Central Cord Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| (6 intermediate revisions by 4 users not shown) | |||
| Line 8: | Line 8: | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
To understand the clinical presentation and pathological process, it is | To understand the clinical presentation and pathological process, it is essential to have knowledge about somatotopic arrangement of tracts in [[Spinal cord anatomy|the spinal cord]]. Somatotopic arrangement of tracts, mainly lateral [[Corticospinal Tract|corticospinal tract]], [[Dorsal Column Medial Lemniscal Pathway|dorsal column pathway]], and lateral [[spinothalamic tract]] are important to understand. | ||
== Epidemiology == | == Epidemiology == | ||
| Line 15: | Line 15: | ||
* It can occasionally be missed if the patient has mild symptoms at the initial presentation. | * It can occasionally be missed if the patient has mild symptoms at the initial presentation. | ||
* Studies reported a bimodal age distribution, however, with about 30% between 10 to 30 years old and 70% older than 40 years. | * Studies reported a bimodal age distribution, however, with about 30% between 10 to 30 years old and 70% older than 40 years. | ||
* | * Males are most affected than females.<ref>Schadler P, Shue J, Girardi F. [https://www.jscimedcentral.com/Neurosurgery/neurosurgery-4-1075.pdf Central Cord Syndrome: A Review of Epidemiology, Treatment and Prognostic Factors.] JSM Neurosurgery and Spine. 2016;4:1075.</ref> | ||
== Mechanism of Injury == | == Mechanism of Injury == | ||
In elderly, | In elderly, | ||
* | * Underlying [[Cervical Spondylosis|cervical spondylosis]] (stress defects) with minor hyperextension trauma or fall may cause CCS (most common). | ||
* This usually happens with a forward fall while striking the chin, and having the neck extend backward at the time of the fall.<ref name=":0">Ameer MA, Gallagher MA, Gillis CC. [https://www.ncbi.nlm.nih.gov/books/NBK441932/ Central Cord Syndrome.] StatPearls [Internet]. 2020 Jan.</ref> | * This usually happens with a forward fall while striking the chin, and having the neck extend backward at the time of the fall.<ref name=":0">Ameer MA, Gallagher MA, Gillis CC. [https://www.ncbi.nlm.nih.gov/books/NBK441932/ Central Cord Syndrome.] StatPearls [Internet]. 2020 Jan.</ref> | ||
* >90% of patients with CCS aged >40 years have been shown to have underlying cervical spine conditions, such as spondylosis with osteophyte formation, canal | * >90% of patients with CCS aged >40 years have been shown to have underlying [[Cervical Anatomy|cervical spine]] conditions, such as spondylosis with osteophyte formation, <u>[[Cervical Stenosis|canal stenos]]</u>[[Cervical Stenosis|is]], and ossification of the [[posterior longitudinal ligament]].<ref name=":1">Nowak DD, Lee JK, Gelb DE, Poelstra KA, Ludwig SC. [http://upload.orthobullets.com/journalclub/free_pdf/19948700_19948700.pdf Central cord syndrome.] JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2009 Dec 1;17(12):756-65.</ref> | ||
In adult, | In adult, | ||
* sustain higher velocity of trauma, leading to cervical spine instability/fracture (most common)or traumatic disk herniation.<ref name=":0" /> | * sustain higher velocity of trauma, leading to cervical spine instability/fracture (most common) or traumatic disk herniation.<ref name=":0" /> | ||
Less common causes including, | Less common causes including, | ||
* [https://physio-pedia.com/Cervical_Spondylosis?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share Cervical spondylosis], | * [https://physio-pedia.com/Cervical_Spondylosis?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share Cervical spondylosis], | ||
* Atlantoaxial instability, | * [[Atlantoaxial Osteoarthritis|Atlantoaxial]] instability, | ||
* [https://physio-pedia.com/Tethered_Cord_Syndrome?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share Tethered cord], | * [https://physio-pedia.com/Tethered_Cord_Syndrome?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share Tethered cord], | ||
* Spinal arthropathies. | * Spinal arthropathies. | ||
| Line 37: | Line 37: | ||
* Injury to the central gray matter and cord hemorrhage were thought to be the main causes of CCS. | * Injury to the central gray matter and cord hemorrhage were thought to be the main causes of CCS. | ||
* However, recent studies have shown that the lateral cortical spinal tract in the mid to upper cervical spine contains the main area of pathologic abnormality. | * However, recent studies have shown that the lateral cortical spinal tract in the mid to upper cervical spine contains the main area of pathologic abnormality. | ||
* Patients with CCS exhibit | * Patients with CCS exhibit [[Wallerian Degeneration|Wallerian degeneration]] of the axonal tracts distal to the zone of injury in the lateral corticospinal tracts. | ||
* The motor-evoked potentials were more severely affected than the somatosensory-evoked potentials, and the hand musculature, particularly the abductor pollicis brevis, was most severely affected. | * The motor-evoked potentials were more severely affected than the somatosensory-evoked potentials, and the hand musculature, particularly the abductor pollicis brevis, was most severely affected. | ||
* Thus, injury to the large myelinated axons of the lateral corticospinal tract seems to be the main cause of the deficits associated with CCS. This explains the primary involvement of the fine motor movements of the distal upper extremity.<ref name=":1" /> | * Thus, injury to the large myelinated axons of the lateral corticospinal tract seems to be the main cause of the deficits associated with CCS. This explains the primary involvement of the fine motor movements of the distal upper extremity.<ref name=":1" /> | ||
| Line 50: | Line 50: | ||
=== Sensory === | === Sensory === | ||
Pain and temperature sensations are lost | Pain and temperature sensations are lost below the level of the lesion due to the involvement of the medial aspect of tracts, mainly the upper extremity, and trunk. Thus, the most common sensory deficits are found in a "cape-like" distribution across their upper back and down their posterior upper extremities.<ref name=":0" /> | ||
=== Bowel, bladder, and sexual === | === Bowel, bladder, and sexual === | ||
Bladder dysfunction, typically urinary retention and priapism, may be present in more severe cases. The sacral sensation is usually preserved, but the rectal tone should be assessed for the severity of the compression.<ref name=":0" /> <ref name=":2">Rich V, McCaslin E. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1569555/#:~:text=The%20differential%20diagnosis%20for%20CCS,and%20symptoms%20of%20each%20condition. Central cord syndrome in a high school wrestler: a case report.] Journal of Athletic Training. 2006;41(3):341.</ref> | Bladder dysfunction, typically urinary retention and priapism, may be present in more severe cases. The sacral sensation is usually preserved, but the rectal tone should be assessed for the severity of the compression.<ref name=":0" /> <ref name=":2">Rich V, McCaslin E. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1569555/#:~:text=The%20differential%20diagnosis%20for%20CCS,and%20symptoms%20of%20each%20condition. Central cord syndrome in a high school wrestler: a case report.] Journal of Athletic Training. 2006;41(3):341.</ref> | ||
{{#ev:youtube|PTNE13R7t6o}}<ref> https://www.youtube.com/watch?v=PTNE13R7t6o. [lasted accessed: 29th Dec, 2020]</ref> | {{#ev:youtube|PTNE13R7t6o}}<ref>https://www.youtube.com/watch?v=PTNE13R7t6o. [lasted accessed: 29th Dec, 2020]</ref> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 69: | Line 69: | ||
In evaluating a patient with SCI, it is essential to determine the extent of neurologic injury (ie, incomplete versus complete). Incomplete injuries have a greater chance for neurologic recovery, whereas motor recovery is achieved in only 3% of patients with complete injury during the first 24 hours and never after 24 to 48 hours. | In evaluating a patient with SCI, it is essential to determine the extent of neurologic injury (ie, incomplete versus complete). Incomplete injuries have a greater chance for neurologic recovery, whereas motor recovery is achieved in only 3% of patients with complete injury during the first 24 hours and never after 24 to 48 hours. | ||
With the help of [[American Spinal Cord Injury Association (ASIA) Impairment Scale|American Spinal | With the help of [[American Spinal Cord Injury Association (ASIA) Impairment Scale|American Spinal Injury (AISA) Impairment Scale [AIS]]], the neurological level and complete -incomplete spinal cord injury level can be identified. | ||
An accurate system of the clinical neurologic assessment and recording influences treatment decisions allows for reliable serial monitoring, and provides prognostic information. | An accurate system of the clinical neurologic assessment and recording influences treatment decisions allows for reliable serial monitoring, and provides prognostic information. | ||
| Line 100: | Line 100: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
* [[Stroke|Middle Cerebral Artery (MCA) stroke.]] | * [[Stroke|Middle Cerebral Artery (MCA) stroke.]] | ||
* Brown-Séquard syndrome | * [[Brown-Sequard Syndrome|Brown-Séquard syndrome]] | ||
* [[Brachial plexus injury]] | * [[Brachial plexus injury]] | ||
* Anterior cord syndrome | * [[Anterior Cord Syndrome|Anterior cord syndrome]] | ||
* Burning hands syndrome<ref name=":2" /> | * Burning hands syndrome<ref name=":2" /> | ||
* [[Syringomyelia]] | * [[Syringomyelia]] | ||
Latest revision as of 18:00, 21 June 2023
Top Contributors - Manisha Shrestha, Kim Jackson, Lucinda hampton, Anas Mohamed, Stacy Schiurring and Rosie Swift
Introduction[edit | edit source]
Central cord syndrome (CCS) is the most commonly encountered incomplete spinal cord injury (SCI) type. CCS was first described in 1954 by Schneider et al. as SCI with “disproportionately more motor impairment of the upper than of the lower extremities, bladder dysfunction, usually urinary retention, and varying degrees of sensory loss below the level of the lesion.”[1]
Clinically Relevant Anatomy[edit | edit source]
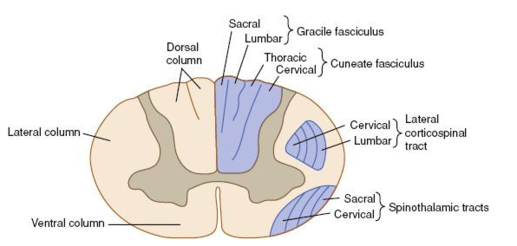
To understand the clinical presentation and pathological process, it is essential to have knowledge about somatotopic arrangement of tracts in the spinal cord. Somatotopic arrangement of tracts, mainly lateral corticospinal tract, dorsal column pathway, and lateral spinothalamic tract are important to understand.
Epidemiology[edit | edit source]
- The estimated incidence of spinal cord injury in the United States is 17,000 new cases each year. The majority of patients are males involved in car accidents, falls, or acts of violence.
- Incomplete injuries are currently the most frequent neurological category with about 60%. Among incomplete cord injuries, central cord syndrome is the most common type, ranging from 40 to 70% of cases.
- It can occasionally be missed if the patient has mild symptoms at the initial presentation.
- Studies reported a bimodal age distribution, however, with about 30% between 10 to 30 years old and 70% older than 40 years.
- Males are most affected than females.[2]
Mechanism of Injury[edit | edit source]
In elderly,
- Underlying cervical spondylosis (stress defects) with minor hyperextension trauma or fall may cause CCS (most common).
- This usually happens with a forward fall while striking the chin, and having the neck extend backward at the time of the fall.[3]
- >90% of patients with CCS aged >40 years have been shown to have underlying cervical spine conditions, such as spondylosis with osteophyte formation, canal stenosis, and ossification of the posterior longitudinal ligament.[4]
In adult,
- sustain higher velocity of trauma, leading to cervical spine instability/fracture (most common) or traumatic disk herniation.[3]
Less common causes including,
- Cervical spondylosis,
- Atlantoaxial instability,
- Tethered cord,
- Spinal arthropathies.
- Syringomyelia
- Spinal epidural abscess[3][4]
Pathological process[edit | edit source]
- CCS originally was theorized to consist of injury to the central gray matter and the central portion of the long tracts, with preservation of the peripheral structures.
- Injury to the central gray matter and cord hemorrhage were thought to be the main causes of CCS.
- However, recent studies have shown that the lateral cortical spinal tract in the mid to upper cervical spine contains the main area of pathologic abnormality.
- Patients with CCS exhibit Wallerian degeneration of the axonal tracts distal to the zone of injury in the lateral corticospinal tracts.
- The motor-evoked potentials were more severely affected than the somatosensory-evoked potentials, and the hand musculature, particularly the abductor pollicis brevis, was most severely affected.
- Thus, injury to the large myelinated axons of the lateral corticospinal tract seems to be the main cause of the deficits associated with CCS. This explains the primary involvement of the fine motor movements of the distal upper extremity.[4]
Clinical Presentation[edit | edit source]
Somatotopic arrangement of tracts in the spinal cord gives a wide idea about the clinical presentation of patient with central cord syndrome. At the level of injury, the lower motor neuron lesion type of features is seen whereas below the level of injury upper motor neuron lesion kind of features are seen. It is generally unilateral, but is seen bilaterally in about 10% of cases.
The palpation of the spinous processes elicited tenderness and an increase in pain.
Motor[edit | edit source]
Since in the medial aspect of corticospinal tracts fibers from upper extremity and trunk are involved, the upper extremities are more severely affected than the lower extremities. In particular, the hands and forearms are most affected.
Sensory[edit | edit source]
Pain and temperature sensations are lost below the level of the lesion due to the involvement of the medial aspect of tracts, mainly the upper extremity, and trunk. Thus, the most common sensory deficits are found in a "cape-like" distribution across their upper back and down their posterior upper extremities.[3]
Bowel, bladder, and sexual[edit | edit source]
Bladder dysfunction, typically urinary retention and priapism, may be present in more severe cases. The sacral sensation is usually preserved, but the rectal tone should be assessed for the severity of the compression.[3] [6]
Diagnostic Procedures[edit | edit source]
Rapid and accurate diagnosis is essential in a patient with suspected SCI.
A full radiographic evaluation should be done, typically consisting of crosstable lateral, AP, and open-mouth odontoid views.
Computer Tomography (CT) is frequently performed either in addition to or instead of traditional radiography. Because of the approximately 10% to 20% incidence of noncontiguous spine fractures, when a cervical spine fracture is identified via CT.
MRI can be useful in further assessing the presence of soft-tissue injury or cord compression. MRI evaluation typically includes axial, coronal, and sagittal sections of T1- and T2- weighted images.[4]
Outcome Measures[edit | edit source]
In evaluating a patient with SCI, it is essential to determine the extent of neurologic injury (ie, incomplete versus complete). Incomplete injuries have a greater chance for neurologic recovery, whereas motor recovery is achieved in only 3% of patients with complete injury during the first 24 hours and never after 24 to 48 hours.
With the help of American Spinal Injury (AISA) Impairment Scale [AIS], the neurological level and complete -incomplete spinal cord injury level can be identified.
An accurate system of the clinical neurologic assessment and recording influences treatment decisions allows for reliable serial monitoring, and provides prognostic information.
For further details about outcome tools in SCI, please look into these pages:
Management / Interventions[edit | edit source]
Non- surgical management[edit | edit source]
Observed neurological improvement is the most compelling reason not to proceed with surgical treatment in favor of non-surgical management of CCS. Nonsurgical treatment consists of immobilization of the neck with a rigid cervical collar, medication like high-dose steroids, and extensive rehabilitation with physical and occupational therapy.
For physiotherapy management, please look into these pages:
- Therapeutic Interventions for Spinal Cord Injury
- Physiotherapy Management of Individuals with Spinal Cord Injury
- Respiratory Management in Spinal Cord Injury
- Contracture Management in Spinal Cord Injury
Surgical management[edit | edit source]
- There is a literature dilemma of whether surgery is beneficial or not. Guidelines published in 2016 recommend that "early surgery be considered as a treatment option in an adult patient with traumatic central cord syndrome." [3]
Prognosis[edit | edit source]
- The prognosis for central cord syndrome varies, but most people whose syndrome is caused by trauma have some recovery of neurological function.
- Those who receive medical intervention soon after their injury often have good outcomes.
- Improvement occurs first in the legs, then the bladder, and may be seen in the arms. Hand function recovers last, if at all.
- Recovery is generally better in younger patients, compared to those over the age of 50.[8]
Differential Diagnosis[edit | edit source]
- Middle Cerebral Artery (MCA) stroke.
- Brown-Séquard syndrome
- Brachial plexus injury
- Anterior cord syndrome
- Burning hands syndrome[6]
- Syringomyelia
- Intramedullary tumor[9]
References[edit | edit source]
- ↑ Divi SN, Schroeder GD, Mangan JJ, Tadley M, Ramey WL, Badhiwala JH, Fehlings MG, Oner FC, Kandziora F, Benneker LM, Vialle EN. Management of acute traumatic central cord syndrome: a narrative review. Global spine journal. 2019 May;9(1_suppl):89S-97S.
- ↑ Schadler P, Shue J, Girardi F. Central Cord Syndrome: A Review of Epidemiology, Treatment and Prognostic Factors. JSM Neurosurgery and Spine. 2016;4:1075.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Ameer MA, Gallagher MA, Gillis CC. Central Cord Syndrome. StatPearls [Internet]. 2020 Jan.
- ↑ 4.0 4.1 4.2 4.3 Nowak DD, Lee JK, Gelb DE, Poelstra KA, Ludwig SC. Central cord syndrome. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2009 Dec 1;17(12):756-65.
- ↑ Alec Weir. MR:EM Central Cord Syndrome. Available from: https://www.youtube.com/watch?v=aPcJe-uWbuU[lasted accessed: 29th Dec, 2020]
- ↑ 6.0 6.1 Rich V, McCaslin E. Central cord syndrome in a high school wrestler: a case report. Journal of Athletic Training. 2006;41(3):341.
- ↑ https://www.youtube.com/watch?v=PTNE13R7t6o. [lasted accessed: 29th Dec, 2020]
- ↑ National Institute of Neurological Disorders and Stroke (NINDS). Central Cord Syndrome Information Page [Internet]. Available from:https://www.ninds.nih.gov/Disorders/All-Disorders/Central-Cord-Syndrome-Information-Page [ last accessed: Dec 26, 2020]
- ↑ Živković S, Ali ST, El-Dokla AM. Translational Correlation: Disorders of the Spinal Cord. InConn's Translational Neuroscience 2017 Jan 1 (pp. 489-494). Academic Press.