Clostridium Difficile Infection CDI: Difference between revisions
Reem Ramadan (talk | contribs) No edit summary |
Reem Ramadan (talk | contribs) No edit summary |
||
| Line 7: | Line 7: | ||
== Introduction == | == Introduction == | ||
[[File:Clostridium difficile CDC.jpeg|thumb|Clostridium difficile]] | [[File:Clostridium difficile CDC.jpeg|thumb|Clostridium difficile]] | ||
Clostridium difficile is | Clostridium Difficile Infections (CDI) are considered one of the most significant nosocomial infections which affect all hospitals worldwide. Clostridium difficile (C. Difficile) is an anaerobic, gram-positive, spore-forming bacillus [[Bacterial Infections|bacteria]] that can cause colitis, a serious [[Inflammation Acute and Chronic|inflammation]] of the colon. [[Infectious Disease|Infections]] from C. difficile often start after over-taking [[antibiotics]] and can sometimes be life-threatening<ref name=":0">Web md Clostridium difficile Available:https://www.webmd.com/digestive-disorders/clostridium-difficile-colitis (accessed 12.5.2022)</ref>. This rode shaped bacterium exists in vegetative or spore form and can survive harsh environments and common sterilization techniques. Clostridium difficile is resistant to ultra-violent light, high temperatures, and antibiotics.<ref name="p2">Cecil J. Clostridium difficile: Changing Epidemiology, Treatment and Infection Prevention Measures. Current Infectious Disease Reports [serial online]. December 2012;14(6):612-619. Available from: MEDLINE, Ipswich, MA. Accessed March 17, 2014</ref> | ||
== Epidemiology == | == Epidemiology == | ||
Clostridium difficile infection (CDI) has become a serious medical and epidemiological problem | Clostridium difficile infection (CDI) has become a serious medical and epidemiological problem with approximately 5% of adults and 15 to 70% of children being colonized by C. difficile and the colonization prevalence further increases with hospitalized patients and patients in nursing homes<ref>Leffler DA, Lamont JT. Clostridium difficile infection. New England Journal of Medicine. 2015 Apr 16;372(16):1539-48.</ref>. Also, patients above the age of 65 are more at risk at developing CDI than younger patients<ref>Czepiel J, Kędzierska J, Biesiada G, Birczyńska M, Perucki W, Nowak P, Garlicki A. Epidemiology of Clostridium difficile infection: results of a hospital-based study in Krakow, Poland. Epidemiology & Infection. 2015 Nov;143(15):3235-43.</ref>. The incidence of CDIs also depends on the length of the hospitalization period where during the first few days of hospitalization the risk is between 2.1 to 20% and longer periods of hospitalization increase the risk to up to 45.4% of getting CDI<ref>Hung YP, Lin HJ, Wu TC, Liu HC, Lee JC, Lee CI, Wu YH, Wan L, Tsai PJ, Ko WC. Risk factors of fecal toxigenic or non-toxigenic Clostridium difficile colonization: impact of Toll-like receptor polymorphisms and prior antibiotic exposure. PloS one. 2013 Jul 25;8(7):e69577.</ref>. In 2015, the Centers for Disease Control and Prevention (CDC) found that C. difficile caused half a million infections and resulted in 15,000 deaths in a single year<ref name=":2">Medical news today What to know about Clostridium difficile Available:https://www.medicalnewstoday.com/articles/172329#what-is-c-difficile (accessed 12.5.2022)</ref>. Prevention, proper diagnosis and effective treatment are necessary to reduce the risk for the patients, deplete the spreading of infection and diminish the probability of recurrent infection. | ||
In 2015, the Centers for Disease Control and Prevention (CDC) found that C. difficile caused half a million infections and resulted in 15,000 deaths in a single year<ref name=":2">Medical news today What to know about Clostridium difficile Available:https://www.medicalnewstoday.com/articles/172329#what-is-c-difficile (accessed 12.5.2022)</ref>. | |||
== Etiology == | == Etiology == | ||
[[File:Hand hygeine.jpg|thumb|Hand | [[File:Hand hygeine.jpg|thumb|Hand Hygiene]] | ||
C. diff exists all around us, being in the air, water, soil, and in the feces of humans and animals. C. diff bacteria that are outside the body turn into spores that can live on surfaces for weeks or months. These spores are dormant but they can become active after ingestion, getting into the intestines. C. difficile also naturally occurs in the gut. When the bacterium is present at normal levels, it is not considered to be an infection. | C. diff exists all around us, being in the air, water, soil, and in the feces of humans and animals. C. diff bacteria that are outside the body turn into spores that can live on surfaces for weeks or months. These spores are dormant but they can become active after ingestion, getting into the intestines. C. difficile also naturally occurs in the gut. When the bacterium is present at normal levels, it is not considered to be an infection. | ||
Revision as of 20:49, 24 February 2023
Original Editors - John Hardy from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - John Hardy, Lucinda hampton, Reem Ramadan, Elaine Lonnemann, WikiSysop, 127.0.0.1, Oyemi Sillo, Kim Jackson, Vidya Acharya and Nupur Smit Shah
Introduction[edit | edit source]
Clostridium Difficile Infections (CDI) are considered one of the most significant nosocomial infections which affect all hospitals worldwide. Clostridium difficile (C. Difficile) is an anaerobic, gram-positive, spore-forming bacillus bacteria that can cause colitis, a serious inflammation of the colon. Infections from C. difficile often start after over-taking antibiotics and can sometimes be life-threatening[1]. This rode shaped bacterium exists in vegetative or spore form and can survive harsh environments and common sterilization techniques. Clostridium difficile is resistant to ultra-violent light, high temperatures, and antibiotics.[2]
Epidemiology[edit | edit source]
Clostridium difficile infection (CDI) has become a serious medical and epidemiological problem with approximately 5% of adults and 15 to 70% of children being colonized by C. difficile and the colonization prevalence further increases with hospitalized patients and patients in nursing homes[3]. Also, patients above the age of 65 are more at risk at developing CDI than younger patients[4]. The incidence of CDIs also depends on the length of the hospitalization period where during the first few days of hospitalization the risk is between 2.1 to 20% and longer periods of hospitalization increase the risk to up to 45.4% of getting CDI[5]. In 2015, the Centers for Disease Control and Prevention (CDC) found that C. difficile caused half a million infections and resulted in 15,000 deaths in a single year[6]. Prevention, proper diagnosis and effective treatment are necessary to reduce the risk for the patients, deplete the spreading of infection and diminish the probability of recurrent infection.
Etiology[edit | edit source]
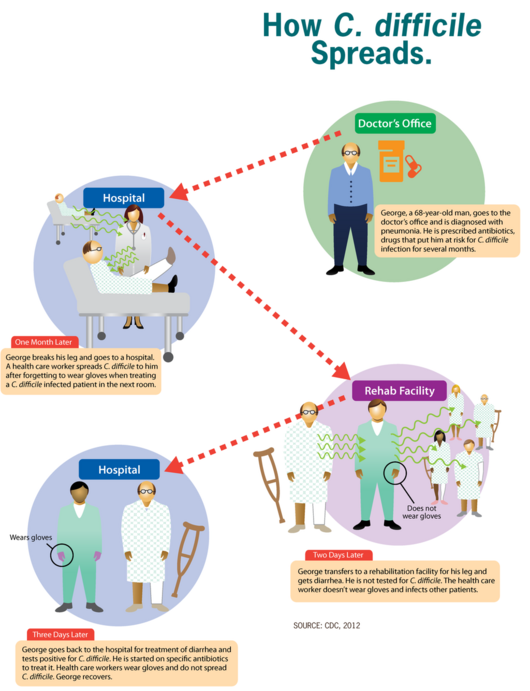
C. diff exists all around us, being in the air, water, soil, and in the feces of humans and animals. C. diff bacteria that are outside the body turn into spores that can live on surfaces for weeks or months. These spores are dormant but they can become active after ingestion, getting into the intestines. C. difficile also naturally occurs in the gut. When the bacterium is present at normal levels, it is not considered to be an infection.
This bacterium does not usually cause problems for people who are otherwise healthy. However, some antibiotics may alter the balance of bacteria in the gut, allowing C. difficile to multiply. It is at this stage that it becomes an infection. The infection can cause diarrhea and increase the risk of more serious illnesses.
Most cases of C. difficile infection occur in healthcare environments, the link here being with antibiotic therapy[6].
Risk Factors[edit | edit source]
C. diff can affect anyone, however cases of C. diff occur when taking antibiotics or not long after finishing taking antibiotics.
Other risk factorsinclude :
- Being 65 or older
- Recent stay at a hospital or nursing home
- A weakened immune system, eg people with HIV/AIDS, cancer, or organ transplant patients taking immunosuppressive drugs
- Previous infection with C. diff or known exposure to the germs[7]
Characteristics/Clinical Presentation[edit | edit source]
Symptoms may develop within a few days after taking antibiotics, and include:
- Severe diarrhea
- Fever
- Stomach tenderness or pain
- Loss of appetite
- Nausea[7]
In a more serious case symptoms peritonitis, septicemia, or perforation of the colon may occur. The risk of experiencing a life threatening condition is higher among older people and those with serious health conditions. Symptoms include:
- Diarrhea more than 10 times a day
- Severe cramping
- Fever
- Nausea
- Loss of appetite/weight loss
- Dehydration
- Rapid heart rate[6]
Diagnosis[edit | edit source]
For definitive diagnosis a stool sample must be collected. Tests include:
- Enzyme immunoassay
- Polymerase chain reaction
- GDH/EIA
- Cell cytotoxicity assay
If a serious problems with the colon is suspected, an X-rays or a CT scan of the intestines may be ordered. In rare cases, the doctor may examine the colon with procedures such as a flexible sigmoidoscopy or colonoscopy[1].
Medical Management[edit | edit source]
Standard treatment for a C. difficile infection is antibiotics. If a person is taking antibiotics when symptoms appear, a doctor may consider stopping that course and prescribing a new type. However, treatment with antibiotics may make a C. difficile infection worse by attacking the helpful bacteria in the body.
Alternative therapies include:
- Probiotics: used to help restore a healthful balance in the intestine. Saccharomyces boulardii (S. boulardii), a natural yeast, can reduce recurring C. difficile infections when a person takes it together with antibiotics. S. boulardii probiotics are available for purchase online.
- Surgery: If symptoms are severe, or if there is organ failure or perforation of the lining of the abdominal wall, it may be necessary to surgically remove the affected part of the colon.
- Fecal microbiota transplantation (FMT): Medical professionals are now using fecal transplants in recurrent cases of C. difficile infection. A healthcare provider will transfer bacteria from a healthy person’s colon into the colon of a person with C. difficile[6].
Physical Therapy Management[edit | edit source]
C. difficile infections are primarily managed through pharmaceutical therapy and associated medical treatments.
The therapist should take an active role in infection control and prevention measures whenever working with these patients. Infection control measures include: donning gloves and gowns prior to entering patients room, washing hands with soap and water upon departure, treating patients in a private room, educating visitors on proper hygiene measures. Routine environmental screening and use of chlorine-containing cleaning agents is also recommended.
References[edit | edit source]
- ↑ 1.0 1.1 Web md Clostridium difficile Available:https://www.webmd.com/digestive-disorders/clostridium-difficile-colitis (accessed 12.5.2022)
- ↑ Cecil J. Clostridium difficile: Changing Epidemiology, Treatment and Infection Prevention Measures. Current Infectious Disease Reports [serial online]. December 2012;14(6):612-619. Available from: MEDLINE, Ipswich, MA. Accessed March 17, 2014
- ↑ Leffler DA, Lamont JT. Clostridium difficile infection. New England Journal of Medicine. 2015 Apr 16;372(16):1539-48.
- ↑ Czepiel J, Kędzierska J, Biesiada G, Birczyńska M, Perucki W, Nowak P, Garlicki A. Epidemiology of Clostridium difficile infection: results of a hospital-based study in Krakow, Poland. Epidemiology & Infection. 2015 Nov;143(15):3235-43.
- ↑ Hung YP, Lin HJ, Wu TC, Liu HC, Lee JC, Lee CI, Wu YH, Wan L, Tsai PJ, Ko WC. Risk factors of fecal toxigenic or non-toxigenic Clostridium difficile colonization: impact of Toll-like receptor polymorphisms and prior antibiotic exposure. PloS one. 2013 Jul 25;8(7):e69577.
- ↑ 6.0 6.1 6.2 6.3 Medical news today What to know about Clostridium difficile Available:https://www.medicalnewstoday.com/articles/172329#what-is-c-difficile (accessed 12.5.2022)
- ↑ 7.0 7.1 CDC C. diff (Clostridioides difficile) Available:https://www.cdc.gov/cdiff/what-is.html (accessed 12.5.2022)