Microcephaly
Original Editor - Ravi Kumar
Top Contributors - Ravi Kumar
Introduction[edit | edit source]
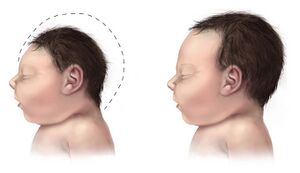
Microcephaly is a rare neurodevelopmental disorder characterized by abnormal smallness of the occipitofrontal head circumference (OFC) in infants compared to other children of the same age and sex[1][2]. The term "Microcephaly" is derived from the Greek words "micros," meaning small, and "kephalē," meaning head[3].
It can be present at birth or may develop in the first few years of life[4]. It often occurs because a baby’s brain has not developed properly during pregnancy or has stopped growing after birth, which results in a smaller head size[2].
Children with microcephaly may have delayed motor functions [5] and speech, facial distortions, dwarfism or low stature, hyperactivity, seizures, issues with coordination and balance,[1] and other brain or neurological abnormalities, depending on the severity of the associated disease.
It is mainly caused by a disturbance in the genetic pathways that develop in the brain early in pregnancy.[6] It can also be caused if the mother is highly exposed to drugs or alcohol[7], becomes infected with a cytomegalovirus,[8] rubella[9], or varicella virus, is exposed to certain toxic chemicals, or has untreated phenylketonuria (PKU)[10].
Prevalence[edit | edit source]
Microcephaly is a rare condition, and its prevalence varies depending on the region and population investigated. The prevalence of microcephaly in Europe was determined to be 1.53 per 10,000 births[11], with substantial variation between registries. The incidence in the United States is estimated to be between 2 and 12 per 10,000 live births[12]. In a Brazilian study, the frequency of microcephaly was reported to be 5.9 per 1000 live births[13]. In another multi-center investigation, the prevalence of microcephaly was reported to be 0.33%. Globally, it affects 1 in every 30,000 to 250,000 births[14].
Etiology[edit | edit source]
The exact causes of microcephaly are unknown[2], but it can result from problems with brain development before or after birth, genetic factors, exposure to drugs or chemicals, and infections during pregnancy[6][7].
The most common causes of microcephaly are genetic abnormalities in certain genes that are associated with brain size growth. Many genes have been termed "MCPH" genes, after the microcephalin genes (MCPH1)[15], because of their function in the development of brain size and in causing primary microcephaly syndromes when mutated. WDR62 (MCPH2), CDK5RAP2 (MCPH3), KNL1 (MCPH4), ASPM (MCPH5), CENPJ (MCPH6), STIL (MCPH7), CEP135 (MCPH8), CEP152 (MCPH9), ZNF335 (MCPH10), PHC1 (MCPH11), and CDK6 are among them (MCPH12)[16].
On the basis of onset, it is classified into two types[18][19].
Congenital microcephaly: It is present at birth or can be visible on an ultrasound within the first 36 weeks of pregnancy.
Postnatal microcephaly: It occurs after birth when the head fails to grow at the expected rate. This is also known as secondary microcephaly, and it can be caused by brain injury in a child.
| CONGENITAL | POSTNATAL |
|---|---|
| Chromosome and/or genetics
Trisomies of 13, 18 and 21 Cornelia de Lange syndrome Cri du Chat syndrome Smith-Lemli-Opitz syndrome |
Chromosome and/or genetics
Inborn errors of metabolism Mitochondrial diseases Aminoacidopathies Defects in glucose transport |
| Aquired
Disruptive traumas Hypoxia or anoxia (insufficient placenta) Death of a twin (monochorionic) |
Aquired
Disruptive traumas Parenchymal hemorrhage (more common in preterm children) Hypoxia or anoxia |
| Infections and protozooses
Toxoplasmosis Cytomegalovirus Herpes simplex Parvovirus B19 Other viruses |
Infections |
| Teratogens/clinical conditions
Alcohol Hydantoin Drugs (cocaine, crack, among others) Maternal diabetes mellitus without adequate control Maternal phenylketonuria |
Toxins
Lead poisoning Chronic renal failure |
| Deprivation
Maternal Folic acid insufficiency Maternal Malnutrition Insufficient placenta |
Deprivation
Congenital cardiopathy |
Signs and symptoms[edit | edit source]
Microcephaly is primarily distinguished by a head size that is significantly smaller than normal for the child's age and gender[21].
Other signs and symptoms
- Delayed development,[22] such as learning to speak, stand, sit, or walk at a later age than other children at a similar stage
- Mearning difficulties
- Movement and balance issues[7]
- High-pitched cry
- Reduced vision from lesions on the retina, the area at the back of the eye
- Distorted facial features and expressions
- Hyperactivity[23]
- Short stature
- Issues with feeding, such as dysphagia, or difficulty swallowing
- Hearing loss
In severe cases, microcephaly may be life-threatening.
Diagnosis[edit | edit source]
Microcephaly requires diagnosis and evaluation to determine the cause and any potential associated conditions. When checking a child with microcephaly, a detailed history and physical examination are important. The history should include questions about the mother's health, including substance use and infections, and any problems at the time of birth. It's also important to know when the microcephaly started, how serious it is, and if there are other family members affected.
An early diagnosis of microcephaly can sometimes be made by detailed fetal ultrasound. Ultrasounds have the best diagnosis possibility if they are made at the end of the second trimester, around 28 weeks, or in the third trimester of pregnancy. Some other diagnostic tests are:
Invasive testing for karyotyping and chromosomal Micro-array[24].
TORCH test for fetal infections[25].
Fetal brain MRI at ≥32 weeks’ gestation for the diagnosis of abnormalities of neuronal migration, such as lissencephaly and polymicrogyria[7][4].
Blood and urine tests.
Role of the Multidisciplinary Team[edit | edit source]
Microcephaly is a lifelong condition, and there is no specific treatment for it. Treatment is symptomatic and supportive. Supportive treatments like occupational therapy, physical therapy , and speech therapy are often used to help children with microcephaly reach their full potential. Treatment for microcephaly depends on the child's condition and may include medications to control seizures or other symptoms, and surgery to correct structural abnormalities in the brain.
Physiotherapy Treatment[edit | edit source]
The physiotherapy treatment can be used as a supportive measure for treating microcephaly. It involves specialized exercises and interventions to improve the motor and developmental abilities of children affected by this condition. The main objective of physiotherapy treatment is to improve physical abilities and promote independence in daily activities, including sitting, standing, walking, and playing. With consistent and targeted physiotherapy, Through consistent and targeted physiotherapy, individuals with microcephaly can make significant progress in achieving their full potential.
Some physiotherapy exercises includes[26]:-
- Strengthening exercises: Strengthening exercises can be used to treat weak muscles, improving the child's function as the muscle will be stronger and have the ability to perform better[27].
- Proprioception exercises: it if performed for awareness of their body.
- Balance and coordination exercises : It help reduce the risks of falls and assist to improve movements such as walking.
References[edit | edit source]
- ↑ 1.0 1.1 Hanzlik E, Gigante J. Microcephaly. Children. 2017 Jun 9;4(6):47.
- ↑ 2.0 2.1 2.2 Asadi S, Jamali M, Valizadeh G, Hosseinpour R. Autosomal Recessive Primary Microcephaly Syndrome.
- ↑ Cox J, Jackson AP, Bond J, Woods CG. What primary microcephaly can tell us about brain growth. Trends in molecular medicine. 2006 Aug 1;12(8):358-66.
- ↑ 4.0 4.1 Passemard S, Kaindl AM, Verloes A. Microcephaly. Handbook of clinical neurology. 2013 Jan 1;111:129-41.
- ↑ Ashwal S, Michelson D, Plawner L, Dobyns WB. Practice parameter: evaluation of the child with microcephaly (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2009 Sep 15;73(11):887-97.
- ↑ 6.0 6.1 Gilmore EC, Walsh CA. Genetic causes of microcephaly and lessons for neuronal development. Wiley Interdisciplinary Reviews: Developmental Biology. 2013 Jul;2(4):461-78.
- ↑ 7.0 7.1 7.2 7.3 Microcephaly [Internet]. [cited 2023 Apr 19]. Available from: https://www.who.int/news-room/fact-sheets/detail/microcephaly
- ↑ Messinger CJ, Lipsitch M, Bateman BT, He M, Huybrechts KF, MacDonald S, Mogun H, Mott K, Hernández-Díaz S. Association between congenital cytomegalovirus and the prevalence at birth of microcephaly in the United States. JAMA pediatrics. 2020 Dec 1;174(12):1159-67.
- ↑ Paller AS, Mancini AJ. Cutaneous Disorders of the Newborn. Hurwitz Clin Pediatr Dermatology. 2016 Jan 1;11-37.e4.
- ↑ Williams RA, Mamotte CD, Burnett JR. Phenylketonuria: an inborn error of phenylalanine metabolism. The Clinical Biochemist Reviews. 2008 Feb;29(1):31.
- ↑ Morris JK, Rankin J, Garne E, Loane M, Greenlees R, Addor MC, Arriola L, Barisic I, Bergman JE, Csaky-Szunyogh M, Dias C. Prevalence of microcephaly in Europe: population based study. bmj. 2016 Sep 13;354.
- ↑ Cragan JD, Isenburg JL, Parker SE, Alverson C1, Meyer RE, Stallings EB, Kirby RS, Lupo PJ, Liu JS, Seagroves A, Ethen MK. Population‐based microcephaly surveillance in the United States, 2009 to 2013: An analysis of potential sources of variation. Birth Defects Research Part A: Clinical and Molecular Teratology. 2016 Nov;106(11):972-82.
- ↑ de Araújo JS, Regis CT, Gomes RG, Tavares TR, Dos Santos CR, Assunção PM, Nóbrega RV, Pinto DD, Bezerra BV, da Silva Mattos S. Microcephaly in north-east Brazil: a retrospective study on neonates born between 2012 and 2015. Bulletin of the World Health Organization. 2016 Nov 11;94(11):835.
- ↑ Microcephaly Epidemiology [Internet]. [cited 2023 Apr 19]. Available from: https://www.news-medical.net/health/Microcephaly-Epidemiology.aspx
- ↑ Pulvers JN, Journiac N, Arai Y, Nardelli J. MCPH1: a window into brain development and evolution. Frontiers in cellular neuroscience. 2015 Mar 27;9:92.
- ↑ Faheem M, Naseer MI, Rasool M, Chaudhary AG, Kumosani TA, Ilyas AM, Pushparaj PN, Ahmed F, Algahtani HA, Al-Qahtani MH, Saleh Jamal H. Molecular genetics of human primary microcephaly: an overview. BMC medical genomics. 2015 Dec;8(1):1-1.
- ↑ Microcephaly | What is the main cause of microcephaly? | What is life expectancy for microcephaly? Available from: https://www.youtube.com/watch?v=9kFh2O6ayj4 [last accessed 16/04/2023]
- ↑ Microcephaly | Johns Hopkins Medicine [Internet]. [cited 2023 Apr 19]. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/microcephaly
- ↑ Duarte G, Moron AF, Timerman A, Fernandes CE, Mariani C, Almeida GL, Werner H, Santo HF, Steibel JA, Bortoletti J, Andrade JB. Zika virus infection in pregnant women and microcephaly. Revista Brasileira de Ginecologia e Obstetrícia. 2017;39:235-48.
- ↑ Joyce T, Gossman W, Huecker MR. Pediatric abusive head trauma.
- ↑ Microcephaly | Johns Hopkins Medicine [Internet]. [cited 2023 Apr 19]. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/microcephaly
- ↑ Aggarwal A, Mittal H, Patil R, Debnath S, Rai A. Clinical profile of children with developmental delay and microcephaly. Journal of neurosciences in rural practice. 2013 Jul;4(03):288-91.
- ↑ Microcephaly: symptoms, diagnosis, support | Raising Children Network [Internet]. [cited 2023 Apr 19]. Available from: https://raisingchildren.net.au/guides/a-z-health-reference/microcephaly
- ↑ Wapner RJ, Martin CL, Levy B, Ballif BC, Eng CM, Zachary JM, Savage M, Platt LD, Saltzman D, Grobman WA, Klugman S. Chromosomal microarray versus karyotyping for prenatal diagnosis. New England Journal of Medicine. 2012 Dec 6;367(23):2175-84.
- ↑ Jaan A, Rajnik M. Torch complex. InStatPearls [Internet] 2022 Jul 18. StatPearls Publishing.
- ↑ Amundsen KR, Evensen KA. Physical therapy intervention for a child with congenital Zika virus syndrome: a case report. Child neurology open. 2020 Mar 3;7:2329048X19896190.
- ↑ Physiotherapy treatment for microcephaly | Microcephaly | Neurological disorders. [Internet]. [cited 2023 Apr 19]. Available from: https://www.manchesterneurophysio.co.uk/paediatrics/conditions-we-treat/neurological-disorders/microcephaly/physiotherapy-treatment-for-microcephaly.php