Statins: Difference between revisions
(tbd) |
(Completed my edits for this page for the month) |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
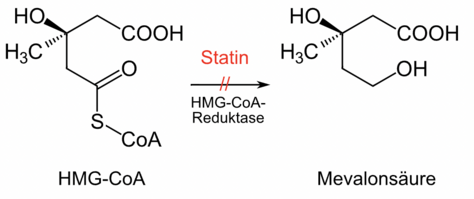
[[File:Statin.png|thumb|474x474px|Schematic mechanism of action of statins]] | [[File:Statin.png|thumb|474x474px|Schematic mechanism of action of statins]] | ||
Statin medications are a class of [[Lipids|lipid]]-lowering medications that decrease illness and mortality in those who are at high risk of [[Cardiovascular Disease|cardiovascular disease]], being the most common cholesterol-lowering drugs<ref name=":0">Sizar O, Khare S, Jamil RT, Talati R. | Statin medications are a class of [[Lipids|lipid]]-lowering medications that decrease illness and mortality in those who are at high risk of [[Cardiovascular Disease|cardiovascular disease]], being the most common cholesterol-lowering drugs.<ref name=":0">Sizar O, Khare S, Jamil RT, Talati R. Statin medications. StatPearls [Internet]. 2024. Available from:https://www.ncbi.nlm.nih.gov/books/NBK430940/</ref> | ||
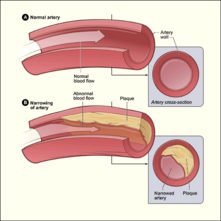
# Statins are 3-hydroxyl-3-methylglutaryl coenzyme A reductase (HMG-CoA Reductase) inhibitors. Statins competitively inhibit HMG-CoA reductase, which limits the rate of cholesterol synthesis (primarily in the liver). As a result, statins break down LDL, decrease the synthesis of VLDL, and increase HDL. Through this mechanism, statins can reduce the amount of plaque that forms in the arteries (see '''[[Atherosclerosis]]''' for more information). <ref name=":1">Bansal AB, Cassagnol M. HMG-CoA Reductase Inhibitors. StatPearls [Internet]. 2024. Available from: [[/www.ncbi.nlm.nih.gov/books/NBK542212/|https://www.ncbi.nlm.nih.gov/books/NBK542212/]]</ref> | # Statins are 3-hydroxyl-3-methylglutaryl coenzyme A reductase (HMG-CoA Reductase) inhibitors. Statins competitively inhibit HMG-CoA reductase, which limits the rate of cholesterol synthesis (primarily in the liver). As a result, statins break down LDL, decrease the synthesis of VLDL, and increase HDL. Through this mechanism, statins can reduce the amount of plaque that forms in the arteries (see '''[[Atherosclerosis]]''' for more information).<ref name=":1">Bansal AB, Cassagnol M. HMG-CoA Reductase Inhibitors. StatPearls [Internet]. 2024. Available from: [[/www.ncbi.nlm.nih.gov/books/NBK542212/|https://www.ncbi.nlm.nih.gov/books/NBK542212/]]</ref> | ||
# Statins may also inhibit many of the structural and functional components of the [[Atherosclerosis|arteriosclerotic]] process. Structural effects include reductions in vascular [[Muscle: Smooth|smooth muscle]] hypertrophy and proliferation, fibrin deposition, and collagen cross-linking. Among the functional effects are improvements in [[Reticuloendothelial System|endothelial function,]] vasodilation due to increased nitric oxide production, reduction in inflammatory [[cytokines]] and [[Free Radicals|reactive oxygen species]], and down-regulation of [[Angiotensin Inhibitors and Blockers for Treating Hypertension|angiotensin]] II and endothelin receptors.<ref>Mangat S, Agarwal S, Rosendorff C. [https://journals.sagepub.com/doi/abs/10.1177/1074248407300380 Do statins lower blood pressure?]. Journal of cardiovascular pharmacology and therapeutics. 2007 Jun;12(2):112-23.Available: https://journals.sagepub.com/doi/abs/10.1177/1074248407300380<nowiki/>(accessed 9.4.2022)</ref> | # Statins may also inhibit many of the structural and functional components of the [[Atherosclerosis|arteriosclerotic]] process. Structural effects include reductions in vascular [[Muscle: Smooth|smooth muscle]] hypertrophy and proliferation, fibrin deposition, and collagen cross-linking. Among the functional effects are improvements in [[Reticuloendothelial System|endothelial function,]] vasodilation due to increased nitric oxide production, reduction in inflammatory [[cytokines]] and [[Free Radicals|reactive oxygen species]], and down-regulation of [[Angiotensin Inhibitors and Blockers for Treating Hypertension|angiotensin]] II and endothelin receptors.<ref>Mangat S, Agarwal S, Rosendorff C. [https://journals.sagepub.com/doi/abs/10.1177/1074248407300380 Do statins lower blood pressure?]. Journal of cardiovascular pharmacology and therapeutics. 2007 Jun;12(2):112-23.Available: https://journals.sagepub.com/doi/abs/10.1177/1074248407300380<nowiki/>(accessed 9.4.2022)</ref> | ||
| Line 17: | Line 17: | ||
Clinicians use statin medications for the treatment of: | Clinicians use statin medications for the treatment of: | ||
* [[Hypercholesterolemia]] | * [[Hypercholesterolemia]] | ||
* [[Hyperlipidemia|Hyperlipoproteinemia]] | * [[Hyperlipidemia|Hyperlipoproteinemia]] | ||
* Hypertriglyceridemia | * Hypertriglyceridemia | ||
| Line 27: | Line 27: | ||
== Brief Literature Review == | == Brief Literature Review == | ||
* A 2019 network meta-analysis compared the benefits and harms of statins in secondary prevention for patients with ischemic [[stroke]]. The resultant conclusion suggests statins are no better than placebo in preventing all strokes and all-cause mortality, but reduce the risk of recurrent ischemic strokes and other cardiovascular events if a patient had a previous stroke or [[Transient Ischaemic Attack (TIA)|transient ischemic attack]]. | * A 2019 systematic review and network meta-analysis compared the benefits and harms of statins in secondary prevention for patients with ischemic [[stroke]]. The resultant conclusion suggests statins are no better than placebo in preventing all strokes and all-cause mortality, but reduce the risk of recurrent ischemic strokes and other cardiovascular events if a patient had a previous stroke or [[Transient Ischaemic Attack (TIA)|transient ischemic attack]].<ref>Tramacere I, Boncoraglio GB, Banzi R, Del Giovane C, Kwag KH, Squizzato A, Moja L. [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-019-1298-5 Comparison of statins for secondary prevention in patients with ischemic stroke or transient ischemic attack: a systematic review and network meta-analysis.] BMC Med. 2019 Mar 26;17(1):67.</ref> | ||
* A 2018 systematic review with meta-analysis suggests that more intensive pharmacotherapeutic LDL-C lowering was associated with a greater reduction in risk of total and cardiovascular mortality compared to less intensive LDL-C lowering. This effect is related to the individual's baseline LDL-C level, as there was no significant difference when LDL-C was less than 100 mg/dL at baseline. | * A 2018 systematic review with meta-analysis suggests that more intensive pharmacotherapeutic LDL-C lowering (via statin dosage) was associated with a greater reduction in risk of total and cardiovascular mortality compared to less intensive LDL-C lowering. This effect is related to the individual's baseline LDL-C level, as there was no significant difference when LDL-C was less than 100 mg/dL at baseline.<ref>Navarese EP, Robinson JG, Kowalewski M, Kolodziejczak M, Andreotti F, Bliden K, Tantry U, Kubica J, Raggi P, Gurbel PA. [https://jamanetwork.com/journals/jama/fullarticle/2678614 Association Between Baseline LDL-C Level and Total and Cardiovascular Mortality After LDL-C Lowering: A Systematic Review and Meta-analysis.] JAMA. 2018 Apr 17;319(15):1566-1579.</ref> | ||
* | * A 2022 statement from the United States Preventive Task Force recommends the prescription of a statin for the primary prevention of [[Cardiovascular Disease]] (CVD) in adults aged 40 to 75 years who have at least 1 CVD risk factor ([[dyslipidemia]], [[diabetes]], [[hypertension]], [[Smoking and Stroke|smoking]]), and an estimated 10-year CVD risk of 10+%.<ref>US Preventive Services Task Force; Mangione CM, Barry MJ, Nicholson WK, Cabana M, Chelmow D, Coker TR, Davis EM, Donahue KE, Jaén CR, Kubik M, Li L, Ogedegbe G, Pbert L, Ruiz JM, Stevermer J, Wong JB. [https://jamanetwork.com/journals/jama/fullarticle/2795521 Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: US Preventive Services Task Force Recommendation Statement.] JAMA. 2022 Aug 23;328(8):746-753.</ref> | ||
== Adverse Effects == | == Adverse Effects == | ||
| Line 35: | Line 35: | ||
Statins are usually well-tolerated, with [[myositis]], [[rhabdomyolysis]], hepatotoxicity, and [[Diabetes Mellitus Type 2|diabetes mellitus]] being the most common adverse reactions. | Statins are usually well-tolerated, with [[myositis]], [[rhabdomyolysis]], hepatotoxicity, and [[Diabetes Mellitus Type 2|diabetes mellitus]] being the most common adverse reactions. | ||
# | # Statin-associated muscle symptoms may present as diffuse myalgias or otherwise unexplainable muscle tenderness or weakness. Of all statin-associated muscle symptoms (SAMS), myalgia is the most common, affecting 5-10% of users. These symptoms are generally dose dependent, and resolve upon discontinuation of medication.<ref name=":2">Thompson PD, Panza G, Zaleski A, Taylor B. [https://www.sciencedirect.com/science/article/pii/S0735109716016922?via%3Dihub Statin-Associated Side Effects.] J Am Coll Cardiol. 2016 May 24;67(20):2395-2410.</ref> | ||
# Rhabdomyolysis is the most serious complication of statin use, but its occurrence is rare. | # [[Rhabdomyolysis]] is the most serious complication of statin use, but its occurrence is rare (current incidence rate of 1 case per 10,000 person-years of treatment after market removal of cerivastatin).<ref name=":2" /> | ||
# Statin-associated immune-mediated necrotizing [[Inflammatory Myopathies|myopathy]](IMNM) can occur due to the development of [[Immunoglobulins (Ig)|antibodies]] against the HMG-CoA reductase [[Enzymes|enzyme]]. Symmetrical, proximal muscle weakness with significantly increased creatine phosphokinase (CPK) that continues for months after ceasing statins is common in IMNM<ref> | # Statin-associated immune-mediated necrotizing [[Inflammatory Myopathies|myopathy]](IMNM) can occur due to the development of [[Immunoglobulins (Ig)|antibodies]] against the HMG-CoA reductase [[Enzymes|enzyme]]. Symmetrical, proximal muscle weakness with significantly increased creatine phosphokinase (CPK) that continues for months after ceasing statins is common in IMNM.<ref name=":0" /> | ||
A notable adverse event occurs when consuming grapefruit juice while taking statins. Grapefruit juice increases the systemic concentrations of statins, thus increasing the risk of all side effects, including all SAMS (particularly myalgia), [[Liver Disease|liver damage]], and [[Chronic Kidney Disease|kidney failure]].<ref name=":2" /> | |||
[[Smoking and Exercise|Smoking cigarettes]] should also be avoided when taking statins. Smoking decreases the positive effects of statins. Smokers had a 74 to 86 % higher risk of events.<ref>Milionis HJ, Rizos E, Mikhailidis DP. [https://journals.sagepub.com/doi/10.1177/000331970105200901#:~:text=Smoking%20markedly%20increased%20the%20risk,trials%20were%2023%2D61%25. Smoking diminishes the beneficial effect of statins: observations from the landmark trials.] Angiology. 2001 Sep;52(9):575-87.</ref> | |||
[[ | == Physiotherapy Implications == | ||
Statins may increase the incidence of exercise-related muscle complaints and in some studies augment the exercise-induced rise in muscle enzymes, but statins do not consistently reduce muscle strength, endurance, overall [[Therapeutic Exercise|exercise]] performance or [[Physical Activity|physical activity.]]<ref>Noyes AM, Thompson PD. [https://pubmed.ncbi.nlm.nih.gov/28807461/ The effects of statins on exercise and physical activity]. Journal of Clinical Lipidology. 2017 Sep 1;11(5):1134-44. </ref> | |||
When lab values are available, monitoring [[Creatine Phosphokinase (CK or CPK)]] can be useful to identify clinical rhabdomyolysis. Although SAMS can occur without an increase in CK, certain health organizations categorize SAMS based on CK elevation.<ref name=":2" /> See our page on [[Rhabdomyolysis]] and [[Rhabdomyolysis Case Study|a rhabdomyolysis case study]] for effective management of patients with this condition. | |||
== References == | == References == | ||
Latest revision as of 01:41, 13 May 2024
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton and Mason Trauger
Introduction[edit | edit source]
Statin medications are a class of lipid-lowering medications that decrease illness and mortality in those who are at high risk of cardiovascular disease, being the most common cholesterol-lowering drugs.[1]
- Statins are 3-hydroxyl-3-methylglutaryl coenzyme A reductase (HMG-CoA Reductase) inhibitors. Statins competitively inhibit HMG-CoA reductase, which limits the rate of cholesterol synthesis (primarily in the liver). As a result, statins break down LDL, decrease the synthesis of VLDL, and increase HDL. Through this mechanism, statins can reduce the amount of plaque that forms in the arteries (see Atherosclerosis for more information).[2]
- Statins may also inhibit many of the structural and functional components of the arteriosclerotic process. Structural effects include reductions in vascular smooth muscle hypertrophy and proliferation, fibrin deposition, and collagen cross-linking. Among the functional effects are improvements in endothelial function, vasodilation due to increased nitric oxide production, reduction in inflammatory cytokines and reactive oxygen species, and down-regulation of angiotensin II and endothelin receptors.[3]
There are several different types of statins. The main difference between them is their potency.
Uses[edit | edit source]
Clinicians use statin medications for the treatment of:
- Hypercholesterolemia
- Hyperlipoproteinemia
- Hypertriglyceridemia
- Hyperlipidemia
- Atherosclerosis
- Myocardial infarction prophylaxis
- Stroke prophylaxis [1] [2]
Brief Literature Review[edit | edit source]
- A 2019 systematic review and network meta-analysis compared the benefits and harms of statins in secondary prevention for patients with ischemic stroke. The resultant conclusion suggests statins are no better than placebo in preventing all strokes and all-cause mortality, but reduce the risk of recurrent ischemic strokes and other cardiovascular events if a patient had a previous stroke or transient ischemic attack.[4]
- A 2018 systematic review with meta-analysis suggests that more intensive pharmacotherapeutic LDL-C lowering (via statin dosage) was associated with a greater reduction in risk of total and cardiovascular mortality compared to less intensive LDL-C lowering. This effect is related to the individual's baseline LDL-C level, as there was no significant difference when LDL-C was less than 100 mg/dL at baseline.[5]
- A 2022 statement from the United States Preventive Task Force recommends the prescription of a statin for the primary prevention of Cardiovascular Disease (CVD) in adults aged 40 to 75 years who have at least 1 CVD risk factor (dyslipidemia, diabetes, hypertension, smoking), and an estimated 10-year CVD risk of 10+%.[6]
Adverse Effects[edit | edit source]
Statins are usually well-tolerated, with myositis, rhabdomyolysis, hepatotoxicity, and diabetes mellitus being the most common adverse reactions.
- Statin-associated muscle symptoms may present as diffuse myalgias or otherwise unexplainable muscle tenderness or weakness. Of all statin-associated muscle symptoms (SAMS), myalgia is the most common, affecting 5-10% of users. These symptoms are generally dose dependent, and resolve upon discontinuation of medication.[7]
- Rhabdomyolysis is the most serious complication of statin use, but its occurrence is rare (current incidence rate of 1 case per 10,000 person-years of treatment after market removal of cerivastatin).[7]
- Statin-associated immune-mediated necrotizing myopathy(IMNM) can occur due to the development of antibodies against the HMG-CoA reductase enzyme. Symmetrical, proximal muscle weakness with significantly increased creatine phosphokinase (CPK) that continues for months after ceasing statins is common in IMNM.[1]
A notable adverse event occurs when consuming grapefruit juice while taking statins. Grapefruit juice increases the systemic concentrations of statins, thus increasing the risk of all side effects, including all SAMS (particularly myalgia), liver damage, and kidney failure.[7]
Smoking cigarettes should also be avoided when taking statins. Smoking decreases the positive effects of statins. Smokers had a 74 to 86 % higher risk of events.[8]
Physiotherapy Implications[edit | edit source]
Statins may increase the incidence of exercise-related muscle complaints and in some studies augment the exercise-induced rise in muscle enzymes, but statins do not consistently reduce muscle strength, endurance, overall exercise performance or physical activity.[9]
When lab values are available, monitoring Creatine Phosphokinase (CK or CPK) can be useful to identify clinical rhabdomyolysis. Although SAMS can occur without an increase in CK, certain health organizations categorize SAMS based on CK elevation.[7] See our page on Rhabdomyolysis and a rhabdomyolysis case study for effective management of patients with this condition.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Sizar O, Khare S, Jamil RT, Talati R. Statin medications. StatPearls [Internet]. 2024. Available from:https://www.ncbi.nlm.nih.gov/books/NBK430940/
- ↑ 2.0 2.1 Bansal AB, Cassagnol M. HMG-CoA Reductase Inhibitors. StatPearls [Internet]. 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542212/
- ↑ Mangat S, Agarwal S, Rosendorff C. Do statins lower blood pressure?. Journal of cardiovascular pharmacology and therapeutics. 2007 Jun;12(2):112-23.Available: https://journals.sagepub.com/doi/abs/10.1177/1074248407300380(accessed 9.4.2022)
- ↑ Tramacere I, Boncoraglio GB, Banzi R, Del Giovane C, Kwag KH, Squizzato A, Moja L. Comparison of statins for secondary prevention in patients with ischemic stroke or transient ischemic attack: a systematic review and network meta-analysis. BMC Med. 2019 Mar 26;17(1):67.
- ↑ Navarese EP, Robinson JG, Kowalewski M, Kolodziejczak M, Andreotti F, Bliden K, Tantry U, Kubica J, Raggi P, Gurbel PA. Association Between Baseline LDL-C Level and Total and Cardiovascular Mortality After LDL-C Lowering: A Systematic Review and Meta-analysis. JAMA. 2018 Apr 17;319(15):1566-1579.
- ↑ US Preventive Services Task Force; Mangione CM, Barry MJ, Nicholson WK, Cabana M, Chelmow D, Coker TR, Davis EM, Donahue KE, Jaén CR, Kubik M, Li L, Ogedegbe G, Pbert L, Ruiz JM, Stevermer J, Wong JB. Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2022 Aug 23;328(8):746-753.
- ↑ 7.0 7.1 7.2 7.3 Thompson PD, Panza G, Zaleski A, Taylor B. Statin-Associated Side Effects. J Am Coll Cardiol. 2016 May 24;67(20):2395-2410.
- ↑ Milionis HJ, Rizos E, Mikhailidis DP. Smoking diminishes the beneficial effect of statins: observations from the landmark trials. Angiology. 2001 Sep;52(9):575-87.
- ↑ Noyes AM, Thompson PD. The effects of statins on exercise and physical activity. Journal of Clinical Lipidology. 2017 Sep 1;11(5):1134-44.