Bipolar Disorder: Difference between revisions
mNo edit summary |
No edit summary |
||
| (29 intermediate revisions by 7 users not shown) | |||
| Line 2: | Line 2: | ||
'''Original Editors '''- [[User:Michael Thompson|Michael Thompson]] as part of the [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | '''Original Editors '''- [[User:Michael Thompson|Michael Thompson]] as part of the [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
<br>Bipolar disorder, once known as manic depression, is a mood disorder experienced by between 1% and 6% of the population. It’s generally a lifelong condition, characterised by swings in mood: from highs that can tip into mania, to lows that can plunge into depression. | |||
Historically, these moods have been the concern of psychiatrists and have therefore been framed in medical terms. Everyone experiences variations in mood, but for people with bipolar disorder these variations are extreme, and require psychiatric and psychological assistance.<ref name=":0">The Conversation [https://theconversation.com/explainer-what-is-bipolar-disorder-7502 Explainer: what is bipolar disorder?] Available:https://theconversation.com/explainer-what-is-bipolar-disorder-7502 (accessed 4.9.2021)</ref> | |||
This one minute video is about Bipolar Disorder{{#ev:youtube|XQ2PbPr2AH4}} | |||
== | == Etiology == | ||
Like most psychiatric disorders, the causes of bipolar disorder are complex and multifactorial. Not surprisingly, there is strong familial transmission of the disorder, as the child is exposed to both genetic and environmental risk factors. | |||
There is also a strong developmental trajectory in bipolar disorder, with early episodes of depression typically occurring in adolescence, followed by a defining manic episode in early adulthood.<ref name=":0" /> | |||
== Epidemiolgy == | |||
< | [[Image:Bipolar-disorder-symptoms.jpg|Courtesy of Bipolar Disorder Symptoms (http://cureanxiety.com/bipolar-disorder-symptoms)|alt=|right|frameless|399x399px]] The Depression and Bipolar Support Alliance has estimated that close to 6 million Americans are affected by bipolar disorder every year. Bipolar disorder can affect anyone at any age and is found in all races, ethnic groups and social classes with the typical onset being 25 years old. Patients may be diagnosed in their early childhood to as late as the 4th and 5th decades of life. Bipolar disorder is not gender-based and can affect men and women equally. Although, studies have shown that women with Bipolar disorder have more depressive and mixed episodes than men with the disorder. More than 66% of people diagnosed with Bipolar disorder have at least one primary family member with the illness<ref name="DBSA 1">Depression and Bipolar Support Alliance. Bipolar disorder statistics. http://www.dbsalliance.org/site/PageServer?pagename=about_statistics_bipolar (accessed 17 March 2011).</ref>. | ||
The incidence of Bipolar disorder in other countries is notable as well. In Australia it is approximately 238,957 people, in the United Kingdom it is approximately 723,248 people, in Germany it is approximately 989,095 people, in Canada it is approximately 390,094 people, in Iran it is approximately 810,038 people and for both India and China it is approximately 12-15 million people<ref name="BL 1">Bipolar-Lives. Bipolar disorder statistics. http://www.bipolar-lives.com/bipolar-disorder-statistics.html (accessed 17 March 2011).</ref>. | |||
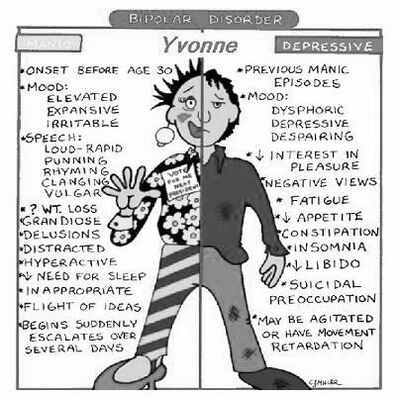
== Characteristics/Clinical Presentation == | |||
[[File:Bipolar.jpeg|right|frameless|423x423px]] | |||
Note - patients can present in a mixed state which includes features from both 'poles' of BD. | |||
# General Appearance: A patient with mania is often hyperkinetic, unpredictable, and erratic. They often are garishly dressed, display negligence of social propriety--demonstrable via excessive friendliness, boundary violations, agitation, or other improprieties--and appear to be unnaturally "happy" or euphoric, however, irritability is also observed, dispositionally. | |||
# Mood and Affect: Mood is often elevated or euphoric, in mania. Affect is often heightened, intense, and extremely lability. Implicit with the affective lability of mania are hyperactivity and severe mobility. When presenting in a depressive state, the patient will report a sad or elegiac mood, while expressing a congruent affect (often tearful). | |||
# Speech: A manic patient will demonstrate pressured speech, which implies a rapid and continuous production of speech that is difficult to interrupt. Reciprocally, speech is slow and soft, in depression. | |||
# Perception: Mood delusions may be present in either the depressed or manic phase (e.g. delusions of guilt during depressed phases or grandiose delusions of power and wealth during manic phases) A manic patient can also have mood-incongruent delusions. | |||
# Thought Process and Content: Patients with mania demonstrate easy distractibility, lack of concentration, illogical condensations, delusions of grandiosity, and flight of ideas. A depressed patient usually has negative thoughts and negative ruminations. | |||
# Sensorium and Cognition: Usually oriented to person, place, and time. Depressed patients may have some impairment in cognition and memory. Manic patients may have a grossly intact [[memory]]. Sometimes orientation is impaired and is called manic delirium. | |||
# Impulse Control: Extremely depressed patients demonstrate lack of willpower. Manic patients are threatening and assaultive. | |||
# Judgment and Insight: Impaired judgment is the distinctive feature of mania along with limited insight. [[Depression|Depressed]] patients often overemphasize their symptoms. | |||
# Reliability: Manic patients are usually unreliable in the information they provide. Depressed patients overemphasize.<ref name=":1">Jain A, Mitra P. [https://www.ncbi.nlm.nih.gov/books/NBK558998/ Bipolar affective disorder.] StatPearls [Internet]. 2021 May 18.Available:https://www.ncbi.nlm.nih.gov/books/NBK558998/ (accessed 4.9.2021)</ref> | |||
| | |||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
[[File:Drug addict.jpeg|right|frameless]] | |||
[[Multimorbidity|Co-morbidities]] range from mental health disease all the way to physical system disorders<ref name="PT 1">Sagman D, Tohen M. Comorbidity in bipolar disorder the complexity of diagnosis and treatment. Psychiatric times 2009;26:4. http://www.psychiatrictimes.com/bipolar-disorder/content/article/10168/1391541?pageNumber=3 (accessed 17 March 2011).</ref>. | |||
* Anxiety | |||
*[[Attention Deficit Disorders|Attention-Deficit/Hyperactivity Disorder]] | |||
*[[Substance Use Disorder|Substance Abuse]] | |||
* Associated medical co-morbidities include but not limited to [[Cardiovascular Disease|cardiovascular disease]], [[Diabetes Mellitus Type 2|type two DM]], and [[Metabolic and Endocrine Disorders|endocrine]] disorders<ref name="PT 1" />. | |||
* | * Medical comorbidities are quite prevalent in patients with bipolar disorder because of the adverse effects of treatment with mood stabilizers, anticonvulsants, antipsychotics, genetic vulnerability, and lifestyle factors (poor diet, lack of [[Therapeutic Exercise|exercise,]] [[Alcoholism|alcohol]] use, [[Smoking Cessation and Brief Intervention|smoking]]).<ref name=":1" /> | ||
Quick Facts: | |||
1.35% of people with bipolar disorder are [[Obesity|obese]]. This is the highest percentage for any psychiatric illness<ref name="BL 1" />. | |||
2. People with bipolar disorder are 3 times more likely to develop [[Diabetes Mellitus Type 2|diabetes]] than are members of the general population<ref name="BL 1" />. | |||
3. People with bipolar disorder are 1.5 - 2 times more likely to die from conditions such as [[Coronary Artery Disease (CAD)|heart disease]], diabetes and [[stroke]]<ref name="BL 1" />.<br> | |||
== Treatment == | |||
Medication assists to stabilise moods, and is the first-line treatment for acute episodes and to prevent relapses. But it’s now known that best practice treatment for bipolar disorder involves a combination of medication and psychotherapy. | |||
< | * In acute management, the primary goals are to ensure the safety of patients and nearby people, achieve clinical and functional stabilization with the least possible adverse effects. Additionally, engagement in treatment and development of a therapeutic alliance is important in any chronic disorder that requires long-term adherence, and this collaboration is especially true during the first episode.<ref name=":1" /> | ||
* Effective psychological treatments assist by providing information about the condition and risk factors and helping people identify and monitor triggers, manage stress, stabilise daily rhythms, adhere to medication, critique unhelpful thoughts and beliefs, and address substance use. | |||
* [[Electroconvulsive Therapy|Electroconvulsive therapy]] is extremely effective for treatment-resistant acute mood episodes like refractory depression or acute life-threatening mania, predominantly in patients with psychotic or catatonic features, and it is the best treatment for mania in a pregnant female.<ref name=":1" /> | |||
* Unfortunately, anecdotal data suggests many people never see a psychologist and, therefore, don’t receive the ongoing care that would help them to live well with bipolar disorder.<ref name=":0" /> | |||
* With the right assistance, the condition can be managed - a major longitudinal study found that approximately 50% of patients did not suffer significant ongoing difficulties with their symptoms. Contemporary researchers are confident that this proportion will grow as treatments advance. | |||
* New frameworks for examining bipolar disorder that focus on patient empowerment and collaboration among health professionals, researchers, families and consumers are also having positive effects<ref name=":0" /> | |||
== Diagnosis == | |||
= | There are no diagnostic tests, imaging studies or lab values that are able to accurately diagnose bipolar disorder. The correct diagnosis of bipolar affective disorder is facilitated, to a large degree, by a general clinical psychiatric assessment with the patient and their relatives, to recognize the longitudinal course of the disorder.<ref name=":1" /> | ||
== Physical Therapy Management == | |||
Patients with bipolar disorder are primarily treated by physicians, who prescribe medications, and psychologists. Both of these types of treatment methods are outside of the physical therapist's scope of practice. So ideally there is not much physical therapy management that goes into treating these patients. However, physical therapists may assist these patients with the various complications of the disorder. Since these patients are at a higher risk of suffering from obesity, diabetes mellitus, heart disease and stroke, physical therapists may play a significant role in helping these patients manage these conditions. Physical therapists can provide these patients with education and various exercise programs to assist them in achieving optimum quality of life. | |||
Physiotherapists can also help these patients with respiratory complications such as sleep apnea and respiratory muscle weakness. By providing breathing exercises and techniques, physiotherapists can improve the patient's lung function and overall respiratory health | |||
In addition, physiotherapists can also help these patients improve their mobility and prevent falls, which are common among individuals with these conditions. By working closely with other healthcare professionals, physical therapists can provide comprehensive care to these patients and improve their overall health outcomes. | |||
== Differential Diagnosis == | |||
== Differential Diagnosis | |||
Bipolar disorder may present with similar symptoms of other disorders such as: | Bipolar disorder may present with similar symptoms of other disorders such as: | ||
| Line 131: | Line 81: | ||
*Cyclothymic disorder | *Cyclothymic disorder | ||
*Schizoaffective disorder | *Schizoaffective disorder | ||
*Schizophrenia | *[[Schizophrenia]] | ||
*Delusional disorder | *Delusional disorder<ref name="BDT">Bipolar Disorder Today. Bipolar disorder. http://www.mental-health-today.com/bp/bi1.htm (accessed 5 April 2011).</ref> | ||
== References == | == References == | ||
<references /> | |||
[[Category:Bellarmine_Student_Project]] | |||
[[Category:Conditions]] | |||
[[Category:Mental_Health]] | |||
[[Category:Mental Health - Conditions]] | |||
[[Category:Head]] | |||
[[Category:Head - Conditions]] | |||
[[Category: | [[Category:Non Communicable Diseases]] | ||
Latest revision as of 17:06, 2 April 2023
Original Editors - Michael Thompson as part of the from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Michael Thompson, Admin, Elaine Lonnemann, Laura Ritchie, Lucinda hampton, Kim Jackson, WikiSysop, Simisola Ajeyalemi, Wendy Walker, Amanda Ager and Tolulope Adeniji
Introduction[edit | edit source]
Bipolar disorder, once known as manic depression, is a mood disorder experienced by between 1% and 6% of the population. It’s generally a lifelong condition, characterised by swings in mood: from highs that can tip into mania, to lows that can plunge into depression.
Historically, these moods have been the concern of psychiatrists and have therefore been framed in medical terms. Everyone experiences variations in mood, but for people with bipolar disorder these variations are extreme, and require psychiatric and psychological assistance.[1]
This one minute video is about Bipolar Disorder
Etiology[edit | edit source]
Like most psychiatric disorders, the causes of bipolar disorder are complex and multifactorial. Not surprisingly, there is strong familial transmission of the disorder, as the child is exposed to both genetic and environmental risk factors.
There is also a strong developmental trajectory in bipolar disorder, with early episodes of depression typically occurring in adolescence, followed by a defining manic episode in early adulthood.[1]
Epidemiolgy[edit | edit source]
The Depression and Bipolar Support Alliance has estimated that close to 6 million Americans are affected by bipolar disorder every year. Bipolar disorder can affect anyone at any age and is found in all races, ethnic groups and social classes with the typical onset being 25 years old. Patients may be diagnosed in their early childhood to as late as the 4th and 5th decades of life. Bipolar disorder is not gender-based and can affect men and women equally. Although, studies have shown that women with Bipolar disorder have more depressive and mixed episodes than men with the disorder. More than 66% of people diagnosed with Bipolar disorder have at least one primary family member with the illness[2].
The incidence of Bipolar disorder in other countries is notable as well. In Australia it is approximately 238,957 people, in the United Kingdom it is approximately 723,248 people, in Germany it is approximately 989,095 people, in Canada it is approximately 390,094 people, in Iran it is approximately 810,038 people and for both India and China it is approximately 12-15 million people[3].
Characteristics/Clinical Presentation[edit | edit source]
Note - patients can present in a mixed state which includes features from both 'poles' of BD.
- General Appearance: A patient with mania is often hyperkinetic, unpredictable, and erratic. They often are garishly dressed, display negligence of social propriety--demonstrable via excessive friendliness, boundary violations, agitation, or other improprieties--and appear to be unnaturally "happy" or euphoric, however, irritability is also observed, dispositionally.
- Mood and Affect: Mood is often elevated or euphoric, in mania. Affect is often heightened, intense, and extremely lability. Implicit with the affective lability of mania are hyperactivity and severe mobility. When presenting in a depressive state, the patient will report a sad or elegiac mood, while expressing a congruent affect (often tearful).
- Speech: A manic patient will demonstrate pressured speech, which implies a rapid and continuous production of speech that is difficult to interrupt. Reciprocally, speech is slow and soft, in depression.
- Perception: Mood delusions may be present in either the depressed or manic phase (e.g. delusions of guilt during depressed phases or grandiose delusions of power and wealth during manic phases) A manic patient can also have mood-incongruent delusions.
- Thought Process and Content: Patients with mania demonstrate easy distractibility, lack of concentration, illogical condensations, delusions of grandiosity, and flight of ideas. A depressed patient usually has negative thoughts and negative ruminations.
- Sensorium and Cognition: Usually oriented to person, place, and time. Depressed patients may have some impairment in cognition and memory. Manic patients may have a grossly intact memory. Sometimes orientation is impaired and is called manic delirium.
- Impulse Control: Extremely depressed patients demonstrate lack of willpower. Manic patients are threatening and assaultive.
- Judgment and Insight: Impaired judgment is the distinctive feature of mania along with limited insight. Depressed patients often overemphasize their symptoms.
- Reliability: Manic patients are usually unreliable in the information they provide. Depressed patients overemphasize.[4]
Associated Co-morbidities[edit | edit source]
Co-morbidities range from mental health disease all the way to physical system disorders[5].
- Anxiety
- Attention-Deficit/Hyperactivity Disorder
- Substance Abuse
- Associated medical co-morbidities include but not limited to cardiovascular disease, type two DM, and endocrine disorders[5].
- Medical comorbidities are quite prevalent in patients with bipolar disorder because of the adverse effects of treatment with mood stabilizers, anticonvulsants, antipsychotics, genetic vulnerability, and lifestyle factors (poor diet, lack of exercise, alcohol use, smoking).[4]
Quick Facts:
1.35% of people with bipolar disorder are obese. This is the highest percentage for any psychiatric illness[3].
2. People with bipolar disorder are 3 times more likely to develop diabetes than are members of the general population[3].
3. People with bipolar disorder are 1.5 - 2 times more likely to die from conditions such as heart disease, diabetes and stroke[3].
Treatment[edit | edit source]
Medication assists to stabilise moods, and is the first-line treatment for acute episodes and to prevent relapses. But it’s now known that best practice treatment for bipolar disorder involves a combination of medication and psychotherapy.
- In acute management, the primary goals are to ensure the safety of patients and nearby people, achieve clinical and functional stabilization with the least possible adverse effects. Additionally, engagement in treatment and development of a therapeutic alliance is important in any chronic disorder that requires long-term adherence, and this collaboration is especially true during the first episode.[4]
- Effective psychological treatments assist by providing information about the condition and risk factors and helping people identify and monitor triggers, manage stress, stabilise daily rhythms, adhere to medication, critique unhelpful thoughts and beliefs, and address substance use.
- Electroconvulsive therapy is extremely effective for treatment-resistant acute mood episodes like refractory depression or acute life-threatening mania, predominantly in patients with psychotic or catatonic features, and it is the best treatment for mania in a pregnant female.[4]
- Unfortunately, anecdotal data suggests many people never see a psychologist and, therefore, don’t receive the ongoing care that would help them to live well with bipolar disorder.[1]
- With the right assistance, the condition can be managed - a major longitudinal study found that approximately 50% of patients did not suffer significant ongoing difficulties with their symptoms. Contemporary researchers are confident that this proportion will grow as treatments advance.
- New frameworks for examining bipolar disorder that focus on patient empowerment and collaboration among health professionals, researchers, families and consumers are also having positive effects[1]
Diagnosis[edit | edit source]
There are no diagnostic tests, imaging studies or lab values that are able to accurately diagnose bipolar disorder. The correct diagnosis of bipolar affective disorder is facilitated, to a large degree, by a general clinical psychiatric assessment with the patient and their relatives, to recognize the longitudinal course of the disorder.[4]
Physical Therapy Management[edit | edit source]
Patients with bipolar disorder are primarily treated by physicians, who prescribe medications, and psychologists. Both of these types of treatment methods are outside of the physical therapist's scope of practice. So ideally there is not much physical therapy management that goes into treating these patients. However, physical therapists may assist these patients with the various complications of the disorder. Since these patients are at a higher risk of suffering from obesity, diabetes mellitus, heart disease and stroke, physical therapists may play a significant role in helping these patients manage these conditions. Physical therapists can provide these patients with education and various exercise programs to assist them in achieving optimum quality of life.
Physiotherapists can also help these patients with respiratory complications such as sleep apnea and respiratory muscle weakness. By providing breathing exercises and techniques, physiotherapists can improve the patient's lung function and overall respiratory health
In addition, physiotherapists can also help these patients improve their mobility and prevent falls, which are common among individuals with these conditions. By working closely with other healthcare professionals, physical therapists can provide comprehensive care to these patients and improve their overall health outcomes.
Differential Diagnosis[edit | edit source]
Bipolar disorder may present with similar symptoms of other disorders such as:
- Cyclothymic disorder
- Schizoaffective disorder
- Schizophrenia
- Delusional disorder[6]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 The Conversation Explainer: what is bipolar disorder? Available:https://theconversation.com/explainer-what-is-bipolar-disorder-7502 (accessed 4.9.2021)
- ↑ Depression and Bipolar Support Alliance. Bipolar disorder statistics. http://www.dbsalliance.org/site/PageServer?pagename=about_statistics_bipolar (accessed 17 March 2011).
- ↑ 3.0 3.1 3.2 3.3 Bipolar-Lives. Bipolar disorder statistics. http://www.bipolar-lives.com/bipolar-disorder-statistics.html (accessed 17 March 2011).
- ↑ 4.0 4.1 4.2 4.3 4.4 Jain A, Mitra P. Bipolar affective disorder. StatPearls [Internet]. 2021 May 18.Available:https://www.ncbi.nlm.nih.gov/books/NBK558998/ (accessed 4.9.2021)
- ↑ 5.0 5.1 Sagman D, Tohen M. Comorbidity in bipolar disorder the complexity of diagnosis and treatment. Psychiatric times 2009;26:4. http://www.psychiatrictimes.com/bipolar-disorder/content/article/10168/1391541?pageNumber=3 (accessed 17 March 2011).
- ↑ Bipolar Disorder Today. Bipolar disorder. http://www.mental-health-today.com/bp/bi1.htm (accessed 5 April 2011).