Brain Tumors: Difference between revisions
No edit summary |
Aya Alhindi (talk | contribs) (general review and added associated spinal cord involvement, Choroid plexus papilloma ,Germ cell tumors and corrected the references ,added references to YT videos) |
||
| Line 4: | Line 4: | ||
[[Brain Anatomy|Brain]] tumours refers to a diverse group of neoplasms originating from intracranial tissues and the [[meninges]] with malignancy levels ranging from benign to aggressive. | [[Brain Anatomy|Brain]] tumours refers to a diverse group of neoplasms originating from intracranial tissues and the [[meninges]] with malignancy levels ranging from benign to aggressive. | ||
Each tumour type has its own biology, treatment, and prognosis and risk factors.<ref name=":2">McKinney PA. [https://jnnp.bmj.com/content/75/suppl_2/ii12 Brain tumours: incidence, survival, and aetiology.] Journal of Neurology, Neurosurgery & Psychiatry. 2004 Jun 1;75(suppl 2):ii12-7. | Each tumour type has its own biology, treatment, and prognosis and risk factors.<ref name=":2">McKinney PA. [https://jnnp.bmj.com/content/75/suppl_2/ii12 Brain tumours: incidence, survival, and aetiology.] Journal of Neurology, Neurosurgery & Psychiatry. 2004 Jun 1;75(suppl 2):ii12-7. </ref> | ||
More than 50 per cent are malignant with poor prognosis despite [[Surgery and General Anaesthetic|surgery]], [[Radiation Side Effects and Syndromes|radiotherapy]], and [[Chemotherapy Side Effects and Syndromes|chemotherapy]] <ref name=":0">de Robles P, Fiest KM, Frolkis AD, Pringsheim T, Atta C, St. Germaine-Smith C, Day L, Lam D, Jette N. The worldwide incidence and prevalence of primary brain tumors: a systematic review and meta-analysis. Neuro-oncology. 2015 Jun 1;17(6):776-83.</ref>. Even benign or low -grade brain tumors can cause significant | More than 50 per cent are malignant with poor prognosis despite [[Surgery and General Anaesthetic|surgery]], [[Radiation Side Effects and Syndromes|radiotherapy]], and [[Chemotherapy Side Effects and Syndromes|chemotherapy]] <ref name=":0">de Robles P, Fiest KM, Frolkis AD, Pringsheim T, Atta C, St. Germaine-Smith C, Day L, Lam D, Jette N. The worldwide incidence and prevalence of primary brain tumors: a systematic review and meta-analysis. Neuro-oncology. 2015 Jun 1;17(6):776-83.</ref>. Even benign or low -grade brain tumors can cause significant disability<ref name=":1">Vargo M. Brain tumor rehabilitation. American journal of physical medicine & rehabilitation. 2011 May 1;90(5):S50-62.</ref>. | ||
== Epidemiology == | == Epidemiology == | ||
[[File:Ependymoma4.jpg|right|frameless]] | [[File:Ependymoma4.jpg|right|frameless]] | ||
| Line 14: | Line 14: | ||
* Gliomas are more frequent in men | * Gliomas are more frequent in men | ||
* Meningiomas are more frequent in women.<ref name=":3">Radiopedia [https://radiopaedia.org/articles/brain-tumours Brain Tumours] | * Meningiomas are more frequent in women.<ref name=":3">Radiopedia [https://radiopaedia.org/articles/brain-tumours Brain Tumours] </ref> | ||
Apart from [[Genetics and Health|genetic]] tendency, the largest environmental risk factor for brain tumours is exposure to high doses of ionising radiation.<ref name=":2" /> | Apart from [[Genetics and Health|genetic]] tendency, the largest environmental risk factor for brain tumours is exposure to high doses of ionising radiation.<ref name=":2" /> | ||
== Classification == | == Classification == | ||
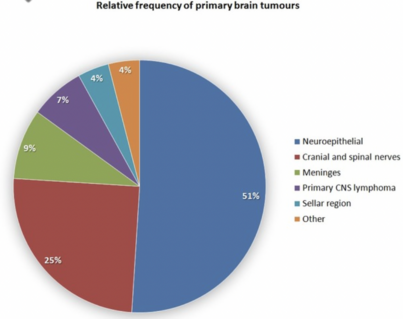
Brain tumour is an umbrella term for numerous individual tumours. Note figures shown vary significantly | Brain tumour is an umbrella term for numerous individual tumours. Note figures shown vary significantly dependent on study. They are mainly classified into the below divisions.<ref name=":3" /> | ||
== Glioma == | == Glioma == | ||
[[File:Glioma.gif|thumb|502x502px|Glioma of the left [[Parietal Lobe|parietal lobe]]]] | [[File:Glioma.gif|thumb|502x502px|Glioma of the left [[Parietal Lobe|parietal lobe]]]] | ||
'''Gliomas''' '''tumours:''' start in the glial (neuroglia) cells of the brain, also known as | '''Gliomas''' '''tumours:''' start in the glial (neuroglia) cells of the brain, also known as neuro-epithelial, most common (50%). They include: astrocytoma, most common tumours arising from [[Glial Cells|glial cells]] (44%); [[ependymoma]] (3%); medulloblastoma (3%); oligodendroglioma (2%). | ||
There are three common types of gliomas, based on the glial cell type: | There are three common types of gliomas, based on the glial cell type: | ||
# Astrocytomas: Originated from astrocytes and can be encapsulated. Low grades are common in children while high grades are common in young adults and older patients. Glioblastomas, a type of high-grade astrocytoma, make up > 50% of all gliomas, common in both adults and children. | # '''Astrocytomas:''' Originated from astrocytes and can be encapsulated. Low grades are common in children while high grades are common in young adults and older patients. Glioblastomas, a type of high-grade astrocytoma, make up > 50% of all gliomas, common in both adults and children. | ||
# Oligodendrogliomas: Originated from oligodendrocyte cells. Less infiltrating than astrocytomas, common in adults. | # '''Oligodendrogliomas:''' Originated from oligodendrocyte cells. Less infiltrating than astrocytomas, common in adults. | ||
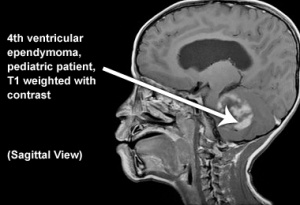
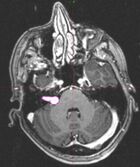
# Ependymomas: Originated from ependymal cells (cells lining the ventricular cavities and the central canal of the spinal cord). Common in the pediatric patient population. | # '''Ependymomas:''' Originated from ependymal cells (cells lining the ventricular cavities and the central canal of the spinal cord). Common in the pediatric patient population. | ||
[[Headache|Headaches]] are the most common first symptom of patients with glioma, thought to be a result of tumour growth that causing a mass effect on surrounding tissue. Gliomas generally, notably glioblastomas, are hard difficult to treat. Despite progress in understanding the | [[Headache|Headaches]] are the most common first symptom of patients with glioma, thought to be a result of tumour growth that causing a mass effect on surrounding tissue. Gliomas generally, notably glioblastomas, are hard difficult to treat. Despite progress in understanding the pathophysiology of gliomas, no significant impact has been made toward preventing the lethality of high-grade gliomas.<ref>Mesfin FB, Al-Dhahir MA. [https://www.ncbi.nlm.nih.gov/books/NBK441874/ Gliomas] in StatPearls.</ref> | ||
Gliomas can spread to the spinal axis via the cerebrospinal fluid (CSF).Spinal seeding is common in patients with glioblastoma (up to 20% of cases have positive CSF) or anaplastic astrocytoma, but it is uncommon in patients with oligodendroglioma, both low grade and anaplastic.<ref>Mariniello G, Peca C, Del Basso De Caro M, Carotenuto B, Formicola F, Elefante A, et al. [http://journals.sagepub.com/doi/10.1177/1971400915594534 Brain gliomas presenting with symptoms of spinal cord metastasis]. Neuroradiol J. 2015;28(5):478–82. </ref> | |||
== '''Non-Glioma Tumour''' == | == '''Non-Glioma Tumour''' == | ||
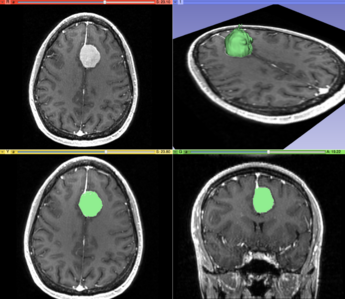
[[File:MeningiomaMRISegmentation.png|thumb|345x345px|Meningioma MRI Segmentation]] | [[File:MeningiomaMRISegmentation.png|thumb|345x345px|Meningioma MRI Segmentation]] | ||
Include: | Include: | ||
* Meningioma, most common tumour of the [[meninges]] | * Meningioma, most common tumour of the [[meninges]] (15%).Originate from the meningeal layer of either the brain or the spinal cord (non-glial neoplasm). Most meningiomas are benign (grade 1), roughly 1 to 3% of meningiomas can change into malignant tumours with a poor prognosis (5-year survival rate of 32 to 64%). Risk factors for recurrence include genetic disorders such as [[Neurofibromatosis Type II|neurofibromatosis type 2]], exposure to [[Radiation Side Effects and Syndromes|radiation]], hormonal therapy, and family history. Manifestation are dependent on size and location with wide differences in symptoms eg asymptomatic to severe experience neurological deficits.<ref>Alruwaili AA, De Jesus O. [https://www.ncbi.nlm.nih.gov/books/NBK560538/ Meningioma]. InStatPearls 2022 May 8. StatPearls Publishing. </ref> | ||
*[[Brain Metastasis|Metastases]] (15%) | *[[Brain Metastasis|Metastases]] (15%) | ||
*[[Pituitary Gland|Pituitary]] tumours (8%). Starts in the pituitary gland, usually benign<ref name=":4" /> | *[[Pituitary Gland|Pituitary]] tumours (8%). Starts in the pituitary gland, usually benign<ref name=":4" /> | ||
*Schwannoma (8%). Starts in Schwann cells which surround nerves in the brain, usually benign, includes [[Facial Schwannoma]] | *[[File:Tumor Acoustic Neuroma.JPG|thumb|Acoustic Neuroma (pink)|alt=|167x167px]]Schwannoma (8%). Starts in Schwann cells which surround nerves in the brain, usually benign, includes [[Facial Schwannoma]][[Acoustic Neuroma|,Acoustic Neurom]]<nowiki/>[[Acoustic Neuroma|a]].<ref name=":4" /> | ||
* Primary CNS [[lymphoma]] (2.5%) | * Primary CNS [[lymphoma]] (2.5%) | ||
* [[Pineal Gland|Pineal]] tumours: Starts in the pineal gland.<ref name=":3" /> | * [[Pineal Gland|Pineal]] tumours: Starts in the pineal gland.<ref name=":3" /> | ||
* Intracranial germ cell tumours 0.4% to 3.4% | * Intracranial germ cell tumours 0.4% to 3.4%. | ||
== Choroid plexus papilloma == | |||
This uncommon, usually benign childhood tumour grows slowly and can increase CSF production and block CSF flow, resulting in headaches and increased intracranial pressure. A less common cancerous form can spread through the cerebrospinal fluid.<ref name=":5">Brain and Spinal Cord Tumors [Internet]. [https://www.ninds.nih.gov/health-information/disorders/brain-and-spinal-cord-tumors National Institute of Neurological Disorders and Stroke.] </ref> | |||
== Germ cell tumors == | |||
These extremely rare childhood tumours may develop from cells that do not leave the CNS during development. Germ cell tumours typically develop in the centre of the brain and can spread to other parts of the brain and spinal cord. Tumours are named after the type of germ cell they contain. <ref name=":5" /> | |||
== Treatment == | == Treatment == | ||
Treatment aims vary, being to remove the tumour completely, slow its growth, or relieve symptoms by reducing the tumour size and decrease swelling. Treatment is personalised and is dependent on many factors including: | Treatment aims vary, being to remove the tumour completely, slow its growth, or relieve symptoms by reducing the tumour size and decrease swelling. | ||
Treatment is personalised and is dependent on many factors including: | |||
* Type, size, grade, location and genetic make-up of the tumour | * Type, size, grade, location and genetic make-up of the tumour | ||
| Line 52: | Line 62: | ||
A benign tumour may only need surgery to removed, but with a malignant brain treatment options include surgery, radiation therapy and chemotherapy (alone or together). Medicines aim to reduce symptoms or through a clinical trial new or modified treatments may. | A benign tumour may only need surgery to removed, but with a malignant brain treatment options include surgery, radiation therapy and chemotherapy (alone or together). Medicines aim to reduce symptoms or through a clinical trial new or modified treatments may. | ||
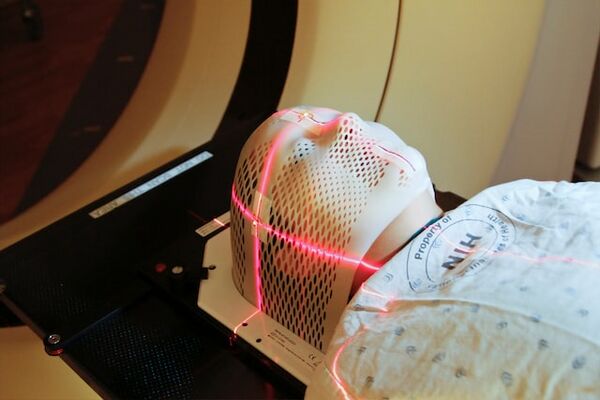
A multidisciplinary team will be involved which may include a medical oncologist, neuropathologist, rehabilitation specialist and Physiotherapist.<ref name=":4">Cancer council Victoria [https://www.cancervic.org.au/cancer-information/types-of-cancer/brain_tumour/brain-tumours-overview.html Brain Tumours] | A multidisciplinary team will be involved which may include a medical oncologist, neuropathologist, rehabilitation specialist and Physiotherapist.<ref name=":4">Cancer council Victoria [https://www.cancervic.org.au/cancer-information/types-of-cancer/brain_tumour/brain-tumours-overview.html Brain Tumours] </ref>[[File:National-cancer-institute-Jg89tuvB1iQ-unsplash.jpeg|thumb|Laser used to pinpoint tumour in a CT scanner to obtain images of tumour before radiation therapy|alt=|center|600x600px]] | ||
== See | == Also See == | ||
[[Oncology Medical Management]]; [[Oncology Physiotherapy Management]]; [[Physiotherapy Role in Geriatric Oncology]]; [[Physical Activity in Cancer]] | [[Oncology Medical Management]]; [[Oncology Physiotherapy Management]]; [[Physiotherapy Role in Geriatric Oncology]]; [[Physical Activity in Cancer]] | ||
== Viewing == | == Viewing == | ||
{{#ev:youtube|pBSncknENRc}} | {{#ev:youtube|pBSncknENRc}}<ref>Challenged N. 2-Minute Neuroscience: [https://www.youtube.com/watch?v=pBSncknENRc Brain tumors] [Internet]. Youtube; 2018 . </ref>{{#ev:youtube|od4h5bf_IUY}}<ref>LearnNeuroradiology. [https://www.youtube.com/watch?v=od4h5bf_IUY Imaging brain tumors - 1 -] Introduction and classification [Internet]. Youtube; 2018 </ref> | ||
{{#ev:youtube|od4h5bf_IUY}} | |||
== References == | == References == | ||
Revision as of 02:00, 1 December 2023
Introduction[edit | edit source]
Brain tumours refers to a diverse group of neoplasms originating from intracranial tissues and the meninges with malignancy levels ranging from benign to aggressive.
Each tumour type has its own biology, treatment, and prognosis and risk factors.[1]
More than 50 per cent are malignant with poor prognosis despite surgery, radiotherapy, and chemotherapy [2]. Even benign or low -grade brain tumors can cause significant disability[3].
Epidemiology[edit | edit source]
Brain tumours increase in frequency with age, with a few notable exceptions and some uncommon tumours found in infancy.
Sex differences:
- Gliomas are more frequent in men
- Meningiomas are more frequent in women.[4]
Apart from genetic tendency, the largest environmental risk factor for brain tumours is exposure to high doses of ionising radiation.[1]
Classification[edit | edit source]
Brain tumour is an umbrella term for numerous individual tumours. Note figures shown vary significantly dependent on study. They are mainly classified into the below divisions.[4]
Glioma[edit | edit source]
Gliomas tumours: start in the glial (neuroglia) cells of the brain, also known as neuro-epithelial, most common (50%). They include: astrocytoma, most common tumours arising from glial cells (44%); ependymoma (3%); medulloblastoma (3%); oligodendroglioma (2%).
There are three common types of gliomas, based on the glial cell type:
- Astrocytomas: Originated from astrocytes and can be encapsulated. Low grades are common in children while high grades are common in young adults and older patients. Glioblastomas, a type of high-grade astrocytoma, make up > 50% of all gliomas, common in both adults and children.
- Oligodendrogliomas: Originated from oligodendrocyte cells. Less infiltrating than astrocytomas, common in adults.
- Ependymomas: Originated from ependymal cells (cells lining the ventricular cavities and the central canal of the spinal cord). Common in the pediatric patient population.
Headaches are the most common first symptom of patients with glioma, thought to be a result of tumour growth that causing a mass effect on surrounding tissue. Gliomas generally, notably glioblastomas, are hard difficult to treat. Despite progress in understanding the pathophysiology of gliomas, no significant impact has been made toward preventing the lethality of high-grade gliomas.[5]
Gliomas can spread to the spinal axis via the cerebrospinal fluid (CSF).Spinal seeding is common in patients with glioblastoma (up to 20% of cases have positive CSF) or anaplastic astrocytoma, but it is uncommon in patients with oligodendroglioma, both low grade and anaplastic.[6]
Non-Glioma Tumour[edit | edit source]
Include:
- Meningioma, most common tumour of the meninges (15%).Originate from the meningeal layer of either the brain or the spinal cord (non-glial neoplasm). Most meningiomas are benign (grade 1), roughly 1 to 3% of meningiomas can change into malignant tumours with a poor prognosis (5-year survival rate of 32 to 64%). Risk factors for recurrence include genetic disorders such as neurofibromatosis type 2, exposure to radiation, hormonal therapy, and family history. Manifestation are dependent on size and location with wide differences in symptoms eg asymptomatic to severe experience neurological deficits.[7]
- Metastases (15%)
- Pituitary tumours (8%). Starts in the pituitary gland, usually benign[8]
- Schwannoma (8%). Starts in Schwann cells which surround nerves in the brain, usually benign, includes Facial Schwannoma,Acoustic Neuroma.[8]
- Primary CNS lymphoma (2.5%)
- Pineal tumours: Starts in the pineal gland.[4]
- Intracranial germ cell tumours 0.4% to 3.4%.
Choroid plexus papilloma[edit | edit source]
This uncommon, usually benign childhood tumour grows slowly and can increase CSF production and block CSF flow, resulting in headaches and increased intracranial pressure. A less common cancerous form can spread through the cerebrospinal fluid.[9]
Germ cell tumors[edit | edit source]
These extremely rare childhood tumours may develop from cells that do not leave the CNS during development. Germ cell tumours typically develop in the centre of the brain and can spread to other parts of the brain and spinal cord. Tumours are named after the type of germ cell they contain. [9]
Treatment[edit | edit source]
Treatment aims vary, being to remove the tumour completely, slow its growth, or relieve symptoms by reducing the tumour size and decrease swelling.
Treatment is personalised and is dependent on many factors including:
- Type, size, grade, location and genetic make-up of the tumour
- Clients age, medical history and health status
- Symptoms.
A benign tumour may only need surgery to removed, but with a malignant brain treatment options include surgery, radiation therapy and chemotherapy (alone or together). Medicines aim to reduce symptoms or through a clinical trial new or modified treatments may.
A multidisciplinary team will be involved which may include a medical oncologist, neuropathologist, rehabilitation specialist and Physiotherapist.[8]
Also See[edit | edit source]
Oncology Medical Management; Oncology Physiotherapy Management; Physiotherapy Role in Geriatric Oncology; Physical Activity in Cancer
Viewing[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 McKinney PA. Brain tumours: incidence, survival, and aetiology. Journal of Neurology, Neurosurgery & Psychiatry. 2004 Jun 1;75(suppl 2):ii12-7.
- ↑ de Robles P, Fiest KM, Frolkis AD, Pringsheim T, Atta C, St. Germaine-Smith C, Day L, Lam D, Jette N. The worldwide incidence and prevalence of primary brain tumors: a systematic review and meta-analysis. Neuro-oncology. 2015 Jun 1;17(6):776-83.
- ↑ Vargo M. Brain tumor rehabilitation. American journal of physical medicine & rehabilitation. 2011 May 1;90(5):S50-62.
- ↑ 4.0 4.1 4.2 Radiopedia Brain Tumours
- ↑ Mesfin FB, Al-Dhahir MA. Gliomas in StatPearls.
- ↑ Mariniello G, Peca C, Del Basso De Caro M, Carotenuto B, Formicola F, Elefante A, et al. Brain gliomas presenting with symptoms of spinal cord metastasis. Neuroradiol J. 2015;28(5):478–82.
- ↑ Alruwaili AA, De Jesus O. Meningioma. InStatPearls 2022 May 8. StatPearls Publishing.
- ↑ 8.0 8.1 8.2 Cancer council Victoria Brain Tumours
- ↑ 9.0 9.1 Brain and Spinal Cord Tumors [Internet]. National Institute of Neurological Disorders and Stroke.
- ↑ Challenged N. 2-Minute Neuroscience: Brain tumors [Internet]. Youtube; 2018 .
- ↑ LearnNeuroradiology. Imaging brain tumors - 1 - Introduction and classification [Internet]. Youtube; 2018