Fibrosis: Difference between revisions
No edit summary |
No edit summary |
||
| (14 intermediate revisions by one other user not shown) | |||
| Line 5: | Line 5: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
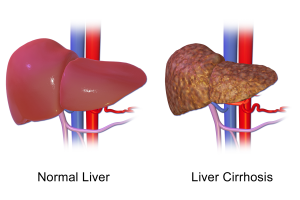
[[File:Liver cirrhosis.png|thumb|Liver Cirrhosis (fibrosis)]] | |||
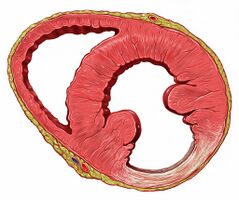
[[File:Heart inferior wall scar.jpeg|thumb|239x239px|Heart inferior wall fibrosis]] | |||
Fibrosis (a pathological feature of many chronic inflammatory diseases) refers to scarring and hardening of tissues and organs. It is defined by the accumulation of excess extracellular matrix components (particularly collagen). When very progressive, the fibrotic process eventually leads to organ malfunction and death. Fibrosis can effect most tissues in the body.<ref name=":1">Wynn TA, Ramalingam TR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3405917/ Mechanisms of fibrosis: therapeutic translation for fibrotic disease]. Nature medicine. 2012 Jul;18(7):1028-40. Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3405917/ (accessed 18.10.2022)</ref>. | |||
Fibrogenesis is becoming increasingly recognised as a major cause of morbidity and death, with a dearth of treatment strategies available to target the pathogenesis of fibrosis.<ref name=":0">News Medical What is Fibrosis? Available:https://www.news-medical.net/health/What-is-Fibrosis.aspx (accessed 18.10.2022)</ref> | |||
== Main Types of Fibrosis == | == Main Types of Fibrosis == | ||
Fibrosis | [[File:Unrepaired extensor tendon injury of left hand following burn.jpg|thumb|Fibrosis after a burn|alt=|300x300px]] | ||
[[File:Frozen shoulder..jpg|thumb|Fibrosis in “Frozen Shoulder”]] | |||
[[File:Cardiac amyloidosis.jpeg|thumb|Myocardial fibrosis]] | |||
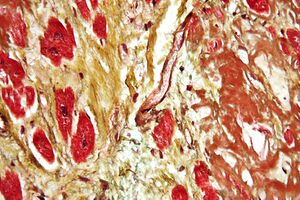
Fibrosis, the excessive accumulation of fibrous connective tissue, can lead to permanent scarring, organ malfunction and, ultimately, death. This can be seen in as seen in end-stage liver disease, kidney disease, idiopathic pulmonary fibrosis, liver cirrhosis and heart failure (cardiac fibrosis). Fibrosis is also a. feature in the following conditions. | |||
# Many chronic [[Autoimmune Disorders|autoimmune disorders]] (eg [[scleroderma]], [[Rheumatoid Arthritis|rheumatoid arthritis]], [[Crohn's Disease|Crohn’s disease]], myelofibrosis and [[Systemic Lupus Erythematosus|systemic lupus erythematosus]]). | |||
# [[Pulmonary Fibrosis|Pulmonary fibrosis,]] as: Replacement fibrosis (as occurs in response to [[Lung Anatomy|lung]] damage caused by infarction or an infection); focal fibrosis, as occurs in a response to irritation by inhaled substances that are inhaled eg [[Silicosis]] or [[Mesothelioma|asbestos]]; diffuse parenchymal lung disease (DPLD).<ref name=":0" /> | |||
# Soft tissue injuries eg Skeletal [[Muscle Injuries|muscle injuries]]: With minor injuries the muscles are able to regenerate completely and recover their usual capabilities. However, in severe injuries, the injured muscle cannot recover to a functional level because of the formation of fibrous scar tissue.<ref>Gardner T, Kenter K, Li Y. [https://www.hindawi.com/journals/jsm/2020/7059057/#conclusion Fibrosis following acute skeletal muscle Injury: mitigation and reversal potential in the clinic]. Journal of Sports Medicine. 2020 Sep 1;2020. Available:https://www.hindawi.com/journals/jsm/2020/7059057/#conclusion (accessed 18.10.2022)</ref> Fibrosis of the [[Joint Classification|joints]] can lead to stiffness and pain in the joints. Fibrosis of the [[Tendon Pathophysiology|tendons]] can lead to eg [[Dupuytren’s Contracture|Dupuytren's contracture]]. Fibrosis of the [[shoulder]] capsule may lead to [[Adhesive Capsulitis|adhesive capsulitis]] (frozen shoulder).<ref>New Medical Types of Fibrosis Available: https://www.news-medical.net/health/Types-of-Fibrosis.aspx (accessed 18.10.2022)</ref> | |||
# Fibrosis is a feature of [[Oncological Disorders|cancers]] (characterized by extracellular matrix deposition, remodeling, and cross-linking). The fibrosis enhances tumor cell growth, survival and migration and also a stiff ECM induces angiogenesis, hypoxia and compromises anti-tumor immunity<ref>Piersma B, Hayward MK, Weaver VM. Fibrosis and cancer: A strained relationship. Biochimica et Biophysica Acta (BBA)-Reviews on Cancer. 2020 Apr 1;1873(2):188356. Available:https://www.sciencedirect.com/science/article/abs/pii/S0304419X19301702 (accessed 19.10.2022)</ref> | |||
# Fibrosis is a feature of chronic graft rejection and the pathogenesis of many progressive [[myopathies]] eg Dysregulated muscle repair with persistent fibrosis rather than correct regeneration plays a major role in the decline and reduced life expectancy associated with severe muscular dystrophies, like [[Duchenne Muscular Dystrophy|Duchenne muscular dystrophy]]<ref name=":1" /><ref>Mann CJ, Perdiguero E, Kharraz Y, Aguilar S, Pessina P, Serrano AL, Muñoz-Cánoves P. Aberrant repair and fibrosis development in skeletal muscle. Skeletal muscle. 2011 Dec;1(1):1-20.Available:https://skeletalmusclejournal.biomedcentral.com/articles/10.1186/2044-5040-1-21#Sec1 (accessed 18.10.2022)</ref> | |||
== Physiotherapy == | |||
Physiotherapy plays a role in eg minimising fibrotic changes, influencing scar tissue strength, living a better quality of life with fibrosis. See links for Physiotherapy specifics. | |||
== References == | == References == | ||
| Line 36: | Line 32: | ||
[[Category:Physiology]] | [[Category:Physiology]] | ||
[[Category:Non Communicable Diseases]] | [[Category:Non Communicable Diseases]] | ||
[[Category:Muscular Dystrophy]] | |||
Latest revision as of 14:25, 27 October 2022
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton and Vidya Acharya
Introduction[edit | edit source]
Fibrosis (a pathological feature of many chronic inflammatory diseases) refers to scarring and hardening of tissues and organs. It is defined by the accumulation of excess extracellular matrix components (particularly collagen). When very progressive, the fibrotic process eventually leads to organ malfunction and death. Fibrosis can effect most tissues in the body.[1].
Fibrogenesis is becoming increasingly recognised as a major cause of morbidity and death, with a dearth of treatment strategies available to target the pathogenesis of fibrosis.[2]
Main Types of Fibrosis[edit | edit source]
Fibrosis, the excessive accumulation of fibrous connective tissue, can lead to permanent scarring, organ malfunction and, ultimately, death. This can be seen in as seen in end-stage liver disease, kidney disease, idiopathic pulmonary fibrosis, liver cirrhosis and heart failure (cardiac fibrosis). Fibrosis is also a. feature in the following conditions.
- Many chronic autoimmune disorders (eg scleroderma, rheumatoid arthritis, Crohn’s disease, myelofibrosis and systemic lupus erythematosus).
- Pulmonary fibrosis, as: Replacement fibrosis (as occurs in response to lung damage caused by infarction or an infection); focal fibrosis, as occurs in a response to irritation by inhaled substances that are inhaled eg Silicosis or asbestos; diffuse parenchymal lung disease (DPLD).[2]
- Soft tissue injuries eg Skeletal muscle injuries: With minor injuries the muscles are able to regenerate completely and recover their usual capabilities. However, in severe injuries, the injured muscle cannot recover to a functional level because of the formation of fibrous scar tissue.[3] Fibrosis of the joints can lead to stiffness and pain in the joints. Fibrosis of the tendons can lead to eg Dupuytren's contracture. Fibrosis of the shoulder capsule may lead to adhesive capsulitis (frozen shoulder).[4]
- Fibrosis is a feature of cancers (characterized by extracellular matrix deposition, remodeling, and cross-linking). The fibrosis enhances tumor cell growth, survival and migration and also a stiff ECM induces angiogenesis, hypoxia and compromises anti-tumor immunity[5]
- Fibrosis is a feature of chronic graft rejection and the pathogenesis of many progressive myopathies eg Dysregulated muscle repair with persistent fibrosis rather than correct regeneration plays a major role in the decline and reduced life expectancy associated with severe muscular dystrophies, like Duchenne muscular dystrophy[1][6]
Physiotherapy[edit | edit source]
Physiotherapy plays a role in eg minimising fibrotic changes, influencing scar tissue strength, living a better quality of life with fibrosis. See links for Physiotherapy specifics.
References[edit | edit source]
- ↑ 1.0 1.1 Wynn TA, Ramalingam TR. Mechanisms of fibrosis: therapeutic translation for fibrotic disease. Nature medicine. 2012 Jul;18(7):1028-40. Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3405917/ (accessed 18.10.2022)
- ↑ 2.0 2.1 News Medical What is Fibrosis? Available:https://www.news-medical.net/health/What-is-Fibrosis.aspx (accessed 18.10.2022)
- ↑ Gardner T, Kenter K, Li Y. Fibrosis following acute skeletal muscle Injury: mitigation and reversal potential in the clinic. Journal of Sports Medicine. 2020 Sep 1;2020. Available:https://www.hindawi.com/journals/jsm/2020/7059057/#conclusion (accessed 18.10.2022)
- ↑ New Medical Types of Fibrosis Available: https://www.news-medical.net/health/Types-of-Fibrosis.aspx (accessed 18.10.2022)
- ↑ Piersma B, Hayward MK, Weaver VM. Fibrosis and cancer: A strained relationship. Biochimica et Biophysica Acta (BBA)-Reviews on Cancer. 2020 Apr 1;1873(2):188356. Available:https://www.sciencedirect.com/science/article/abs/pii/S0304419X19301702 (accessed 19.10.2022)
- ↑ Mann CJ, Perdiguero E, Kharraz Y, Aguilar S, Pessina P, Serrano AL, Muñoz-Cánoves P. Aberrant repair and fibrosis development in skeletal muscle. Skeletal muscle. 2011 Dec;1(1):1-20.Available:https://skeletalmusclejournal.biomedcentral.com/articles/10.1186/2044-5040-1-21#Sec1 (accessed 18.10.2022)