Childhood Obesity: Difference between revisions
Lynne Turner (talk | contribs) (format change around images) |
Kim Jackson (talk | contribs) No edit summary |
||
| (145 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editors ''' - [[User:User Name|Alexander Dow]], [[User:User Name|Andrea Civitarese]], [[User:User Name|Lynne Turner]], [[User:User Name|Alison O’Brien]], [[User:User Name|Rachael Le Page]], [[User:User Name|Courtney Ferguson]] as part of the [[Current_and_Emerging_Roles_in_Physiotherapy_Practice|Queen Margaret University's Current and Emerging Roles in Physiotherapy Practice Project]]<br> | |||
'''Original Editors ''' - Alexander Dow, Andrea Civitarese, Lynne Turner, Alison O’Brien, Rachael Le Page, Courtney Ferguson | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | |||
[[Obesity]] is the excessive or abnormal accumulation of fat or [[Adipose Tissue|adipose]] tissue in the body that may impair health. | |||
The obesity epidemic around the world affects not only adults but also children. About 50% of the time, obesity in childhood is carried into adulthood in a phenomenon known as "tracking." Per the latest data from the World Health Organization, the number of overweight and obese children under five years of age is estimated to be close to 39 million. | |||
</ | * By 2030 some epidemiologists suggest that 20% of the world's population will be obese, i.e., having a body mass index ([[Body Mass Index|BMI]]) of more than 30 kg/m² in adults, or a BMI ≥95th percentile for age and sex in children aged 2 to 18 years. See also [[Waist Measurement|waist measurement]] and [[Body Composition|body composition]] | ||
* Obesity as a disease itself is multifactorial and occurs due to complex interactions occurring between genetics and the environment.<ref>Tirthani E, Said MS, Rehman A. [https://www.statpearls.com/ArticleLibrary/viewarticle/131519 Genetics and Obesity]. StatPearls [Internet]. 2021 Aug 4.Available:https://www.statpearls.com/ArticleLibrary/viewarticle/131519 (accessed 13.11.2021)</ref> | |||
* Overweight and obesity, as well as their related diseases, are largely preventable. Prevention of childhood obesity needs high priority<ref name=":7">World Health Organization. [https://www.who.int/news-room/q-a-detail/noncommunicable-diseases-childhood-overweight-and-obesity Noncommunicable diseases: Childhood overweight and obesity]. Available: https://www.who.int/news-room/q-a-detail/noncommunicable-diseases-childhood-overweight-and-obesity (accessed 9.10.2021)</ref>. | |||
=== Why Does This Matter? === | |||
Obese children carry an increased risk of [[asthma]], [[Diabetes Mellitus Type 2|type 2 diabetes]], and orthopedic disorders. Studies have also found a link between childhood obesity and poor academic performance. | |||
* The roots of childhood obesity can begin in utero. Maternal obesity and excessive weight gain during pregnancy, for example, both correlate with a higher risk of childhood obesity. Moreover, other determinants of childhood obesity, eg rapid weight gain during infancy, are well established before age five. | |||
* Obese children are more likely to become obese adults. As obese adults, they will have a higher risk of many of the major causes of adult mortality, including [[Coronary Artery Disease (CAD)|coronary artery disease]], [[hypertension]], [[stroke]], [[Chronic Kidney Disease|chronic kidney]] and [[Liver Disease|liver]] disease as well as many types of cancer. <ref>ASN Childhood Obesity Prevention Strategies Must Start Early Available:https://nutrition.org/childhood-obesity-prevention-strategies-must-start-early/ (Accessed 13.11.2021)</ref> | |||
This less than 2 minute video is a worthwhile watch.{{#ev:youtube|5Km1fFLX6T8|600}} <ref>Childhood Obesity in the UK Available from: https://www.youtube.com/watch?v=5Km1fFLX6T8 [last accessed 15/03/18]</ref> | |||
== | == Etiology == | ||
[[File:Junk food.jpg|right|frameless]] | |||
The fundamental cause of childhood overweight and obesity is an energy imbalance between calories consumed and calories expended. | |||
Global increases in childhood overweight and obesity are attributable to several factors. | |||
# There has been a global shift in diet towards increased intake of energy-dense foods that are high in fat and sugars but low in vitamins, minerals and other healthy micronutrients. | |||
# There is also a trend towards decreased [[physical activity]] levels due to the increasingly sedentary nature of many forms of recreation time, changing modes of transportation and increasing urbanization. | |||
The problem is societal and therefore it demands a population-based multisectoral, multidisciplinary and culturally relevant approach. | |||
* Unlike most adults, children and adolescents cannot choose the environment in which they live or the food they eat. They also have a limited ability to understand the long-term consequences of their behaviour. They therefore require special attention when fighting the obesity epidemic<ref name=":7" />. | |||
* | |||
== Fighting the Epidemic == | |||
[[File:Parent_image_4.png|frameless|499x499px|alt=|right]] | |||
WHO recommends the following to reduce and prevent childhood overweight and obesity: | |||
# Increase consumption of fruit and vegetables, as well as legumes, whole grains and nuts | |||
# Limit energy intake from total fats and shift fat consumption away from saturated fats to unsaturated fats | |||
# Limit the intake of sugars | |||
# Be physically active and accumulate at least 60 minutes of regular, moderate- to vigorous-intensity activity each day that is developmentally appropriate. | |||
Image 3: Eat well guide for parental guidance . | |||
See also | |||
# [[Physiotherapy communication approaches in management of obesity and overweight]] | |||
# [[Promoting Active Living in Young People Through Behaviour Change]] | |||
# [[Fostering Behaviour Change in Obese Adolescents]] | |||
==== ' | == The Benefits Of Physical Activity== | ||
Physical activity and inactivity can have a big effect on a child's health and development in many ways. It is important to know and understand the benefits of regular activity and the risk of inactivity for a child between the ages of 5 - 12 years old. | |||
=== Regular Activity === | |||
Encouraging a child participate in regular physical activity between the ages of 5 - 12 years old will benefit their body and mind health in a variety of ways including mentally, physically and academically <ref>Gov.UK. Publication: Start active, stay active: infographics on physical activity. Available from:https://www.gov.uk/government/publications/start-active-stay-active-infographics-on-physical-activity (accessed 02 April 2018)</ref><ref>SSEHS Active. Interpreting the UK physical activity guidelines for children. Available from:http://www.ssehsactive.org.uk/young-people-resources-and-publications-item/39/443/index.html (accessed 02 April 2018)</ref><ref name=":0">Great Ormond Street. Exercise for children and young people. Available from: https://www.gosh.nhs.uk/medical-information/general-health-advice/leading-active-lifestyle/exercise-children-and-young-people (accessed 02 April 2018)</ref><ref name=":1">Kohl III, H. W., and CooK, H. D. Educating the Student Body: Taking Physical Activity and Physical Education to School. Washington: The National Academies Press. Available from: https://www.ncbi.nlm.nih.gov/books/NBK201497/<nowiki/>(accessed 02 April 2018)</ref><ref>SSEHS Active. Children and young people evidence briefing. Available from:http://www.ssehsactive.org.uk/resources-and-publications-item/40/475/index.html (accessed 02 April 2018) </ref>. These benefits are detailed below: | |||
[[File:Screen Shot 2018-03-28 at 19.36.55.png|left|381x381px|frameless]] | |||
[[File:Screen Shot 2018-03-28 at 19.37.03.png|centre|381x381px|frameless]] | |||
<br /> | |||
The video below provides more details of the top 5 benefits of physical activity for children. | |||
==== ' | {{#ev:youtube|nD-0Wc6eSUE|600}} <ref name=":2">5 Reasons Why Physical Activity is Important for Children Available from: https://www.youtube.com/watch?v=nD-0Wc6eSUE [last accessed 28/03/18]</ref> | ||
[[File: | === Inactivity === | ||
It is common to find children playing video games and watching television, however, this leads to a lot of sitting and therefore to an inactive lifestyle which can have a detrimental effect on on children's future health<ref name=":0" /><ref name=":1" />. These effects may not show until later life. It is important to be aware of the higher risk of developing non communicable diseases due to childhood inactivity<ref name=":1" /> and encourage regular physical activity to help reduce and prevent a child developing them in adulthood. | |||
* Obesity | |||
* Heart disease eg [[Coronary Artery Disease (CAD)|coronary arterial disease]] | |||
*[[Stroke]] | |||
* Diabetes | |||
*[[Oncology|Cancer]] | |||
* Mental health disease eg anxiety, [[depression]] and [[dementia]] | |||
* Earlier death | |||
== Physical Activity Guidelines for Children (Age 5-12) == | |||
[[File:Infograph.png|alt=|right|frameless|779x779px]] | |||
Children (aged 5-12) should partake in at least 60 minutes of physical activity a day - this should range from moderate activity to vigorous activity<ref name=":5">NHS., 2015. ''Physical Activity Guidelines for Children and Young People'' [online]. [viewed 9<sup>th</sup> April 2018]. Available from: <nowiki>https://www.nhs.uk/Livewell/fitness/Pages/physical-activity-guidelines-for-young-people.aspx</nowiki> | |||
</ref>. Amounts of physical activity greater than 60 minutes, provides additional heath benefits to your child<ref>World Health Organization., 2016. ''Physical Activity and Young People'' [online]. [viewed 9<sup>th</sup> April 2018]. Avaiable from: <nowiki>http://www.who.int/dietphysicalactivity/factsheet_young_people/en/</nowiki> | |||
</ref>. | |||
''' | '''Moderate Activity'''[[File:30440825_10160213199190285_6406574266132725760_n.png|right|frameless|156x156px]] | ||
Moderate activity raises the heart rate and can make a person sweat. Examples of activities which involve moderate exertion for children include: | |||
* | * Cycling on flat ground | ||
* | * Walking to school | ||
* | * Playing in the playground | ||
''' | * Walking the dog | ||
* Riding a scooter | |||
* Rollerblading<ref name=":5" /> | |||
* | '''Vigorous Activity'''[[File:30414685_10160213199510285_1474170515588382720_n.png|right|frameless|232x232px]] | ||
* | Vigorous activity is known to improve general health, bone and muscle strength and self-esteem. Vigorous activity can bring health benefits over and above that of moderate activity. Every one-minute of vigorous activity provides the same health benefits as two-minutes of moderate activity <ref name=":5" />. eg | ||
* Swimming | |||
* | * Running | ||
* | * Gymnastics | ||
* Football | |||
* Karate | |||
* Rugby<ref name=":5" /> | |||
'''Bone Strengthening Activities'''[[File:Screen_Shot_2018-04-09_at_00.05.49.png|right|frameless|215x215px]] | |||
Children should include [[bone]] and muscle [[Strength Training|strengthening]] exercises at least 3 days a week. Many vigorous activities can help to build strong muscles and bones in children. This can include anything involving running and jumping, such as football or gymnastics<ref name=":5" />. eg | |||
* Body weight lifting exercises | |||
* Jumping and climbing activites | |||
* Hopscotch | |||
* Rope Skipping | |||
Examples of suitable muscle-strengthening activities for children: | |||
* Sit-ups and Press-ups | |||
* Gymnastics | |||
* Resistance band exercises | |||
* Rock Climbing<ref name=":5" /> | |||
Click [https://www.nhs.uk/Livewell/fitness/Documents/children-and-young-people-5-18-years.pdf <u>here</u>] to download a helpful fact sheet on physical activity guidelines for children <ref>GOV.UK. 2011. ''UK Physical Activity Guidelines'' [online]. [viewed 9<sup>th</sup> April 2018]. Available from: <nowiki>https://www.gov.uk/government/publications/uk-physical-activity-guidelines</nowiki> | |||
</ref>. | |||
== Managing Childhood Obesity == | |||
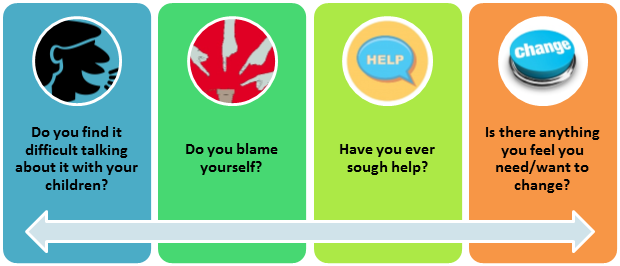
See [[Management of Obesity]][[File:Parent 1 image.png|frameless|620x620px|alt=|right]]Encourage parents to take proactive steps in managing their child's weight<ref>TURNER, K.M., SALISBURY, C. AND SHIELD, J.P., 2011. Parents’ views and experiences of childhood obesity management in primary care: a qualitative study. ''Family Practice'', ''29''(4), pp.476-481.</ref>'''.''' Once they have identified problems it is important to take steps to effect change. | |||
[[File: | |||
= | Remind parents they are not alone, they can consult their General Practitioner and other health professionals for advice<ref name=":6">ACADEMY OF NUTRITION AND DIETETICS., 2017. ''How to Talk to Kids about Weight and Obesity'' [online]. [viewed 30 March 2018]. Available from: ''<nowiki>https://www.eatright.org/health/weight-loss/overweight-and-obesity/how-to-talk-to-kids-about-weight-and-obesity</nowiki>.'' </ref> <ref>CENTER FOR DISEASE CONTROL AND PREVENTION., 2017. ''Tips for Parents-Ideas to Help Children and Maintain a Healthy Weight'' [online]. [viewed 29 March 2018]. Available from: <nowiki>https://www.cdc.gov/healthyweight/children/index.html</nowiki>. | ||
</ref>. | |||
== | == Apps == | ||
We are in the age of technology and it may be easier to encourage children to get active by the use of free online Apps. Below is a list of free apps online that may help parents to engage their child in physical activity and also provide ideas of activities. This is not an exhaustive list and there is a wide variety and many more apps available. | |||
# '''HOOP:''' Find and book fun things to do in your local area for children aged 0-11 years old. ([https://itunes.apple.com/gb/app/hoop-whats-on-for-families/id996073365?mt=8 iOS] & [https://play.google.com/store/apps/details?id=uk.co.hoop.android&hl=en_GB Android]) | |||
# '''Wuf Shanti Yoga Fun Machine:''' Yoga app using games and music to promote health and happiness for your child through yoga, meditation and mindfulness. ([https://itunes.apple.com/us/app/wuf-shanti-yoga-fun-machine/id1296345752?mt=8 iOS]) | |||
== Conclusion == | == Conclusion == | ||
Childhood obesity between the ages of 5-12 years old is rising and is a current global concern and challenge. Unfortunately, in this present age the growing popularity in the daily use of technology in children, among the many other barriers mentioned above, is enhancing an inactive lifestyle. It is important to recognise and understand childhood obesity and how to encourage children to become more active and make changes to help manage a child’s weight and maintain a healthy lifestyle. | |||
== Useful Links == | == Useful Links == | ||
* [https://www.nhs.uk/Livewell/childhealth6-15/Pages/child-health-measurement-programme-very-overweight-advice.aspx NHS Choices: What can I do if my child is very overweight?] | |||
* [http://www.bbc.co.uk/news/health-37116611 BBC: What to do if your child is overweight] | |||
* [https://www.nhs.uk/change4life NHS: Change 4 Life] | |||
*[https://www.familiesonline.co.uk/child/child-wellbeing Families online: child-wellbeing] | |||
*[http://www.more-life.co.uk/ More Life] | |||
*[https://www.helpguide.org/articles/diets/childhood-obesity-and-weight-problems.htm Childhood Obesity and Weight Problems Help Guide] | |||
*[https://www.eatright.org/health/weight-loss/overweight-and-obesity/how-to-talk-to-kids-about-weight-and-obesity. Kids eat right: How to Talk to Kids about Weight and Obesity] | |||
*[https://www.cdc.gov/healthyweight/children/index.html Tips for Parents – Ideas to Help Children and Maintain a Healthy Weight: Centers for Disease Control and Prevention] | |||
*[https://www.bbcgoodfood.com/recipes/collection/school-lunch Healthy Kids' Lunchbox Recipe Ideas] | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Queen_Margaret_University_Project]] [[Category: | [[Category:Queen_Margaret_University_Project]] | ||
[[Category:Paediatrics]] | |||
[[Category:Paediatrics - Conditions]] | |||
[[Category:Paediatrics - Physical Activity]] | |||
Latest revision as of 15:20, 15 November 2021
Top Contributors - Andrea Civitarese, Rachael Le Page, Lynne Turner, Kim Jackson, Lucinda hampton, Courtney Ferguson, Alison O' Brien, Alexander Dow and Rachael Lowe
Introduction[edit | edit source]
Obesity is the excessive or abnormal accumulation of fat or adipose tissue in the body that may impair health.
The obesity epidemic around the world affects not only adults but also children. About 50% of the time, obesity in childhood is carried into adulthood in a phenomenon known as "tracking." Per the latest data from the World Health Organization, the number of overweight and obese children under five years of age is estimated to be close to 39 million.
- By 2030 some epidemiologists suggest that 20% of the world's population will be obese, i.e., having a body mass index (BMI) of more than 30 kg/m² in adults, or a BMI ≥95th percentile for age and sex in children aged 2 to 18 years. See also waist measurement and body composition
- Obesity as a disease itself is multifactorial and occurs due to complex interactions occurring between genetics and the environment.[1]
- Overweight and obesity, as well as their related diseases, are largely preventable. Prevention of childhood obesity needs high priority[2].
Why Does This Matter?[edit | edit source]
Obese children carry an increased risk of asthma, type 2 diabetes, and orthopedic disorders. Studies have also found a link between childhood obesity and poor academic performance.
- The roots of childhood obesity can begin in utero. Maternal obesity and excessive weight gain during pregnancy, for example, both correlate with a higher risk of childhood obesity. Moreover, other determinants of childhood obesity, eg rapid weight gain during infancy, are well established before age five.
- Obese children are more likely to become obese adults. As obese adults, they will have a higher risk of many of the major causes of adult mortality, including coronary artery disease, hypertension, stroke, chronic kidney and liver disease as well as many types of cancer. [3]
This less than 2 minute video is a worthwhile watch.
Etiology[edit | edit source]
The fundamental cause of childhood overweight and obesity is an energy imbalance between calories consumed and calories expended.
Global increases in childhood overweight and obesity are attributable to several factors.
- There has been a global shift in diet towards increased intake of energy-dense foods that are high in fat and sugars but low in vitamins, minerals and other healthy micronutrients.
- There is also a trend towards decreased physical activity levels due to the increasingly sedentary nature of many forms of recreation time, changing modes of transportation and increasing urbanization.
The problem is societal and therefore it demands a population-based multisectoral, multidisciplinary and culturally relevant approach.
- Unlike most adults, children and adolescents cannot choose the environment in which they live or the food they eat. They also have a limited ability to understand the long-term consequences of their behaviour. They therefore require special attention when fighting the obesity epidemic[2].
Fighting the Epidemic[edit | edit source]
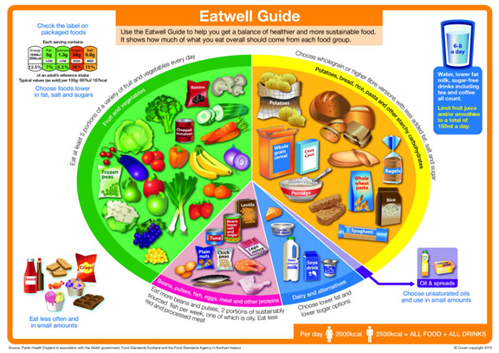
WHO recommends the following to reduce and prevent childhood overweight and obesity:
- Increase consumption of fruit and vegetables, as well as legumes, whole grains and nuts
- Limit energy intake from total fats and shift fat consumption away from saturated fats to unsaturated fats
- Limit the intake of sugars
- Be physically active and accumulate at least 60 minutes of regular, moderate- to vigorous-intensity activity each day that is developmentally appropriate.
Image 3: Eat well guide for parental guidance .
See also
- Physiotherapy communication approaches in management of obesity and overweight
- Promoting Active Living in Young People Through Behaviour Change
- Fostering Behaviour Change in Obese Adolescents
The Benefits Of Physical Activity[edit | edit source]
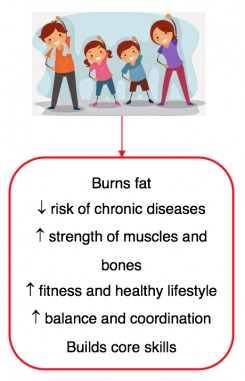
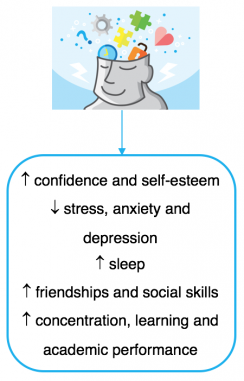
Physical activity and inactivity can have a big effect on a child's health and development in many ways. It is important to know and understand the benefits of regular activity and the risk of inactivity for a child between the ages of 5 - 12 years old.
Regular Activity[edit | edit source]
Encouraging a child participate in regular physical activity between the ages of 5 - 12 years old will benefit their body and mind health in a variety of ways including mentally, physically and academically [5][6][7][8][9]. These benefits are detailed below:
The video below provides more details of the top 5 benefits of physical activity for children.
Inactivity[edit | edit source]
It is common to find children playing video games and watching television, however, this leads to a lot of sitting and therefore to an inactive lifestyle which can have a detrimental effect on on children's future health[7][8]. These effects may not show until later life. It is important to be aware of the higher risk of developing non communicable diseases due to childhood inactivity[8] and encourage regular physical activity to help reduce and prevent a child developing them in adulthood.
- Obesity
- Heart disease eg coronary arterial disease
- Stroke
- Diabetes
- Cancer
- Mental health disease eg anxiety, depression and dementia
- Earlier death
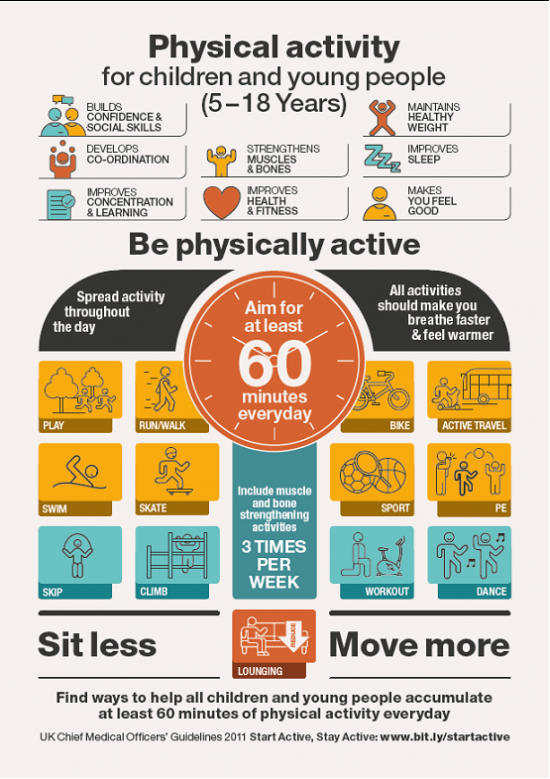
Physical Activity Guidelines for Children (Age 5-12)[edit | edit source]
Children (aged 5-12) should partake in at least 60 minutes of physical activity a day - this should range from moderate activity to vigorous activity[11]. Amounts of physical activity greater than 60 minutes, provides additional heath benefits to your child[12].
Moderate Activity
Moderate activity raises the heart rate and can make a person sweat. Examples of activities which involve moderate exertion for children include:
- Cycling on flat ground
- Walking to school
- Playing in the playground
- Walking the dog
- Riding a scooter
- Rollerblading[11]
Vigorous Activity
Vigorous activity is known to improve general health, bone and muscle strength and self-esteem. Vigorous activity can bring health benefits over and above that of moderate activity. Every one-minute of vigorous activity provides the same health benefits as two-minutes of moderate activity [11]. eg
- Swimming
- Running
- Gymnastics
- Football
- Karate
- Rugby[11]
Bone Strengthening Activities
Children should include bone and muscle strengthening exercises at least 3 days a week. Many vigorous activities can help to build strong muscles and bones in children. This can include anything involving running and jumping, such as football or gymnastics[11]. eg
- Body weight lifting exercises
- Jumping and climbing activites
- Hopscotch
- Rope Skipping
Examples of suitable muscle-strengthening activities for children:
- Sit-ups and Press-ups
- Gymnastics
- Resistance band exercises
- Rock Climbing[11]
Click here to download a helpful fact sheet on physical activity guidelines for children [13].
Managing Childhood Obesity[edit | edit source]
Encourage parents to take proactive steps in managing their child's weight[14]. Once they have identified problems it is important to take steps to effect change.
Remind parents they are not alone, they can consult their General Practitioner and other health professionals for advice[15] [16].
Apps[edit | edit source]
We are in the age of technology and it may be easier to encourage children to get active by the use of free online Apps. Below is a list of free apps online that may help parents to engage their child in physical activity and also provide ideas of activities. This is not an exhaustive list and there is a wide variety and many more apps available.
- HOOP: Find and book fun things to do in your local area for children aged 0-11 years old. (iOS & Android)
- Wuf Shanti Yoga Fun Machine: Yoga app using games and music to promote health and happiness for your child through yoga, meditation and mindfulness. (iOS)
Conclusion[edit | edit source]
Childhood obesity between the ages of 5-12 years old is rising and is a current global concern and challenge. Unfortunately, in this present age the growing popularity in the daily use of technology in children, among the many other barriers mentioned above, is enhancing an inactive lifestyle. It is important to recognise and understand childhood obesity and how to encourage children to become more active and make changes to help manage a child’s weight and maintain a healthy lifestyle.
Useful Links[edit | edit source]
- NHS Choices: What can I do if my child is very overweight?
- BBC: What to do if your child is overweight
- NHS: Change 4 Life
- Families online: child-wellbeing
- More Life
- Childhood Obesity and Weight Problems Help Guide
- Kids eat right: How to Talk to Kids about Weight and Obesity
- Tips for Parents – Ideas to Help Children and Maintain a Healthy Weight: Centers for Disease Control and Prevention
- Healthy Kids' Lunchbox Recipe Ideas
References[edit | edit source]
- ↑ Tirthani E, Said MS, Rehman A. Genetics and Obesity. StatPearls [Internet]. 2021 Aug 4.Available:https://www.statpearls.com/ArticleLibrary/viewarticle/131519 (accessed 13.11.2021)
- ↑ 2.0 2.1 World Health Organization. Noncommunicable diseases: Childhood overweight and obesity. Available: https://www.who.int/news-room/q-a-detail/noncommunicable-diseases-childhood-overweight-and-obesity (accessed 9.10.2021)
- ↑ ASN Childhood Obesity Prevention Strategies Must Start Early Available:https://nutrition.org/childhood-obesity-prevention-strategies-must-start-early/ (Accessed 13.11.2021)
- ↑ Childhood Obesity in the UK Available from: https://www.youtube.com/watch?v=5Km1fFLX6T8 [last accessed 15/03/18]
- ↑ Gov.UK. Publication: Start active, stay active: infographics on physical activity. Available from:https://www.gov.uk/government/publications/start-active-stay-active-infographics-on-physical-activity (accessed 02 April 2018)
- ↑ SSEHS Active. Interpreting the UK physical activity guidelines for children. Available from:http://www.ssehsactive.org.uk/young-people-resources-and-publications-item/39/443/index.html (accessed 02 April 2018)
- ↑ 7.0 7.1 Great Ormond Street. Exercise for children and young people. Available from: https://www.gosh.nhs.uk/medical-information/general-health-advice/leading-active-lifestyle/exercise-children-and-young-people (accessed 02 April 2018)
- ↑ 8.0 8.1 8.2 Kohl III, H. W., and CooK, H. D. Educating the Student Body: Taking Physical Activity and Physical Education to School. Washington: The National Academies Press. Available from: https://www.ncbi.nlm.nih.gov/books/NBK201497/(accessed 02 April 2018)
- ↑ SSEHS Active. Children and young people evidence briefing. Available from:http://www.ssehsactive.org.uk/resources-and-publications-item/40/475/index.html (accessed 02 April 2018)
- ↑ 5 Reasons Why Physical Activity is Important for Children Available from: https://www.youtube.com/watch?v=nD-0Wc6eSUE [last accessed 28/03/18]
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 NHS., 2015. Physical Activity Guidelines for Children and Young People [online]. [viewed 9th April 2018]. Available from: https://www.nhs.uk/Livewell/fitness/Pages/physical-activity-guidelines-for-young-people.aspx
- ↑ World Health Organization., 2016. Physical Activity and Young People [online]. [viewed 9th April 2018]. Avaiable from: http://www.who.int/dietphysicalactivity/factsheet_young_people/en/
- ↑ GOV.UK. 2011. UK Physical Activity Guidelines [online]. [viewed 9th April 2018]. Available from: https://www.gov.uk/government/publications/uk-physical-activity-guidelines
- ↑ TURNER, K.M., SALISBURY, C. AND SHIELD, J.P., 2011. Parents’ views and experiences of childhood obesity management in primary care: a qualitative study. Family Practice, 29(4), pp.476-481.
- ↑ ACADEMY OF NUTRITION AND DIETETICS., 2017. How to Talk to Kids about Weight and Obesity [online]. [viewed 30 March 2018]. Available from: https://www.eatright.org/health/weight-loss/overweight-and-obesity/how-to-talk-to-kids-about-weight-and-obesity.
- ↑ CENTER FOR DISEASE CONTROL AND PREVENTION., 2017. Tips for Parents-Ideas to Help Children and Maintain a Healthy Weight [online]. [viewed 29 March 2018]. Available from: https://www.cdc.gov/healthyweight/children/index.html.