Lung Compliance: Difference between revisions
(Created page with " PULMONARY COMPIANCE: is the total compliance of both lungs, measuring the extent to which the lungs will expand (change in volume of lungs) for each unit increase in...") |
Mohit Chand (talk | contribs) No edit summary |
||
| (70 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editor ''' - [[User:Shalini Varadhan|Shalini Varadhan]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
== Introduction == | |||
[[File:Compliance.png|right|frameless|400x400px]] | |||
Pulmonary compliance, a measure of the [[Lung Anatomy|lung]] expandability, which is important in ideal [[Respiratory System|respiratory]] system function. It refers to the ability of the lungs to stretch and expand. Lung compliance can be calculated by dividing volume by pressure (C = V/P). | |||
* Two factors affecting lung compliance are elasticity from the elastin in[[Connective Tissue Disorders|connective tissue,]] and surface tension which is decreased by surfactant production. | |||
* Lung compliance participates in the lung-chest wall system by opposing the outward pull of chest wall compliance. | |||
* The net compliance (lung-chest wall system) allows the lungs to achieve appropriate functional residual capacity, the volume remaining after passive expiration<ref name=":1">Edwards Z, Annamaraju P. Physiology, Lung Compliance.2020 Available from:https://www.statpearls.com/articlelibrary/viewarticle/24496/ (accessed 17.4.2021)</ref>. | |||
== Transmural Pressures == | |||
The compliance of the lung describes the relationship between the transmural pressure (i.e. pressure passing through a wall/hollow structure) across the lung, compared to the organ's volume. Transmural pressure indicates the relative pressure between the [[alveoli]] and the intrapleural space. Positive transmural pressures indicate greater alveolar pressures than intrapleural pressures.<ref>Iotti G, Braschi A. [https://sofia.medicalistes.fr/spip/IMG/pdf/measurements_of_respiratory_mechanics_during_mechanical_ventilation_lotti_braschi_1999_.pdf Measurements of respiratory mechanics during mechanical ventilation]. Rhäzüns, Switzerland: Hamilton Medical Scientific Library. 1999</ref> | |||
* Although positive transmural pressures are required to expand the lung, they are not achieved by generating positive [[Alveoli|alveolar]] air pressures. Rather, lung expansion is achieved by generating progressively negative pressures within the intrapleural space. Conceptually, one can think of this as inflating a balloon, not by breathing into it and increasing the internal pressure above that of atmospheric pressure, but rather by placing it within a chamber and generating a progressive vacuum around the balloon. Appreciation of this important feature of lung expansion is critical for understanding how lung expansion can be achieved, given the fact that the lung is not physically attached to the chest wall but is separated from the chest wall by the intrapleural space. | |||
* Similar to a balloon, the lungs expand by generating positive transmural pressures. However, unlike a balloon, these positive transmural pressures are generated by creating negative surrounding pressure within the intrapleural space. As shown, the pressure of air within the lungs remains equivalent to that of the atmosphere at the peak inspiration or expiration<ref name=":0">Pathway medicine [http://pathwaymedicine.org/lung-compliance Lung compliance] Available from:http://pathwaymedicine.org/lung-compliance (accessed 17.4.2021)</ref>. | |||
The following video helps explain the different components of transmural pressure: | |||
{{#ev:youtube|ZAF-EN9jfqY}}<ref>Dr. Umar Azizov. Transmural Pressures (transpulmonary, transthoracic, transrespiratory pressure). Available from: https://www.youtube.com/watch?v=ZAF-EN9jfqY&ab_channel=Dr.UmarAzizov (accessed 14 April 2022). </ref> | |||
== Function == | |||
[[File:Compliance curve.PNG|right|frameless]] | |||
Compliance of the respiratory system describes the expandability of the lungs and chest wall. There are two types of compliance: dynamic and static. | |||
# Dynamic compliance describes the compliance measured during breathing, which involves a combination of lung compliance and airway resistance. This is defined as the change in lung volume by the change in pressure, in the presence of flow. | |||
# Static compliance describes pulmonary compliance when there is no airflow, like an inspiratory pause. This is defined as the change in lung volume by the change in pressure, in the absence of flow. | |||
For example, if a person was to fill the lung with pressure and then not move it, the pressure would eventually decrease. This is the static compliance measurement. Dynamic compliance is measured by dividing the tidal volume, the average volume of air in one breath cycle, by the difference between the pressure of the lungs at full inspiration and full expiration C<sub>D</sub>= V<sub>T</sub>/(P<sub>I</sub>-P<sub>E</sub>). | |||
Static compliance is always a higher value than dynamic.<ref name=":2">Infobloom Lung compliance Available from:https://www.infobloom.com/what-is-lung-compliance.htm (accessed 17.4.2021)</ref> | |||
Pressure-volume curves are common schemes to express the relationship of dynamic and static compliance where the slope represents the compliance.<ref>Harris RS. [http://rc.rcjournal.com/content/respcare/50/1/78.full.pdf Pressure-volume curves of the respiratory system]. Respiratory care. 2005; 50(1): 78-99.</ref> The graph at the top of this section would be called a 'Compliance curve', where the top curve represents expiration, airway resistance, and the bottom curve represents inspiration, elastic resistance. The slope of this curve represents dynamic compliance of the lungs. The space in between the curves represents the amount of energy/work needed to surpass the airways resistance during inspiration, and expiration. This phenomenon is known as hysteresis. | |||
It can be seen that the pressure required for inspiration is greater than the pressure required for expiration. With much more or much less compliance, the slope of the curve may be steeper or shallower, respectively. <ref name=":4" /> | |||
'''Rubber Band/Balloon Concept <small>-</small>''' A simple way to understand lung compliance is through the rubber band or balloon concept. | |||
• A tighter rubber band, with more resistance, would be more difficult to stretch, and can readily recoil. | |||
• A loose rubber band, with less resistance, would easily stretch, and wouldn't recoil as easily. | |||
This is analogous to the mechanism of a balloon, and thus the alveoli. Alveoli (or a balloon) which are deflated have a high compliance (ability to stretch and inflate), while alveoli which are inflated have a low compliance. In this respect, it should be noted that each alveoli has a different compliance. <ref>Gilmore, T. Respiratory Cram - Lung Compliance: The Ability to Stretch. Available from: https://respiratorycram.com/lung-compliance-the-ability-to-stretch/ (accessed 15 April 2022)</ref> | |||
== Important Factors == | |||
[[File:Lung and diaphragm.jpg|right|frameless|442x442px]] | |||
As mentioned above, two important factors of lung compliance are elastic fibers and surface tension.<ref name=":3">LibreTexts. Factors Affecting Pulmonary Ventilation: Compliance of the Lungs. [Internet]. 2020 [cited 20 April 2021]. Available from:https://med.libretexts.org/Bookshelves/Anatomy_and_Physiology/Book%3A_Anatomy_and_Physiology_(Boundless)/21%3A_Respiratory_System/21.6%3A_Factors_Affecting_Pulmonary_Ventilation/21.6B%3A_Factors_Affecting_Pulmonary_Ventilation%3A_Compliance_of_the_Lungs </ref> More elastic fibers in the tissue lead to ease in expandability and, therefore, compliance. Surface tension within the alveoli is decreased by the production of surfactant, to prevent collapse. Compliance is more easily achieved by decreasing surface tension. | |||
# Elastin: a highly stretchable protein that is found widely throughout the pulmonary interstitial connective tissue. Molecularly, elastin proteins naturally tend toward a globular structure but can be stretched if a force is applied; however, once the protein is fully extended, the molecule is highly resistant to further stretching. This is similar to a rubber band. The elastic recoil of the lung and its tendency to have higher compliance at lower lung volumes is mainly explained by the combined action of the elastin fibers spread throughout the pulmonary interstitium. These fibers serve to powerfully recoil the lung and only stretch when a force is applied; however, once the lung is stretched to large volumes, these proteins become highly resistant to further stretching. | |||
# Surface Tension: a physical property of water that causes surfaces of water to achieve the smallest possible area. Surface tension arises from the energetic preference of water molecules to interact with one another through hydrogen bonding rather than with air. Individual alveoli all contain a highly thin inner lining of water-based fluid whose surface tension exerts a collapsing force on the alveolus. This is because smaller alveolar volumes would naturally reduce the surface area of the thin fluid lining. | |||
The combined force of surface tension throughout the lung's alveoli serves as a powerful contributor to the elastic recoil of the lung. | |||
Increased lung volumes would require expansion of individual alveoli which is highly resisted by the surface tension of the alveolar fluid inner lining. In fact, the recoiling force of alveolar surface tension is so powerful that special surfactant chemicals must be synthesized and secreted into the inner lining fluid to reduce the surface tension. Failure to produce these surfactants is an important contributor to major pulmonary pathologies, e.g. [[Neonatal Respiratory Distress Syndrome]].<ref name=":0" /> | |||
== Pathophysiology == | |||
[[File:Copd-diagram-of-lungs-blf-695.jpg|right|frameless]] | |||
Changes in lung compliance can indicate issues within the lungs. These generally cause, or are caused by, injuries, illnesses, or impairments. | |||
# A decreased compliance might show [[Restrictive Lung Disease|restrictive lung diseases]]. Restrictive lung disease can result from mechanical issues with peripheral hypoventilation, including poor muscular effort or structural dysfunction. Conditions like [[Muscular Dystrophy|muscular dystrophy]], [[Poliomyelitis|polio]], [[Myasthenia Gravis|myasthenia gravis]], and [[Guillain-Barre Syndrome|Guillain-barre syndrome]] can cause poor muscular effort. [[Scoliosis]] or morbid obesity can also cause structural limitations. | |||
# Increased compliance can be present where there is degeneration of lung tissue. Degenerative lung tissue diseases (e.g. [[emphysema]]) make it harder for the lungs to expand, and harder to exhale as there is less elastic recoil.<ref name=":2" /> | |||
# [[Pulmonary Fibrosis]]: Scarring and hardening of the lung tissue can be caused by environmental factors or pollutants or can be caused from genetic factors. The lung tissue elastin fibers would be replaced by collagen, which is less elastic and more rigid. This would thus decrease lung compliance and increase the work of breathing. <ref name=":4">Desai, Jay P; Moustarah, Fady. National Library of Medicine - Pulmonary Compliance. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538324/ (accessed 14 April 2022)</ref> | |||
# There are cases of lung compliance pathology caused by problems with the surfactant. The recoiling force of alveolar surface tension is so powerful that special surfactant chemicals must be synthesized and secreted into the inner lining fluid to reduce the surface tension. Failure to produce these surfactants is an important contributor to major pulmonary pathologies, such as Neonatal Respiratory Distress Syndrome.<ref name=":0" /><ref name=":2" /> | |||
# [[Pneumothorax]]: This condition characteristically demonstrates the accumulation of air in the intrapleural space. This leads to the equalization of intrapleural pressure with atmospheric pressure. As a result, the chest wall protrudes outward, and [[Atelectasis|lungs collapse]] as this is the natural tendency without transmural pressure. The patient will commonly present with [[dyspnoea]], [[Angina|chest pain]], uneven expansion of the chest, and diminished breath sounds on the affected side. Without proper transmural pressure, lung-chest wall compliance is inoperable.<ref name=":1" /> | |||
# [[Atelectasis]]/ARDS: With the collapse of the lung, or part of the lung, there is a decrease in the volume of the lung, and thus compliance decreases, since a higher pressure would be needed to aerate and inflate the alveoli. <ref name=":4" /> | |||
# [[Obesity]] results in low lung compliance with reduced functional residual capacity and expiratory reserve volume. | |||
# [[Scoliosis]] decreases the chest wall and lung compliance that results in increased respiratory workload. | |||
# [[Older People - An Introduction|Aging]] is accompanied by a decrease in muscular strength and elastic recoil. Therefore, lung compliance increases, and chest wall compliance decreases as age increases.<ref name=":1" /> | |||
{| class="wikitable" | |||
|'''Lung compliance''' | |||
|'''Chest wall compliance''' | |||
|- | |||
|'''Increased lung compliance''' | |||
* Lung surfactant | |||
* Lung volume: compliance is at its highest at FRC | |||
* Posture (supine, upright) | |||
* Loss of lung connective tissue associated with age | |||
* Emphysema | |||
|'''Increased chest wall compliance''' | |||
* Ehler-Dahlos syndrome and other connective tissue diseases | |||
* Rib resection | |||
* Cachexia | |||
* Flail segment rib fractures | |||
* Open chest (eg clamshell) | |||
|- | |||
|'''Decreased static lung compliance''' | |||
* Loss of surfactant (eg. ARDS) | |||
* Decreased lung elasticity | |||
** Pulmonary fibrosis<ref name=":3" /> | |||
** Pulmonary oedema | |||
* Decreased functional lung volume | |||
** Pneumonectomy or lobectomy | |||
** [[Pneumonia]] | |||
** Atelectasis | |||
** Small stature | |||
* Alveolar derecruitment | |||
* Alveolar overdistension | |||
'''Decreased dynamic lung compliance''' | |||
* Increased airway resistance (eg. asthma) | |||
* Increased airflow (increased resp rate) | |||
|'''Decreased chest wall compliance''' | |||
* Structural abnormalities | |||
** Kyphosis/scoliosis | |||
** Pectus excavatum | |||
** Circumferential burns | |||
** Surgical rib fixation | |||
* Functional abnormalities | |||
** Muscle spasm, eg. seizure or tetanus | |||
* Extrathoracic influences on chest/diaphragmatic excursion | |||
** Obesity | |||
** Abdominal compartment syndrome | |||
** Prone position | |||
|} | |||
Here is a video summarizing lung and chest wall compliance: | |||
{{#ev:youtube|AWKTCwmXopY}}<ref>Byte Size Med. Lung and Chest Wall Compliance | Breathing Mechanics | Respiratory Physiology. Available from: https://www.youtube.com/watch?v=AWKTCwmXopY&t=2s&ab_channel=ByteSizeMed (accessed 14 May 2022).</ref> | |||
== References == | |||
<references /> | |||
[[Category:Respiratory]] | |||
Latest revision as of 19:18, 10 April 2024
Original Editor - Shalini Varadhan
Top Contributors - Kapil Narale, Shalini Varadhan, Lucinda hampton, Kim Jackson, Uchechukwu Chukwuemeka and Mohit Chand
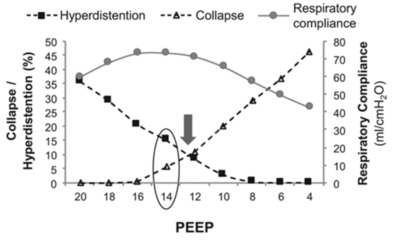
Introduction[edit | edit source]
Pulmonary compliance, a measure of the lung expandability, which is important in ideal respiratory system function. It refers to the ability of the lungs to stretch and expand. Lung compliance can be calculated by dividing volume by pressure (C = V/P).
- Two factors affecting lung compliance are elasticity from the elastin inconnective tissue, and surface tension which is decreased by surfactant production.
- Lung compliance participates in the lung-chest wall system by opposing the outward pull of chest wall compliance.
- The net compliance (lung-chest wall system) allows the lungs to achieve appropriate functional residual capacity, the volume remaining after passive expiration[1].
Transmural Pressures[edit | edit source]
The compliance of the lung describes the relationship between the transmural pressure (i.e. pressure passing through a wall/hollow structure) across the lung, compared to the organ's volume. Transmural pressure indicates the relative pressure between the alveoli and the intrapleural space. Positive transmural pressures indicate greater alveolar pressures than intrapleural pressures.[2]
- Although positive transmural pressures are required to expand the lung, they are not achieved by generating positive alveolar air pressures. Rather, lung expansion is achieved by generating progressively negative pressures within the intrapleural space. Conceptually, one can think of this as inflating a balloon, not by breathing into it and increasing the internal pressure above that of atmospheric pressure, but rather by placing it within a chamber and generating a progressive vacuum around the balloon. Appreciation of this important feature of lung expansion is critical for understanding how lung expansion can be achieved, given the fact that the lung is not physically attached to the chest wall but is separated from the chest wall by the intrapleural space.
- Similar to a balloon, the lungs expand by generating positive transmural pressures. However, unlike a balloon, these positive transmural pressures are generated by creating negative surrounding pressure within the intrapleural space. As shown, the pressure of air within the lungs remains equivalent to that of the atmosphere at the peak inspiration or expiration[3].
The following video helps explain the different components of transmural pressure:
Function[edit | edit source]
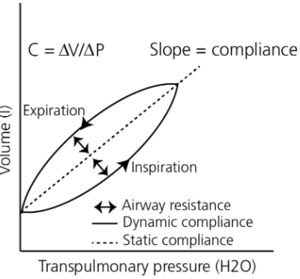
Compliance of the respiratory system describes the expandability of the lungs and chest wall. There are two types of compliance: dynamic and static.
- Dynamic compliance describes the compliance measured during breathing, which involves a combination of lung compliance and airway resistance. This is defined as the change in lung volume by the change in pressure, in the presence of flow.
- Static compliance describes pulmonary compliance when there is no airflow, like an inspiratory pause. This is defined as the change in lung volume by the change in pressure, in the absence of flow.
For example, if a person was to fill the lung with pressure and then not move it, the pressure would eventually decrease. This is the static compliance measurement. Dynamic compliance is measured by dividing the tidal volume, the average volume of air in one breath cycle, by the difference between the pressure of the lungs at full inspiration and full expiration CD= VT/(PI-PE).
Static compliance is always a higher value than dynamic.[5]
Pressure-volume curves are common schemes to express the relationship of dynamic and static compliance where the slope represents the compliance.[6] The graph at the top of this section would be called a 'Compliance curve', where the top curve represents expiration, airway resistance, and the bottom curve represents inspiration, elastic resistance. The slope of this curve represents dynamic compliance of the lungs. The space in between the curves represents the amount of energy/work needed to surpass the airways resistance during inspiration, and expiration. This phenomenon is known as hysteresis.
It can be seen that the pressure required for inspiration is greater than the pressure required for expiration. With much more or much less compliance, the slope of the curve may be steeper or shallower, respectively. [7]
Rubber Band/Balloon Concept - A simple way to understand lung compliance is through the rubber band or balloon concept.
• A tighter rubber band, with more resistance, would be more difficult to stretch, and can readily recoil.
• A loose rubber band, with less resistance, would easily stretch, and wouldn't recoil as easily.
This is analogous to the mechanism of a balloon, and thus the alveoli. Alveoli (or a balloon) which are deflated have a high compliance (ability to stretch and inflate), while alveoli which are inflated have a low compliance. In this respect, it should be noted that each alveoli has a different compliance. [8]
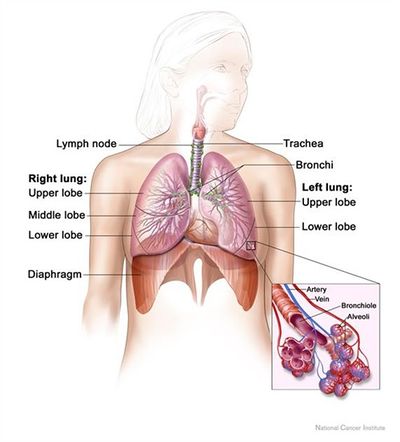
Important Factors[edit | edit source]
As mentioned above, two important factors of lung compliance are elastic fibers and surface tension.[9] More elastic fibers in the tissue lead to ease in expandability and, therefore, compliance. Surface tension within the alveoli is decreased by the production of surfactant, to prevent collapse. Compliance is more easily achieved by decreasing surface tension.
- Elastin: a highly stretchable protein that is found widely throughout the pulmonary interstitial connective tissue. Molecularly, elastin proteins naturally tend toward a globular structure but can be stretched if a force is applied; however, once the protein is fully extended, the molecule is highly resistant to further stretching. This is similar to a rubber band. The elastic recoil of the lung and its tendency to have higher compliance at lower lung volumes is mainly explained by the combined action of the elastin fibers spread throughout the pulmonary interstitium. These fibers serve to powerfully recoil the lung and only stretch when a force is applied; however, once the lung is stretched to large volumes, these proteins become highly resistant to further stretching.
- Surface Tension: a physical property of water that causes surfaces of water to achieve the smallest possible area. Surface tension arises from the energetic preference of water molecules to interact with one another through hydrogen bonding rather than with air. Individual alveoli all contain a highly thin inner lining of water-based fluid whose surface tension exerts a collapsing force on the alveolus. This is because smaller alveolar volumes would naturally reduce the surface area of the thin fluid lining.
The combined force of surface tension throughout the lung's alveoli serves as a powerful contributor to the elastic recoil of the lung.
Increased lung volumes would require expansion of individual alveoli which is highly resisted by the surface tension of the alveolar fluid inner lining. In fact, the recoiling force of alveolar surface tension is so powerful that special surfactant chemicals must be synthesized and secreted into the inner lining fluid to reduce the surface tension. Failure to produce these surfactants is an important contributor to major pulmonary pathologies, e.g. Neonatal Respiratory Distress Syndrome.[3]
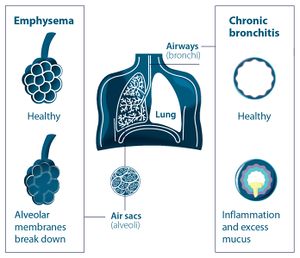
Pathophysiology[edit | edit source]
Changes in lung compliance can indicate issues within the lungs. These generally cause, or are caused by, injuries, illnesses, or impairments.
- A decreased compliance might show restrictive lung diseases. Restrictive lung disease can result from mechanical issues with peripheral hypoventilation, including poor muscular effort or structural dysfunction. Conditions like muscular dystrophy, polio, myasthenia gravis, and Guillain-barre syndrome can cause poor muscular effort. Scoliosis or morbid obesity can also cause structural limitations.
- Increased compliance can be present where there is degeneration of lung tissue. Degenerative lung tissue diseases (e.g. emphysema) make it harder for the lungs to expand, and harder to exhale as there is less elastic recoil.[5]
- Pulmonary Fibrosis: Scarring and hardening of the lung tissue can be caused by environmental factors or pollutants or can be caused from genetic factors. The lung tissue elastin fibers would be replaced by collagen, which is less elastic and more rigid. This would thus decrease lung compliance and increase the work of breathing. [7]
- There are cases of lung compliance pathology caused by problems with the surfactant. The recoiling force of alveolar surface tension is so powerful that special surfactant chemicals must be synthesized and secreted into the inner lining fluid to reduce the surface tension. Failure to produce these surfactants is an important contributor to major pulmonary pathologies, such as Neonatal Respiratory Distress Syndrome.[3][5]
- Pneumothorax: This condition characteristically demonstrates the accumulation of air in the intrapleural space. This leads to the equalization of intrapleural pressure with atmospheric pressure. As a result, the chest wall protrudes outward, and lungs collapse as this is the natural tendency without transmural pressure. The patient will commonly present with dyspnoea, chest pain, uneven expansion of the chest, and diminished breath sounds on the affected side. Without proper transmural pressure, lung-chest wall compliance is inoperable.[1]
- Atelectasis/ARDS: With the collapse of the lung, or part of the lung, there is a decrease in the volume of the lung, and thus compliance decreases, since a higher pressure would be needed to aerate and inflate the alveoli. [7]
- Obesity results in low lung compliance with reduced functional residual capacity and expiratory reserve volume.
- Scoliosis decreases the chest wall and lung compliance that results in increased respiratory workload.
- Aging is accompanied by a decrease in muscular strength and elastic recoil. Therefore, lung compliance increases, and chest wall compliance decreases as age increases.[1]
| Lung compliance | Chest wall compliance |
Increased lung compliance
|
Increased chest wall compliance
|
Decreased static lung compliance
Decreased dynamic lung compliance
|
Decreased chest wall compliance
|
Here is a video summarizing lung and chest wall compliance:
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Edwards Z, Annamaraju P. Physiology, Lung Compliance.2020 Available from:https://www.statpearls.com/articlelibrary/viewarticle/24496/ (accessed 17.4.2021)
- ↑ Iotti G, Braschi A. Measurements of respiratory mechanics during mechanical ventilation. Rhäzüns, Switzerland: Hamilton Medical Scientific Library. 1999
- ↑ 3.0 3.1 3.2 Pathway medicine Lung compliance Available from:http://pathwaymedicine.org/lung-compliance (accessed 17.4.2021)
- ↑ Dr. Umar Azizov. Transmural Pressures (transpulmonary, transthoracic, transrespiratory pressure). Available from: https://www.youtube.com/watch?v=ZAF-EN9jfqY&ab_channel=Dr.UmarAzizov (accessed 14 April 2022).
- ↑ 5.0 5.1 5.2 Infobloom Lung compliance Available from:https://www.infobloom.com/what-is-lung-compliance.htm (accessed 17.4.2021)
- ↑ Harris RS. Pressure-volume curves of the respiratory system. Respiratory care. 2005; 50(1): 78-99.
- ↑ 7.0 7.1 7.2 Desai, Jay P; Moustarah, Fady. National Library of Medicine - Pulmonary Compliance. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538324/ (accessed 14 April 2022)
- ↑ Gilmore, T. Respiratory Cram - Lung Compliance: The Ability to Stretch. Available from: https://respiratorycram.com/lung-compliance-the-ability-to-stretch/ (accessed 15 April 2022)
- ↑ 9.0 9.1 LibreTexts. Factors Affecting Pulmonary Ventilation: Compliance of the Lungs. [Internet]. 2020 [cited 20 April 2021]. Available from:https://med.libretexts.org/Bookshelves/Anatomy_and_Physiology/Book%3A_Anatomy_and_Physiology_(Boundless)/21%3A_Respiratory_System/21.6%3A_Factors_Affecting_Pulmonary_Ventilation/21.6B%3A_Factors_Affecting_Pulmonary_Ventilation%3A_Compliance_of_the_Lungs
- ↑ Byte Size Med. Lung and Chest Wall Compliance | Breathing Mechanics | Respiratory Physiology. Available from: https://www.youtube.com/watch?v=AWKTCwmXopY&t=2s&ab_channel=ByteSizeMed (accessed 14 May 2022).