Rehabilitation of Burns in Disasters and Conflicts: Difference between revisions
No edit summary |
m (Protected "Rehabilitation of Burns in Disasters and Conflicts" ([Edit=⧼protect-level-ppadmin⧽] (indefinite) [Move=⧼protect-level-ppadmin⧽] (indefinite))) |
||
| (39 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors ''' - | '''Original Editors ''' - [[User:Stacy Schiurring|Stacy Schiurring]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div | </div> | ||
== Introduction == | == Introduction == | ||
Burn injuries are complex and involved injuries | Burn injuries are complex and involved injuries that require immediate and specialised interventions. Burn injuries commonly require a prolonged rehabilitation process to return to functional independence, often with adaptation or compensatory training in the long term. These patients will require both physical and psychological support throughout their rehabilitation process. This is especially true when an injury occurs as a result of disaster or conflict.<ref name=":0">Lathia C, Skelton P, Clift Z. [https://hi.org/sn_uploads/document/36199-Humanity--Inclusion-Clinical-Handbook-web_1.pdf Early rehabilitation in conflicts and disasters.] Handicap International: London, UK. 2020.</ref> | ||
Acutely, rehabilitation will be supportive of the medical needs of the patient. | Acutely, rehabilitation will be supportive of the medical needs of the patient. However, rehabilitation plays an important role in the acute phase to prepare the patient both physically and mentally for the therapy to come. This article will focus on the physical rehabilitation of patients who have had a burn injury, but will include important wound care considerations with regards to mobility and positioning. | ||
<blockquote>Rehabilitation for burn injuries starts from day one of the injury, right through the period of scar maturation, and often for years after the injury, especially relevant to the prevention of contractures and in children where growth is not complete.<ref name=":0" /></blockquote> | <blockquote>Rehabilitation for burn injuries starts from day one of the injury, right through the period of scar maturation, and often for years after the injury, especially relevant to the prevention of contractures and in children where growth is not complete.<ref name=":0" /></blockquote> | ||
Please read the linked article for background knowledge of [[Wound Healing|wound healing]]. Understanding the expected timeline of wound healing and the body's response to injury is vital in patient education and differentiating normal wound healing from the signs and symptoms of infection. | == Burns Overview == | ||
Please read the linked article for background knowledge on the [[Skin|anatomy and physiology of the skin]]. Understanding the structure of the skin is an important part of burn classification. Please read the linked article for background knowledge of [[Wound Healing|wound healing]]. Understanding the expected timeline of wound healing and the body's response to injury is vital in patient education and differentiating normal wound healing from the signs and symptoms of infection. This article also contains links to [[Wound Assessment|wound assessment]] and [[Wound Debridement|wound debridement]] to better understand these procedures. Wound care is a specialised skill and should not be performed without the proper training. Physiotherapists can specialise in wound management with advanced training. | |||
=== Types of Burns === | === Types of Burns === | ||
Burn injuries have several common causes which include, but are not limited to: | |||
# '''Thermal burns:''' due to heat sources | # '''Thermal burns:''' They occur due to heat sources that raise the temperature of the skin and surrounding tissues. This causes tissue cell death or charring. Heat sources can include hot metals, scalding liquids, steam, and flames. Thermal burns can also be caused by exposure to extreme colds such as a frostbite injury. | ||
# '''Radiation burns:''' | # '''Radiation burns:''' Radiation burns occur due to prolonged exposure to ultraviolet rays or to other sources of radiation. Radiation sources can include the sun and X-rays. | ||
# '''Chemical burns:''' due to strong acids, alkalies, detergents, or solvents | # '''Chemical burns:''' These happen due to strong acids, alkalies, detergents, or solvents that come into contact with the skin. | ||
# '''Electrical burns:''' due to electrical current, either alternating current (AC) or direct current (DC) coming into contact with the body. <ref> | # '''Electrical burns:''' Electrical burns occur due to electrical current, either alternating current (AC) or direct current (DC) coming into contact with the body. These burns have increased potential for internal damage. | ||
<ref>Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. [https://www.nature.com/articles/s41572-020-0145-5#citeas Burn injury.] Nature Reviews Disease Primers. 2020 Feb 13;6(1):1-25.</ref> | |||
=== Classification of Burns === | === Classification of Burns === | ||
[[File:Burn Degree Diagram.svg.png|center|thumb|857x857px|Depth of burn classification ]] | |||
{| | {| class="wikitable" | ||
|+ | |+ | ||
'''Table.1''' Depth of Burns Characteristics adapted from Lathia et al. 2020.<ref name=":0" /> | |||
!'''Depth of burn''' | !'''Depth of burn''' | ||
!'''Tissues destroyed''' | !'''Tissues destroyed''' | ||
!'''Burn Appearance''' | !'''Burn Appearance''' | ||
!'''Pain Sensitivity''' | !'''Pain Sensitivity''' | ||
!'''Healing Time and Prognosis''' | |||
|- | |- | ||
|Superficial | |'''Superficial''' | ||
i.e. 1st degree burn | i.e. 1st degree burn | ||
|Outer layer of epidermis | |Outer layer of epidermis | ||
| | | | ||
* | * Red | ||
* | * Blistering is uncommon | ||
* | * Slight oedema | ||
* Capillary refill: affected area blanches with pressure and refills (see video example below) | * Capillary refill: affected area blanches with pressure and refills (see video example below) | ||
|Painful | |Painful | ||
| | |||
* Less than 14 days | |||
* No long term scarring expected | |||
|- | |- | ||
|Superficial Partial Thickness (SPT) | |'''Superficial Partial Thickness (SPT)''' | ||
i.e. 2nd degree burn: superficial/intermediate | i.e. 2nd degree burn: superficial/intermediate | ||
| | | | ||
| Line 55: | Line 55: | ||
* Some hair follicles and sweat and sebaceous glands destroyed | * Some hair follicles and sweat and sebaceous glands destroyed | ||
| | | | ||
* | * Red | ||
* | * Blisters | ||
* | * Moist subcutaneous | ||
* | * Oedema | ||
* Capillary refill | * Capillary refill | ||
|Very painful and hypersensitive | |Very painful and hypersensitive | ||
| | |||
* 7 - 20 days | |||
* May scar in rare cases | |||
* Pigment changes | |||
|- | |- | ||
|Deep Partial Thickness (DPT) | |'''Deep Partial Thickness (DPT)''' | ||
i.e. 2nd degree burn: deep | i.e. 2nd degree burn: deep | ||
| | | | ||
| Line 69: | Line 73: | ||
| | | | ||
* Variable in colour (mottled) | * Variable in colour (mottled) | ||
* | * Wet or waxy dry | ||
* Generally blisters | * Generally blisters | ||
* No or slow capillary refill | * No or slow capillary refill | ||
* Eschar forms | * Eschar forms | ||
|Less sensitive to pain due to destroyed nerve endings | |Less sensitive to pain due to destroyed nerve endings | ||
| | |||
* At least 21 days healing time but difficult to determine | |||
* Scarring | |||
* Risk of contractures | |||
* May require grafting | |||
|- | |- | ||
|Full Thickness Burn (FTB) | |'''Full Thickness Burn (FTB)''' | ||
i.e. 3rd degree burn | i.e. 3rd degree burn | ||
|All skin layers damaged or destroyed; fat or bone may be visible. | |All skin layers damaged or destroyed; fat or bone may be visible. | ||
| Line 82: | Line 91: | ||
* No blisters | * No blisters | ||
|No pain from lost cutaneous pain receptors BUT situation is often painful for the patient. | |No pain from lost cutaneous pain receptors BUT situation is often painful for the patient. | ||
| | |||
* Severe scarring | |||
* Risk of contractures | |||
* No skin regeneration | |||
* Need excision and grafting | |||
* Prolonged hospitalisation | |||
|} | |} | ||
Below is a video which goes into greater detail on burn classification and staging. It also includes examples of the burn's appearance. | |||
{{#ev:youtube| vCzPNl8EvHM |500}}<ref>YouTube. Burns: Clinical Estimation – Emergency Medicine | Lecturio. Available from: https://www.youtube.com/watch?v=vCzPNl8EvHM [last accessed 03/03/2022]</ref> | |||
Next is a video of the capillary refill test being performed on a healthy finger. Note the blanching of the skin when pressure is removed and how long it takes for the colour to return. The '''[[Capillary Refill Test]] (CRT)''' is a rapid test used for assessing the blood flow through peripheral tissues. It is a quick test performed on the nail beds to monitor the amount of blood flow to tissues and [[dehydration]].<ref>Capillary nail refill test. Available from: https://medlineplus.gov/ency/article/003394.htm (Accessed 24 October 2020)</ref> The CRT measures the efficacity of the vascular system of hands and feet as they are far from the heart.<ref>Capillary nail refill test. Available from: http://pennstatehershey.adam.com/content.aspx?productid=117&pid=1&gid=003394 (last Accessed 25 October 2020</ref> | |||
{{#ev:youtube|n--wFoZFklg|500}}<ref>YouTube. Capillary Refill Test. Available from: https://www.youtube.com/watch?v=n--wFoZFklg [last accessed 02/03/2022]</ref> | |||
=== Burn Assessment === | |||
'''Total Body Surface Area''' (TBSA) burned: the area of the body that is affected by a burn. This is expressed in a percentage, for example if a chart reads 20% TBSA burn, this would mean 20% of the total surface area of that patient was affected by a burn. | |||
* Different forms are used for adults and children | |||
* For adults, a major burn involves 30% TBSA or more, children 20% TBSA or more. | |||
* Location and type of burn also influence the severity and have functional implications. For example: deep burns on the hands record as a small TBSA but have a huge functional impact for that patient. | |||
<br> | |||
The two most common recording methods of TBSA are the '''Rule of Nines''' and '''Lund and Browder'''.<ref name=":0" /> Examples of these two methods are shown below as reference.[[File:Rule of nines and Lund Browder chart.png|center|thumb|500x500px|Example of Rule of Nines and Lund-Browder Assessments]] | |||
== Immediate Medical Care Needs == | == Immediate Medical Care Needs == | ||
In the acute care phase of major burns injuries, medical management will include: | In the acute care phase of major burns injuries, medical management will include: | ||
# Fluid resuscitation<ref name=":0" /> | |||
# Fluid resuscitation | # Airway management<ref name=":0" /><ref name=":1">Legrand M, Barraud D, Constant I, Devauchelle P, Donat N, Fontaine M, Goffinet L, Hoffmann C, Jeanne M, Jonqueres J, Leclerc T. [https://www.sciencedirect.com/science/article/pii/S2352556820300382 Management of severe thermal burns in the acute phase in adults and children]. Anaesthesia Critical Care & Pain Medicine. 2020 Apr 1;39(2):253-67.</ref> | ||
# Airway management | |||
# Wound debridement and or surgical procedures such as escharotomy or fasciotomy<ref name=":0" /> | # Wound debridement and or surgical procedures such as escharotomy or fasciotomy<ref name=":0" /> | ||
# Pain management<ref name=":1" /> | |||
== Rehabilitation | == Acute Rehabilitation for Burn Injury == | ||
=== Acute Burn Injury Mobility Precautions === | === Acute Burn Injury Mobility Precautions === | ||
* Burns encountered in conflict zones or disaster areas are often combined with trauma injuries such as fractures<ref name=":0" />, internal injuries, or brain and or head injuries. Appropriate mobility precautions such as extremity weightbearing status, spinal and or cervical immobilisation, or bedrest needs in the case of internal organ injuries or bleeding need to be determined with the medical team. | |||
* Burns encountered in conflict zones or disaster areas are often combined with trauma injuries such as fractures<ref name=":0" />, internal injuries, or brain and or head injuries. | * If shrapnel is present in the burn/wound and cannot be easily removed due to the risk of further tissue damage, it may be left in place.<ref name=":0" /> Defer to the medical team regarding mobilisation of the affected area in these cases. | ||
* If shrapnel is present in the burn/wound | * Pain will develop following surgical debridements<ref name=":0" />, plan accordingly with the pain medication schedule. | ||
* Pain will develop following surgical debridements<ref name=":0" />, plan accordingly with pain medication schedule. | |||
* | * | ||
=== Acute Rehabilitation === | === Acute Rehabilitation === | ||
Rehabilitation should begin as soon as the patient is medically stable. Research has found that early initiation of limb positioning, mobilisation and splint use has a positive outcome in subsequent development of contractures in patients with burns.<ref>Puri V, Shrotriya R, Bachhav M. [https://www.bachhavcosmeticsurgery.com/wp-content/uploads/2019/03/pbc.who-will-bell-the-cat.pdf The scourge of burn contractures: Who will bell the cat?]. Burns. 2019 Jun 1;45(4):791-7.</ref> <blockquote>'''Acute rehabilitation for burn injury focuses on:''' | |||
# Respiratory Care | |||
# Oedema Management | |||
# Positioning, Splinting and Pressure Relief | |||
# Early Mobility | |||
# Progressive Graded Exercises | |||
# Maintaining Functional Independence | |||
# Patient and Caregiver Education<ref name=":0" /> | |||
</blockquote> | |||
==== Respiratory Care ==== | |||
The aims of physiotherapy for respiratory care involve: airway maintenance, secretion removal, gas exchange improvement, prevention and or treatment of [[atelectasis]], and maintenance of thoracic expansion.<ref name=":0" /> | |||
For deeper knowledge on these topics, please read more about [[Inhalation Injury|inhalation injury]] and [[Respiratory Physiotherapy|chest physiotherapy]]. | |||
==== Oedema Management ==== | |||
Oedema is a normal response to injury and an important step in wound healing. However, excessive oedema can negatively effect wound healing. | |||
'''Acute oedema management includes:''' | |||
* Appropriate extremity positioning | |||
* Use of muscle pump action through active AROM | |||
* Facial oedema requires a patient to sit up to at least 45 degrees 24 hours/day | |||
* Expect dressings used for oedema management to be firm but allowing for AROM of all joints | |||
==== Positioning, Splinting, Pressure Relief ==== | |||
<blockquote>Proper and correct positioning is essential for contracture prevention. Positioning for contracture prevention should be used prophylactically even when there is no sign of lost ROM upon initial assessment of affected area. Depending on the severity of the burn injury, splinting and positioning programmes may need to be continued for at least six months for optimal results.<ref name=":0" /></blockquote>Patients with burns will typically wish to go into a position of comfort, which is generally a [[Flexion deformity|flexion pattern]]. Developing scar tissue will result in shortened muscle lengths if patients are allows to maintain these positions over time. Scar tissue after a burn can develop as quickly as over a few hours. | |||
'''Anti-Deformity Positioning:''' | |||
*'''Shoulders''': abducted to 90 degrees, horizontally adducted to 20 degrees, encourage external rotation | |||
*'''Scapula''': retracted, depressed, supinated | |||
*'''Upper extremities''': neutral rotation, forearms supinated | |||
*'''Elbows''': extended | |||
*'''Wrist''': 30-40 degrees extension, MP 45-70 degrees flexion, IP extension, thumb abducted and opposed | |||
*'''Neck''': slightly extended, no pillow | |||
*'''Hips''': slight abduction with full extension, block external rotation<ref name=":0" /> | |||
[[File:Pressure sore.jpeg|thumb|400x400px|Bony landmarks and potential courses of pressure]] | |||
<br>Patients with burns are at high risk of further skin breakdown at areas of increased pressure. Offload and provide appropriate pressure relief as needed. This is especially true following a skin graft or surgical flap. No pressure can be placed over an area following a skin graft or flap as occlusion in blood flow will make the new tissue nonviable.<br> | |||
<br>'''Splinting''' is typically indicated: | |||
* To position extremities for contracture prevention | |||
* To protect grafts or surgical flaps during the initial phase of healing | |||
<br>According to a 2020 systematic review, "orthotic use should be considered as a treatment choice for improving ROM or reducing contracture in adults who have sustained a burn injury." This study also found that patients who used splints or orthotics had a lower incident for the need of reconstructive surgery later in their healing process and provided positive skin graft outcomes with appropriate orthotic use.<ref name=":2">Parry IS, Schneider JC, Yelvington M, Sharp P, Serghiou M, Ryan CM, Richardson E, Pontius K, Niszczak J, McMahon M, MacDonald LE. [https://experts.nebraska.edu/en/publications/systematic-review-and-expert-consensus-on-the-use-of-orthoses-spl Systematic review and expert consensus on the use of orthoses (splints and casts) with adults and children after burn injury to determine practice guidelines.] Journal of Burn Care & Research. 2020 May 2;41(3):503-34.</ref> | |||
Splints or orthotics can be used on any part or joint of the body. They are most commonly used for positioning of the mouth (42%), then neck (12%), hands and axillae (10% each), ankle (8%), elbow (4%), and knee (2%). Unfortunately, there is no standardised wearing time or schedule for burn contracture management. Studies in non-burn-specific literature evaluating hand and finger contracture management using dynamic splinting recommend orthosis wear at end range of motion for greater than 6 hours per day, for a minimum of 12 weeks.<ref name=":2" /> | |||
Please read this article for more in-depth information on [[Splinting for Burns|splinting for burns]]. | |||
==== Early Mobility, Exercise, Functional Independence ==== | |||
The goal of early mobilisation and therapy interventions after a burn is to maintain functional mobility and endurance while the body heals. The degree of burn will dictate therapy intensity. The areas affected by the burn will require gentle ROM, which should be slow and smooth to decrease associated pain and inflammation with movement.<ref name=":0" /> | |||
Currently there is little research on early mobilisation following acute burns. A 2019 meta-analysis and systematic review of trauma patients in the ICU found that early mobilisation decreased time of mechanical ventilation, but had similar mortality and hospital length of stay compared to those patients that did not receive early mobility.<ref>Higgins SD, Erdogan M, Coles SJ, Green RS. [https://www.sciencedirect.com/science/article/abs/pii/S0020138319305248 Early mobilization of trauma patients admitted to intensive care units: a systematic review and meta-analyses.] Injury. 2019 Nov 1;50(11):1809-15.</ref> However a 2020 retrospective study of trauma patients in the ICU not only states that early mobility is a safe, feasible and effective strategy to improve functional outcomes, but also that patients who received early mobility were less likely to die in both the ICU and hospital.<ref>Coles SJ, Erdogan M, Higgins SD, Green RS. [https://journals.lww.com/jtrauma/Abstract/2020/04000/Impact_of_an_early_mobilization_protocol_on.7.aspx Impact of an early mobilization protocol on outcomes in trauma patients admitted to the intensive care unit: A retrospective pre-post study.] Journal of Trauma and Acute Care Surgery. 2020 Apr 1;88(4):515-21.</ref> Please read this article for more in-depth information on [[Early Mobilization in the ICU|early mobilisation of patients in the ICU]]. | |||
While further research is needed on the effectiveness and risks/benefits of early mobility of patients after burns, data from similar populations suggest the benefits may outweigh no mobility intervention. Please read this article for more in-depth information on [[Post-burn Rehabilitation|post-burn rehabilitation]]. | |||
=== | ==== Education ==== | ||
Due to the long healing and rehabilitation timeframe following a burn, patient and caregiver education is of vital importance for successful burn management and rehabilitation. | |||
== Treatment Red Flags == | This education and training should include: | ||
* ROM and stretching exercises with special consideration given to a patient's fear of movement due to pain | |||
* Contracture aetiology and prevention | |||
* Functional activities and mobility to include assistive device use | |||
* Positioning and pressure relief techniques | |||
* Splint use and wearing schedule | |||
* Infection control | |||
* Anticipated healing times as a patient moves from the acute phase into the subacute phase and beyond<ref name=":0" /> | |||
=== Treatment Red Flags === | |||
Rehabilitation therapists such as physiotherapists often have the most direct contact with their patients. Therefore, it is important to monitor these patients for treatment red flags and alert the medical team as appropriate. | |||
* Hypovolemic shock | |||
* Infection: this is the most common cause of death of patients with burns who survive the initial injury. | |||
*[[Compartment Syndrome|Compartment syndrome]] | |||
* Inadequate pain management<ref name=":0" /> | |||
<br>Familiarise yourself with the signs and symptoms of [[sepsis]]. | |||
== Resources == | == Resources == | ||
===Rehabilitation in Conflict and Disasters Field Support=== | |||
*[https://humanity-inclusion.org.uk/sn_uploads/uk/document/responding-disasters-dos-and-donts-guide-rehabilitation-professionals-april-2016.pdf Responding Internationally to Disasters: Do’s and Don’ts] | |||
*[https://hi.org/en/early-rehabilitation-in-conflicts-and-disasters Early Rehabilitation in Conflict and Disasters,] Humanity and Inclusion | |||
*[https://www.physio-pedia.com/images/a/ae/Chapter_8_Acquired_Brain_Injury.pdf Rehabilitation in Sudden Onset Disasters,] Humanity and Inclusion | |||
*[https://get.disasterready.org/rehabilitation-treatment-planning/ Rehabilitation Treatment Planning Tool for Common Conflict and Emergency Related Injuries] | |||
=== Burns Specific Support === | |||
* [https://worldburn.org International Society for Burn Injuries] | |||
*[http://brc.iaff.org/burn-foundations---partnerships.html Burn Foundations and Partnerships] | |||
*[https://ameriburn.org American Burn Association] | |||
=== Technical Standards for Medical Teams === | |||
*[https://www.who.int/publications/i/item/emergency-medical-teams Minimum Technical Standards and Recommendations for Rehabilitation in Emergency Medical Teams] | |||
*[https://www.jisprm.org/article.asp?issn=2349-7904;year=2018;volume=1;issue=2;spage=72;epage=94;aulast=Amatya Minimum Technical Standards and Recommendations for TBI Rehabilitation Teams in Sudden-onset Disasters] | |||
== References == | == References == | ||
<references /> | |||
[[Category:Rehabilitation in Disaster and Conflict Situations Content Development Project]] | |||
[[Category:Rehabilitation in Disaster and Conflict Situations]] | |||
[[Category:ReLAB-HS Course Page]] | |||
[[Category:Rehabilitation]] | |||
[[Category:Course Pages]] | |||
[[Category:Projects]] | |||
[[Category:Burns]] | |||
Latest revision as of 12:12, 25 November 2022
Original Editors - Stacy Schiurring
Top Contributors - Stacy Schiurring, Naomi O'Reilly, Rishika Babburu, Kim Jackson, Jess Bell, Chelsea Mclene and Carin Hunter
Introduction[edit | edit source]
Burn injuries are complex and involved injuries that require immediate and specialised interventions. Burn injuries commonly require a prolonged rehabilitation process to return to functional independence, often with adaptation or compensatory training in the long term. These patients will require both physical and psychological support throughout their rehabilitation process. This is especially true when an injury occurs as a result of disaster or conflict.[1]
Acutely, rehabilitation will be supportive of the medical needs of the patient. However, rehabilitation plays an important role in the acute phase to prepare the patient both physically and mentally for the therapy to come. This article will focus on the physical rehabilitation of patients who have had a burn injury, but will include important wound care considerations with regards to mobility and positioning.
Rehabilitation for burn injuries starts from day one of the injury, right through the period of scar maturation, and often for years after the injury, especially relevant to the prevention of contractures and in children where growth is not complete.[1]
Burns Overview[edit | edit source]
Please read the linked article for background knowledge on the anatomy and physiology of the skin. Understanding the structure of the skin is an important part of burn classification. Please read the linked article for background knowledge of wound healing. Understanding the expected timeline of wound healing and the body's response to injury is vital in patient education and differentiating normal wound healing from the signs and symptoms of infection. This article also contains links to wound assessment and wound debridement to better understand these procedures. Wound care is a specialised skill and should not be performed without the proper training. Physiotherapists can specialise in wound management with advanced training.
Types of Burns[edit | edit source]
Burn injuries have several common causes which include, but are not limited to:
- Thermal burns: They occur due to heat sources that raise the temperature of the skin and surrounding tissues. This causes tissue cell death or charring. Heat sources can include hot metals, scalding liquids, steam, and flames. Thermal burns can also be caused by exposure to extreme colds such as a frostbite injury.
- Radiation burns: Radiation burns occur due to prolonged exposure to ultraviolet rays or to other sources of radiation. Radiation sources can include the sun and X-rays.
- Chemical burns: These happen due to strong acids, alkalies, detergents, or solvents that come into contact with the skin.
- Electrical burns: Electrical burns occur due to electrical current, either alternating current (AC) or direct current (DC) coming into contact with the body. These burns have increased potential for internal damage.
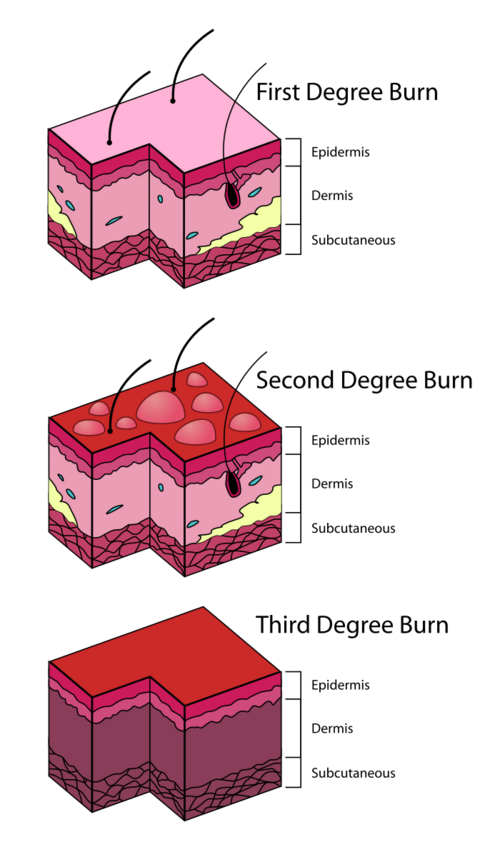
Classification of Burns[edit | edit source]
| Depth of burn | Tissues destroyed | Burn Appearance | Pain Sensitivity | Healing Time and Prognosis |
|---|---|---|---|---|
| Superficial
i.e. 1st degree burn |
Outer layer of epidermis |
|
Painful |
|
| Superficial Partial Thickness (SPT)
i.e. 2nd degree burn: superficial/intermediate |
|
|
Very painful and hypersensitive |
|
| Deep Partial Thickness (DPT)
i.e. 2nd degree burn: deep |
|
|
Less sensitive to pain due to destroyed nerve endings |
|
| Full Thickness Burn (FTB)
i.e. 3rd degree burn |
All skin layers damaged or destroyed; fat or bone may be visible. |
|
No pain from lost cutaneous pain receptors BUT situation is often painful for the patient. |
|
Below is a video which goes into greater detail on burn classification and staging. It also includes examples of the burn's appearance.
Next is a video of the capillary refill test being performed on a healthy finger. Note the blanching of the skin when pressure is removed and how long it takes for the colour to return. The Capillary Refill Test (CRT) is a rapid test used for assessing the blood flow through peripheral tissues. It is a quick test performed on the nail beds to monitor the amount of blood flow to tissues and dehydration.[4] The CRT measures the efficacity of the vascular system of hands and feet as they are far from the heart.[5]
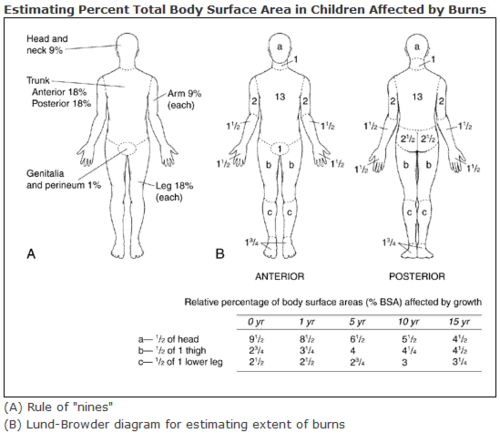
Burn Assessment[edit | edit source]
Total Body Surface Area (TBSA) burned: the area of the body that is affected by a burn. This is expressed in a percentage, for example if a chart reads 20% TBSA burn, this would mean 20% of the total surface area of that patient was affected by a burn.
- Different forms are used for adults and children
- For adults, a major burn involves 30% TBSA or more, children 20% TBSA or more.
- Location and type of burn also influence the severity and have functional implications. For example: deep burns on the hands record as a small TBSA but have a huge functional impact for that patient.
The two most common recording methods of TBSA are the Rule of Nines and Lund and Browder.[1] Examples of these two methods are shown below as reference.
Immediate Medical Care Needs[edit | edit source]
In the acute care phase of major burns injuries, medical management will include:
- Fluid resuscitation[1]
- Airway management[1][7]
- Wound debridement and or surgical procedures such as escharotomy or fasciotomy[1]
- Pain management[7]
Acute Rehabilitation for Burn Injury[edit | edit source]
Acute Burn Injury Mobility Precautions[edit | edit source]
- Burns encountered in conflict zones or disaster areas are often combined with trauma injuries such as fractures[1], internal injuries, or brain and or head injuries. Appropriate mobility precautions such as extremity weightbearing status, spinal and or cervical immobilisation, or bedrest needs in the case of internal organ injuries or bleeding need to be determined with the medical team.
- If shrapnel is present in the burn/wound and cannot be easily removed due to the risk of further tissue damage, it may be left in place.[1] Defer to the medical team regarding mobilisation of the affected area in these cases.
- Pain will develop following surgical debridements[1], plan accordingly with the pain medication schedule.
Acute Rehabilitation[edit | edit source]
Rehabilitation should begin as soon as the patient is medically stable. Research has found that early initiation of limb positioning, mobilisation and splint use has a positive outcome in subsequent development of contractures in patients with burns.[8]
Acute rehabilitation for burn injury focuses on:
- Respiratory Care
- Oedema Management
- Positioning, Splinting and Pressure Relief
- Early Mobility
- Progressive Graded Exercises
- Maintaining Functional Independence
- Patient and Caregiver Education[1]
Respiratory Care[edit | edit source]
The aims of physiotherapy for respiratory care involve: airway maintenance, secretion removal, gas exchange improvement, prevention and or treatment of atelectasis, and maintenance of thoracic expansion.[1]
For deeper knowledge on these topics, please read more about inhalation injury and chest physiotherapy.
Oedema Management[edit | edit source]
Oedema is a normal response to injury and an important step in wound healing. However, excessive oedema can negatively effect wound healing.
Acute oedema management includes:
- Appropriate extremity positioning
- Use of muscle pump action through active AROM
- Facial oedema requires a patient to sit up to at least 45 degrees 24 hours/day
- Expect dressings used for oedema management to be firm but allowing for AROM of all joints
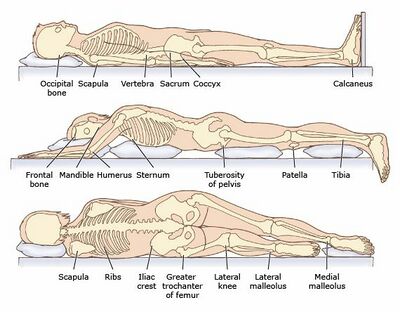
Positioning, Splinting, Pressure Relief[edit | edit source]
Proper and correct positioning is essential for contracture prevention. Positioning for contracture prevention should be used prophylactically even when there is no sign of lost ROM upon initial assessment of affected area. Depending on the severity of the burn injury, splinting and positioning programmes may need to be continued for at least six months for optimal results.[1]
Patients with burns will typically wish to go into a position of comfort, which is generally a flexion pattern. Developing scar tissue will result in shortened muscle lengths if patients are allows to maintain these positions over time. Scar tissue after a burn can develop as quickly as over a few hours.
Anti-Deformity Positioning:
- Shoulders: abducted to 90 degrees, horizontally adducted to 20 degrees, encourage external rotation
- Scapula: retracted, depressed, supinated
- Upper extremities: neutral rotation, forearms supinated
- Elbows: extended
- Wrist: 30-40 degrees extension, MP 45-70 degrees flexion, IP extension, thumb abducted and opposed
- Neck: slightly extended, no pillow
- Hips: slight abduction with full extension, block external rotation[1]
Patients with burns are at high risk of further skin breakdown at areas of increased pressure. Offload and provide appropriate pressure relief as needed. This is especially true following a skin graft or surgical flap. No pressure can be placed over an area following a skin graft or flap as occlusion in blood flow will make the new tissue nonviable.
Splinting is typically indicated:
- To position extremities for contracture prevention
- To protect grafts or surgical flaps during the initial phase of healing
According to a 2020 systematic review, "orthotic use should be considered as a treatment choice for improving ROM or reducing contracture in adults who have sustained a burn injury." This study also found that patients who used splints or orthotics had a lower incident for the need of reconstructive surgery later in their healing process and provided positive skin graft outcomes with appropriate orthotic use.[9]
Splints or orthotics can be used on any part or joint of the body. They are most commonly used for positioning of the mouth (42%), then neck (12%), hands and axillae (10% each), ankle (8%), elbow (4%), and knee (2%). Unfortunately, there is no standardised wearing time or schedule for burn contracture management. Studies in non-burn-specific literature evaluating hand and finger contracture management using dynamic splinting recommend orthosis wear at end range of motion for greater than 6 hours per day, for a minimum of 12 weeks.[9]
Please read this article for more in-depth information on splinting for burns.
Early Mobility, Exercise, Functional Independence[edit | edit source]
The goal of early mobilisation and therapy interventions after a burn is to maintain functional mobility and endurance while the body heals. The degree of burn will dictate therapy intensity. The areas affected by the burn will require gentle ROM, which should be slow and smooth to decrease associated pain and inflammation with movement.[1]
Currently there is little research on early mobilisation following acute burns. A 2019 meta-analysis and systematic review of trauma patients in the ICU found that early mobilisation decreased time of mechanical ventilation, but had similar mortality and hospital length of stay compared to those patients that did not receive early mobility.[10] However a 2020 retrospective study of trauma patients in the ICU not only states that early mobility is a safe, feasible and effective strategy to improve functional outcomes, but also that patients who received early mobility were less likely to die in both the ICU and hospital.[11] Please read this article for more in-depth information on early mobilisation of patients in the ICU.
While further research is needed on the effectiveness and risks/benefits of early mobility of patients after burns, data from similar populations suggest the benefits may outweigh no mobility intervention. Please read this article for more in-depth information on post-burn rehabilitation.
Education[edit | edit source]
Due to the long healing and rehabilitation timeframe following a burn, patient and caregiver education is of vital importance for successful burn management and rehabilitation.
This education and training should include:
- ROM and stretching exercises with special consideration given to a patient's fear of movement due to pain
- Contracture aetiology and prevention
- Functional activities and mobility to include assistive device use
- Positioning and pressure relief techniques
- Splint use and wearing schedule
- Infection control
- Anticipated healing times as a patient moves from the acute phase into the subacute phase and beyond[1]
Treatment Red Flags[edit | edit source]
Rehabilitation therapists such as physiotherapists often have the most direct contact with their patients. Therefore, it is important to monitor these patients for treatment red flags and alert the medical team as appropriate.
- Hypovolemic shock
- Infection: this is the most common cause of death of patients with burns who survive the initial injury.
- Compartment syndrome
- Inadequate pain management[1]
Familiarise yourself with the signs and symptoms of sepsis.
Resources[edit | edit source]
Rehabilitation in Conflict and Disasters Field Support[edit | edit source]
- Responding Internationally to Disasters: Do’s and Don’ts
- Early Rehabilitation in Conflict and Disasters, Humanity and Inclusion
- Rehabilitation in Sudden Onset Disasters, Humanity and Inclusion
- Rehabilitation Treatment Planning Tool for Common Conflict and Emergency Related Injuries
Burns Specific Support[edit | edit source]
Technical Standards for Medical Teams[edit | edit source]
- Minimum Technical Standards and Recommendations for Rehabilitation in Emergency Medical Teams
- Minimum Technical Standards and Recommendations for TBI Rehabilitation Teams in Sudden-onset Disasters
References [edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 Lathia C, Skelton P, Clift Z. Early rehabilitation in conflicts and disasters. Handicap International: London, UK. 2020.
- ↑ Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. Burn injury. Nature Reviews Disease Primers. 2020 Feb 13;6(1):1-25.
- ↑ YouTube. Burns: Clinical Estimation – Emergency Medicine | Lecturio. Available from: https://www.youtube.com/watch?v=vCzPNl8EvHM [last accessed 03/03/2022]
- ↑ Capillary nail refill test. Available from: https://medlineplus.gov/ency/article/003394.htm (Accessed 24 October 2020)
- ↑ Capillary nail refill test. Available from: http://pennstatehershey.adam.com/content.aspx?productid=117&pid=1&gid=003394 (last Accessed 25 October 2020
- ↑ YouTube. Capillary Refill Test. Available from: https://www.youtube.com/watch?v=n--wFoZFklg [last accessed 02/03/2022]
- ↑ 7.0 7.1 Legrand M, Barraud D, Constant I, Devauchelle P, Donat N, Fontaine M, Goffinet L, Hoffmann C, Jeanne M, Jonqueres J, Leclerc T. Management of severe thermal burns in the acute phase in adults and children. Anaesthesia Critical Care & Pain Medicine. 2020 Apr 1;39(2):253-67.
- ↑ Puri V, Shrotriya R, Bachhav M. The scourge of burn contractures: Who will bell the cat?. Burns. 2019 Jun 1;45(4):791-7.
- ↑ 9.0 9.1 Parry IS, Schneider JC, Yelvington M, Sharp P, Serghiou M, Ryan CM, Richardson E, Pontius K, Niszczak J, McMahon M, MacDonald LE. Systematic review and expert consensus on the use of orthoses (splints and casts) with adults and children after burn injury to determine practice guidelines. Journal of Burn Care & Research. 2020 May 2;41(3):503-34.
- ↑ Higgins SD, Erdogan M, Coles SJ, Green RS. Early mobilization of trauma patients admitted to intensive care units: a systematic review and meta-analyses. Injury. 2019 Nov 1;50(11):1809-15.
- ↑ Coles SJ, Erdogan M, Higgins SD, Green RS. Impact of an early mobilization protocol on outcomes in trauma patients admitted to the intensive care unit: A retrospective pre-post study. Journal of Trauma and Acute Care Surgery. 2020 Apr 1;88(4):515-21.