a seated position - this is first indication of coccygodynia. Tenderness over the coccyx is likely present, and the location of tenderness may help to discern between different forms of coccygodynia[4][5]:
- Referred or radiating pain is caused by a lumbar disc lesion, irritation of lower pelvic structures or deviations of the lower lumbar and/or sacroiliac joints[4][5].
- Local pain or coccygodynia is usually caused by direct trauma to the coccyx bone, or may be idiopathic in nature: Factors contributing to idiopathic coccygodynia include anatomical variations of the coccyx or pregnancy/delivery.[4][5].
Differential Diagnosis[edit | edit source]
- Coccyx fracture
- Rectal tumour
- Perianal abscess
- Lumbar spondylosis/disk herniation
- Chronic proctalgia
- Chronic pelvic pain and pudendal neuralgia
- Piriformis syndrome
Diagnostic Procedures[edit | edit source]
Local coccygodynia presents as pain felt in the coccyx during sitting, and does not spread in any direction. The pain can be relieved by sitting on a hard surface or with the buttocks over the border of the chair. Only pressure point pain is present. Depending on the exact location of the pain, walking, stair walking or getting up from sitting can be painful.
Other movements are painless and examination of the lumbar spine and sacroiliac joints and hips are normal. Trauma or overtension of the levator ani muscle can shift the coccyx into an abnormal position. These contributing factors can be distinguished based on the affected tissues[4][5].
Psychogenic coccydynia features a less specific pain location and usually a vague and radiating pain in various directions. Lumbar and hip movements are painful[4].
Outcome Measures[edit | edit source]
Pain Measures[edit | edit source]
- 4-Item Pain Intensity Measure (P4)
- Brief Pain Inventory - Short Form
- Numeric Pain Rating Scale
- Short-form McGill Pain Questionnaire
- Visual Analogue Scale
Level of Function in Activities of Daily Living[edit | edit source]
Condition Specific[edit | edit source]
Examination[edit | edit source]
Coccygodynia can be diagnosed during a physical examination. Patients may take a guarding seated position, in which one buttock is elevated to shift weight from the coccyx and to prevent and/or minimize discomfort and pain. With referred or radiated pain, the pain will also arise during lumbar movements. Coughing is painful. Physical examination will show increased pain during a straight leg raise test. There may be radiating pain around the buttocks and going to the back of the thighs. Women may have pain during menstruation[4][5]. Palpation at the sacrococcygeal junction will elicit a tender point and will be painful[2].
Physical Therapy Management[edit | edit source]
Patients with coccygodynia are initially advised to avoid provocative factors. Initial treatment includes ergonomic adjustments such as using a donut-shaped pillow or gel cushion when sitting for a long period of time. This reduces local pressure and improves the patient's posture. There is however no significant evidence that these minor changes reduce the patient's complaints[8].
Mobilizations[edit | edit source]
Mobilizations can be used to help realign the position of the coccyx. The first choice for mobilization is postero-anterior central vertebral pressure (first gently oscillating). Given that there is tenderness to palpation, it might be best to start with rotation mobilization. It is advised to begin mobilizing only one side at one treatment[9].
Another option for manual therapy is to apply Deep transverse frictions (DTF) to the affected ligaments. The patient lies in a prone position with a pillow under the pelvis and the legs in slight abduction and internal rotation. The therapist places his thumb on the affected spot, and, depending on the location of the lesion (direction DTF), the DTF is administered.
Manipulation[edit | edit source]
Manipulation of the coccyx can be performed intrarectal with the patient in lateral position. With the index finger, the coccyx is repeatedly flexed and extended. This is performed for only one minute, to avoid damage or irritations of the rectal mucosa[1].
Massage[edit | edit source]
Massage of the levator ani muscle and coccygeus muscles has also been found to relieve pain[10][11]. To exclude the possibility of muscles pulling on the os coccyx, relaxation of the pelvic floor muscles can be integrated by using biofeedback[12].
Evidence of Physical Therapy Treatments[edit | edit source]
- Stretching of piriformis and iliopsoas muscles and Maitland's rhythmic oscillatory thoracic mobilization for 3 weeks, 5 sessions per week showed significant improvement in pain pressure threshold.[13]
- Extracorporeal shortwave therapy was more effective and satisfactory in reducing discomfort and disability caused by coccydynia than the use of physical modalities. Thus, it was recommended as an alternative treatment option for patients with coccydynia.[14]
- Combined manipulation and corticosteroid injection were more effective in the treatment of Coccydynia as compared to manipulation or corticosteroid injection alone. Patients following the treatment were completely pain free at the end of the year.[15]
- In 16% of the patients (Wray et al) daily ultrasound followed by two weeks of short-wave diathermy (no settings were given) was found beneficial.[1][11]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Wray CC, Easom S, Hoskinson J. Coccydynia: aetiology and treatment. J Bone Joint Surg 1991;73(B):335-8.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Kerr EE, Benson D, Schrot RJ. Coccygectomy for chronic refractory coccygodynia: clinical case series and literature review. J Neurosurg Spine 2011;14:654-663.
- ↑ 3.0 3.1 3.2 3.3 Patel R, Appanagari A, Whang PG. Coccydynia. Curr Rev Musculoskelet Med 2008;1:223-226.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Ombregt L, Bisschop P, ter Veer JH. A System of Orthopaedic Medicine. Elsevier Science Limited, 2003, p.968-969.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Gregory P. Grieve, De wervelkolom, veel voorkomende aandoeningen (The spine), 1984, p. 320-321.
- ↑ Maigne R. Douleurs d’origine vertébrale et traitements par manipulations, medicine orthopédique des derangements intervertébraux mineurs, 2e editie, p. 473-476.
- ↑ CRTechnologies Straight Leg Raise Test (CR) Available from https://www.youtube.com/watch?time_continue=2&v=KziCDXXfC-4 accessed on 13/6/19
- ↑ Chiarioni G, et al. Chronic proctalgia and chronic pelvic pain syndromes: New etiologic insights and treatment options. World J Gastroenterol 2011;17(40):4451-4455.
- ↑ Maitland GD, Brewerton DA. Vertebral manipulation. Butterworths, 1973, p.236-239.
- ↑ Thiele GH. Coccygodynia: cause and treatment. Diseases of the Colon and Rectum, 1963, p.422-436.
- ↑ 11.0 11.1 Wu C, et al. The application of infrared thermography in the assessment of patients with coccygodynia before and after manual therapy combined with diathermy. J Manipulative Physiol Ther 2009:287-293.
- ↑ Physiotherapist UZ Brussels, internal physiotherapy and gynaecology.
- ↑ Mohanty PP, Pattnaik M. Effect of stretching of piriformis and iliopsoas in coccydynia. Journal of bodywork and movement therapies. 2017 Jul 1;21(3):743-6.
- ↑ Lin SF, Chen YJ, Tu HP, Lee CL, Hsieh CL, Wu WL, Chen CH. The effects of extracorporeal shock wave therapy in patients with coccydynia: a randomized controlled trial. PloS one. 2015 Nov 10;10(11):e0142475.
- ↑ Chakraborty S. Nonoperative Management of Coccydynia: A Comparative Study Comparing Three Methods. The Spine Journal. 2012 Sep 1;12(9):S69-70.