Avascular Necrosis Femoral Head: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (37 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class=" | <div class="noeditbox"> This article is currently under review and may not be up to date. Please come back soon to see the finished work! ({{REVISIONDAY}}/{{REVISIONMONTH}}/{{REVISIONYEAR}}) </div> | ||
<div class="editorbox"> | |||
'''Original Editor '''[[User:Anouk Toye|Anouk Toye]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
== Introduction == | |||
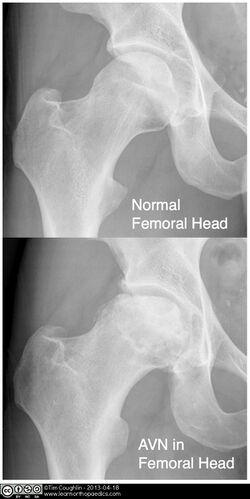
[[File:Hip Avascular Necrosis.jpeg|right|frameless|alt=|500x500px]] | |||
[[Avascular Necrosis|Avascular necrosis]] (AN) of the [[Femur|femoral]] head is a pathologic process that results from interruption of [[Blood Physiology|blood]] supply to the [[bone]]. Femoral head ischaemia causes bone marrow and osteocytic death, leading to collapse of the necrotic segment of the head of femur.. | |||
AN of the femoral head has often been described as a multifactorial disease. Etiopathogenesis is not well understood Risk Factors include: | |||
[[ | *[[Genetics and Health|Genetic predilection]]<ref>Adesina O, Brunson A, Keegan THM, Wun T. Osteonecrosis of the femoral head in sickle cell disease: prevalence, comorbidities, and surgical outcomes in California. Blood Adv. 2017;1(16):1287-1295.</ref> | ||
*[[Corticosteroid Medication|Corticosteroid]] intake<ref>Xie XH, Wang XL, Yang HL, Zhao DW, Qin L. Steroid-associated osteonecrosis: Epidemiology, pathophysiology, animal model, prevention, and potential treatments (an overview). J Orthop Translat. 2015 Apr;3(2):58-70. </ref> | |||
*[[Alcoholism|Alcohol]] | |||
* Smoking | |||
* Various [[Chronic Disease|chronic diseases]] <ref>Jaffré C, Rochefort GY. Alcohol-induced osteonecrosis--dose and duration effects. Int J Exp Pathol. 2012;93(1):78-9 | |||
</ref> eg [[Sickle Cell Anemia|sickle cell disease]], [[Human Immunodeficiency Virus (HIV)|human immunodeficiency virus]] , hypercoagulable states, [[Autoimmune Disorders|autoimmune disorder]]<nowiki/>s<ref name=":0">Orthobullets Hip Osteonecrosis Available: https://www.orthobullets.com/recon/5006/hip-osteonecrosis<nowiki/>(accessed 15.12.2022)</ref><ref name="Mont">Mont MA, Jones LC, Hungerford DS. Non-traumatic avascular necrosis of the femoral head: ten years later. J Bone Joint Surg Am. 2006;88:1117-1132</ref>. | |||
| |||
== Stages == | |||
AN progresses through four stages: | |||
# Initial/necrosis:blood supply gets disrupted, and necrosis begins | |||
# Fragmentation: the body resorbs the necrotic bone and replaces it with woven bone that is weak and vulnerable to breaking and collapse | |||
# Reossification: stronger bone develops | |||
# Healed/Remodeling: bone regrowth is complete, and final shape present (depending on damage may be normal or abnormal).<ref name=":1" /> | |||
It is very important that avascular necrosis is diagnosed early in the disease process | == Diagnostic procedures == | ||
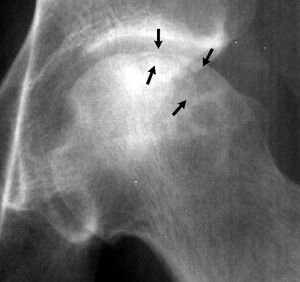
[[File:Crescent sign avascular necrosis.jpeg|thumb|Crescent sign]] | |||
It is very important that avascular necrosis is diagnosed early in the disease process as the success of the treatment relates to the stage at which the treatment starts. | |||
== | * Diagnosis be made with [[X-Rays|plain radiographs]] in moderate/late disease but [[MRI Scans|MRI]] may be required to detect early or subclinical osteonecrosis.<ref name=":0" /><ref name="Mont" /> | ||
* Crescent Sign: On Xray, a thin, curvilinear lucent line parallel to the [[Bone Cortical And Cancellous|cortical]] margin of the femoral head, in a patient with AN. | |||
== History and Physical Examination == | |||
= | Patients are often seen because of pain in the groin, but symptoms can also radiate to the [[knee]] or buttocks. On examination, there is usually a painful [[Range of Motion|range of motion]], especially on forced internal rotation<ref name="MA">Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995; 77:459-474</ref>. It is also important to track any risk factors before the start of the examination. Investigators need to be wary of avascular necrosis in any patient who has pain in the [[Hip Anatomy|hip]], negative radiographic findings, and any of the risk factors, described above. The other hip must also be evaluated. | ||
== Management == | |||
[[Image:Head of femur avascular necrosis.jpg|thumb|alt=|Head of femur avascular necrosis]]The precise therapy used depends on many factors, with each patient being evaluated individually for best outcomes. Such factors include the age of the patient, level of pain/discomfort, location and extent of necrosis and comorbidities. Treatments are best implemented at the pre-collapse stage and include both operatives as well as non-operatives options. If left untreated, femoral head AN may lead to subchondral fractures within only 2 to 3 years. The management ranges from conservative to invasive. Conservative management includes physical therapy, restricted weight-bearing, alcohol cessation, discontinuation of steroid therapy, pain control medication, and targeted pharmacologic therapy, among others. | |||
Generally, | |||
= | * Non-operative treatments or core decompression are best for asymptomatic and symptomatic small to medium-sized pre-collapse lesions. Conservative managements are physical therapy, restricted weight-bearing, alcohol cessation, discontinuation of steroid therapy, pain control medication, and targeted pharmacologic therapy, among others. | ||
* Medium to larger-sized lesions can have treatment with bone grafting (vascularized or non-vascularized), or osteotomies. | |||
* If femoral collapse has occurred or acetabular involvement is present, arthroplasty is indicated.<ref name=":1">Hsu H, Nallamothu SV. StatPearls. StatPearls Publishing; Treasure Island (FL), 2020. Hip Osteonecrosis. Available from:https://www.ncbi.nlm.nih.gov/books/NBK499954/ (Accessed 25 July 2020)</ref><ref>Barney J, Piuzzi NS, Akhondi H. Femoral head avascular necrosis.Available:https://www.ncbi.nlm.nih.gov/books/NBK546658/ (accessed 15.12.2022) </ref> | |||
Core decompression is a surgical procedure that requires surgical drilling into the area of dead bone near the joint, reducing pressure, allows for increased blood flow. This aims to slows or stops bone and/or joint destruction.<ref>Standford medicine Core decompression Available: https://stanfordhealthcare.org/medical-conditions/bones-joints-and-muscles/avascular-necrosis/treatments/core-decompression.html (accessed 15.12.2022)</ref> | |||
=== Physical therapy === | |||
Conservative management such as physiotherapy is needed to avoid further deterioration of the affected hip. However, while it has been shown to delay the disease progressing, physiotherapy alone cannot cure the process with most clients requiring surgical treatment. | |||
Physiotherapy treatment aims include: | |||
# Decreasing weight bearing: usually achieved with use of crutches or a walking aid. By using crutches, the load that the hip joint bears, will be decreased. This weight-bearing restriction is an important conservative treatment. | |||
# Education: On prevention, removal or reduction of risk factors such as smoking, alcohol abuse, obesity and corticosteroids | |||
# Range Of Motion: Both passive and active exercises should be initiated. Passive exercises contain passive movements of the hip and stretching exercises. Active exercises consist of 3 dimensional motions of the hip joint and can be applied during standing, sitting on a chair or while lying down. | |||
# Strengthening exercises: In the next stage, strengthening exercises are added, focusing on the muscles of the hip and thigh. Also include exercises for the core area as they play a large supporting role. To improve functionality it is important to implement endurance training and coordination training in a more advanced stage of the therapy. Endurance can be trained by walking on a treadmill or cycling on a home trainer. To improve coordination, walking exercises with increased complexity and balancing exercises can be adopted in physical therapy sessions. | |||
Physical therapy after surgery is also a key component for recovery. It starts immediately the day after surgery. Prepare the patients for discharge by showing them how to do their everyday activities like getting in and out of bed and walking with a walker or crutches. | |||
In a more advanced stage of the therapy, the therapist instructs the patient on exercises to strengthen their muscles, improve range of motion, work on balance and gait speed. The patient specifically learns how to move, while maintaining hip precautions. The rehabilitation protocol is combined with a home exercise program.<ref>Paula Miller, Treating Avascular Necrosis, 21(17):23</ref> | |||
[[Avascular Necrosis|See avascular necrosis page]]<br> | |||
== References == | |||
= References = | |||
<references /> | <references /> | ||
[[Category:Hip]] | |||
[[Category:Conditions]] | |||
[[Category:Hip - Conditions]] | |||
Latest revision as of 15:42, 15 December 2022
Original Editor Anouk Toye
Top Contributors - Lucinda hampton, Anouk Toye, Kim Jackson, Uchechukwu Chukwuemeka, Aarti Sareen, Admin and 127.0.0.1
Introduction[edit | edit source]
Avascular necrosis (AN) of the femoral head is a pathologic process that results from interruption of blood supply to the bone. Femoral head ischaemia causes bone marrow and osteocytic death, leading to collapse of the necrotic segment of the head of femur..
AN of the femoral head has often been described as a multifactorial disease. Etiopathogenesis is not well understood Risk Factors include:
- Genetic predilection[1]
- Corticosteroid intake[2]
- Alcohol
- Smoking
- Various chronic diseases [3] eg sickle cell disease, human immunodeficiency virus , hypercoagulable states, autoimmune disorders[4][5].
Stages[edit | edit source]
AN progresses through four stages:
- Initial/necrosis:blood supply gets disrupted, and necrosis begins
- Fragmentation: the body resorbs the necrotic bone and replaces it with woven bone that is weak and vulnerable to breaking and collapse
- Reossification: stronger bone develops
- Healed/Remodeling: bone regrowth is complete, and final shape present (depending on damage may be normal or abnormal).[6]
Diagnostic procedures[edit | edit source]
It is very important that avascular necrosis is diagnosed early in the disease process as the success of the treatment relates to the stage at which the treatment starts.
- Diagnosis be made with plain radiographs in moderate/late disease but MRI may be required to detect early or subclinical osteonecrosis.[4][5]
- Crescent Sign: On Xray, a thin, curvilinear lucent line parallel to the cortical margin of the femoral head, in a patient with AN.
History and Physical Examination[edit | edit source]
Patients are often seen because of pain in the groin, but symptoms can also radiate to the knee or buttocks. On examination, there is usually a painful range of motion, especially on forced internal rotation[7]. It is also important to track any risk factors before the start of the examination. Investigators need to be wary of avascular necrosis in any patient who has pain in the hip, negative radiographic findings, and any of the risk factors, described above. The other hip must also be evaluated.
Management[edit | edit source]
The precise therapy used depends on many factors, with each patient being evaluated individually for best outcomes. Such factors include the age of the patient, level of pain/discomfort, location and extent of necrosis and comorbidities. Treatments are best implemented at the pre-collapse stage and include both operatives as well as non-operatives options. If left untreated, femoral head AN may lead to subchondral fractures within only 2 to 3 years. The management ranges from conservative to invasive. Conservative management includes physical therapy, restricted weight-bearing, alcohol cessation, discontinuation of steroid therapy, pain control medication, and targeted pharmacologic therapy, among others.
Generally,
- Non-operative treatments or core decompression are best for asymptomatic and symptomatic small to medium-sized pre-collapse lesions. Conservative managements are physical therapy, restricted weight-bearing, alcohol cessation, discontinuation of steroid therapy, pain control medication, and targeted pharmacologic therapy, among others.
- Medium to larger-sized lesions can have treatment with bone grafting (vascularized or non-vascularized), or osteotomies.
- If femoral collapse has occurred or acetabular involvement is present, arthroplasty is indicated.[6][8]
Core decompression is a surgical procedure that requires surgical drilling into the area of dead bone near the joint, reducing pressure, allows for increased blood flow. This aims to slows or stops bone and/or joint destruction.[9]
Physical therapy[edit | edit source]
Conservative management such as physiotherapy is needed to avoid further deterioration of the affected hip. However, while it has been shown to delay the disease progressing, physiotherapy alone cannot cure the process with most clients requiring surgical treatment.
Physiotherapy treatment aims include:
- Decreasing weight bearing: usually achieved with use of crutches or a walking aid. By using crutches, the load that the hip joint bears, will be decreased. This weight-bearing restriction is an important conservative treatment.
- Education: On prevention, removal or reduction of risk factors such as smoking, alcohol abuse, obesity and corticosteroids
- Range Of Motion: Both passive and active exercises should be initiated. Passive exercises contain passive movements of the hip and stretching exercises. Active exercises consist of 3 dimensional motions of the hip joint and can be applied during standing, sitting on a chair or while lying down.
- Strengthening exercises: In the next stage, strengthening exercises are added, focusing on the muscles of the hip and thigh. Also include exercises for the core area as they play a large supporting role. To improve functionality it is important to implement endurance training and coordination training in a more advanced stage of the therapy. Endurance can be trained by walking on a treadmill or cycling on a home trainer. To improve coordination, walking exercises with increased complexity and balancing exercises can be adopted in physical therapy sessions.
Physical therapy after surgery is also a key component for recovery. It starts immediately the day after surgery. Prepare the patients for discharge by showing them how to do their everyday activities like getting in and out of bed and walking with a walker or crutches.
In a more advanced stage of the therapy, the therapist instructs the patient on exercises to strengthen their muscles, improve range of motion, work on balance and gait speed. The patient specifically learns how to move, while maintaining hip precautions. The rehabilitation protocol is combined with a home exercise program.[10]
References[edit | edit source]
- ↑ Adesina O, Brunson A, Keegan THM, Wun T. Osteonecrosis of the femoral head in sickle cell disease: prevalence, comorbidities, and surgical outcomes in California. Blood Adv. 2017;1(16):1287-1295.
- ↑ Xie XH, Wang XL, Yang HL, Zhao DW, Qin L. Steroid-associated osteonecrosis: Epidemiology, pathophysiology, animal model, prevention, and potential treatments (an overview). J Orthop Translat. 2015 Apr;3(2):58-70.
- ↑ Jaffré C, Rochefort GY. Alcohol-induced osteonecrosis--dose and duration effects. Int J Exp Pathol. 2012;93(1):78-9
- ↑ 4.0 4.1 Orthobullets Hip Osteonecrosis Available: https://www.orthobullets.com/recon/5006/hip-osteonecrosis(accessed 15.12.2022)
- ↑ 5.0 5.1 Mont MA, Jones LC, Hungerford DS. Non-traumatic avascular necrosis of the femoral head: ten years later. J Bone Joint Surg Am. 2006;88:1117-1132
- ↑ 6.0 6.1 Hsu H, Nallamothu SV. StatPearls. StatPearls Publishing; Treasure Island (FL), 2020. Hip Osteonecrosis. Available from:https://www.ncbi.nlm.nih.gov/books/NBK499954/ (Accessed 25 July 2020)
- ↑ Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995; 77:459-474
- ↑ Barney J, Piuzzi NS, Akhondi H. Femoral head avascular necrosis.Available:https://www.ncbi.nlm.nih.gov/books/NBK546658/ (accessed 15.12.2022)
- ↑ Standford medicine Core decompression Available: https://stanfordhealthcare.org/medical-conditions/bones-joints-and-muscles/avascular-necrosis/treatments/core-decompression.html (accessed 15.12.2022)
- ↑ Paula Miller, Treating Avascular Necrosis, 21(17):23