Functional Anatomy of the Hip
Original Editor - Ewa Jaraczewska
Top Contributors - Ewa Jaraczewska, Jess Bell and Kim Jackson
Introduction[edit | edit source]
The hip joint connects the lower extremities with the axial skeleton. The primary function of the hip joint is to provide dynamic support for the body's weight while facilitating force and load transmission from the axial skeleton to the lower extremities to allow mobility. Understanding the anatomy of the hip joint is crucial for diagnosing hip pathology and selecting the most appropriate intervention. This article will discuss the anatomy of the hip joint in detail and provide some examples of hip joint pathology.
Key Terms[edit | edit source]
Axes: lines around which an object rotates. The rotation axis is a line that passes through the centre of mass. There are three axes of rotation: sagittal passing from posterior to anterior, frontal passing from left to right, and vertical passing from inferior to superior. The rotation axes of the foot joints are perpendicular to the cardinal planes. Therefore, motion at these joints results in rotations within three planes. Example: supination involves inversion, internal rotation, and plantarflexion.
Bursae: reduce friction between the moving parts of the body joints. A bursa is a fluid-filled sac. There are four types of bursae: adventitious, subcutaneous, synovial, and sub-muscular.
Capsule: one of the characteristics of the synovial joints. It is a fibrous connective tissue which forms a band that seals the joint space, provides passive and active stability and may even form articular surfaces for the joint. The capsular pattern is "the proportional motion restriction in range of motion during passive exercises due to tightness of the joint capsule."
Closed pack position: the position with the most congruency of the joint surfaces. In this position, joint stability increases. For example, the closed pack position for the interphalangeal joints is full extension.
Degrees of freedom: the direction of joint movement or rotation; there is a maximum of six degrees of freedom, including three translations and three rotations.
Ligament: fibrous connective tissue that holds the bones together.
Open (loose) pack position: position with the least joint congruency where joint stability is reduced.
Planes of movement: describe how the body moves. Up and down movements (flexion/extension) occur in the sagittal plane. Sideway movements (abduction/adduction) occur in the frontal plane. The transverse plane movements are rotational (internal and external rotation).
Hip Structure[edit | edit source]
The head of the femur and the acetabulum of the pelvis make up the hip joint.
Head of the Femur[edit | edit source]
The femoral head is located at the proximal aspect of the femoral bone, which connects distally to the tibia and the fibula. The neck of the femur supports the rounded head of the femur. The femoral head points in a medial, superior, and slightly anterior direction.
The angle of inclination is the angle between the long axes of the femoral neck and the femoral shaft. In adults, the angle of inclination is normally between 120 and 125 degrees. An angle greater than 125 degrees is called coxa valga, whereas an angle less than 120 degrees is called coxa vara.
The surface of the head of femur is covered with cartilage, except for the area known as the fovea capitis femoris. This fovea, or medial depression, is the attachment point for the ligamentum teres.
There are two bony protrusions at the proximal end of the femur: the greater and lesser trochanters. They serve as attachment points for the muscles responsible for hip and knee movements. The femoral head connects to the femur via the femoral neck, which extends to the femoral shaft.
At the epiphyses of the femoral bone, there is a supportive, connective tissue element called the trabeculae. The growth of the trabeculae follows the lines of stress along the bone. Wolff's law explains the formation of the trabecular pattern:
Wolff's law: a living bone will react to the mechanical forces exerted on it. These forces can be static or dynamic, internal or external. Internal forces are dynamic. External forces can be dynamic or static. Gravity is an example of static force. Weight-bearing is considered a dynamic force. The bone will go through a remodelling process when the load is increased. As a result, it becomes stronger and can resist loading.[1]
Acetabulum of the Pelvis[edit | edit source]
The acetabulum is on the anterolateral part of the pelvis.[2] The head of the femur fits into the concave shape of the acetabulum.
The acetabulum is divided into anterior and posterior columns. The anterior column includes the anterior ilium, anterior wall, the anterior dome of the acetabulum, and superior pubic ramus. The posterior column consists of the greater and lesser sciatic notches, the posterior wall, the posterior dome of the acetabulum, and the ischial tuberosity.[2]
The superior and posterior walls of the acetabulum are angulated, which results in acetabular anteversion and abduction. The face of the acetabulum has an average of 20.7 degrees of anteversion and 39.8 degrees of abduction. The anterior portion of the acetabulum is flat, while the posterior portion is angled with its highest point at the sciatic notch.[3]
The acetabular margin almost forms a circle, but there is a depression on the anteroinferior aspect, which is called the acetabular notch. The transverse ligament of the hip closes the circle at this notch. The acetabular labrum attaches to the margin of the acetabulum. This increases the articular area of the acetabulum, so that more than 50% of the femoral head can fit into the acetabulum.[2]
Labrum[edit | edit source]
The labrum forms a fibrocartilagenous extension of the bony acetabulum. As mentioned above, this anatomical structure allows more than 50% of the femoral head to fit into the acetabulum.[2]
The labrum mostly contains type 1 collagen. It lines the acetabular socket and attaches to the bony rim of the acetabulum.[4] It has three surfaces:
- internal articular surface
- external articular surface
- basal surface
The majority of the labrum is avascular (around two-thirds). The obturator, superior gluteal and inferior gluteal arteries supply the part of the labrum that is vascularised. The superior and inferior portions of the labrum are believed to be the most innervated areas, containing free nerve endings and nerve sensory end organs.[5]
Bones and Articulations of the Hip[edit | edit source]
| Bones | Articulations | Characteristic | Key palpation |
|---|---|---|---|
| Femur
Pelvis |
Femoroacetabular joint | The joint between the femoral head and the acetabulum. The acetabular labrum is a fibrocartilaginous ring that lines the rim of the acetabular socket. It deepens the hip socket and limits extreme ranges of motion. Structurally, the anterior portion of the labrum is the thinnest and most vulnerable to injury. | The acetabulum of the hip bone, and the head and neck of the femur are NOT palpable |
Hip Kinematics[edit | edit source]
There are variations in descriptions of hip kinematics in the literature. Factors that may explain these variations include ethnic origin, types of sports activities performed by high-level athletes, age and testing position, particularly for hip rotation. Examples include:
- Types of sports activities performed by high-level athletes: increased hip external rotation range of motion in professional baseball pitchers.[6]
- Age: reduced total hip rotation range of motion in older persons may be explained by repetitive micro-traumas.[7]
- Testing position: significant difference in external rotation in the prone position vs sitting position. However, no difference was found when testing internal rotation.[8]
| Joint | Type of joint | Plane of Movement | Motion | Kinematics | Closed pack position | Open pack position |
|---|---|---|---|---|---|---|
| Femoroacetabular joint | Ball and socket | Saggital
Frontal Transverse |
Flexion/extension
Abduction/adduction Internal/external rotation (IR/ER) |
Normal range of motion for the adult hip at rest:[9]
flexion/extension: 140°/30° (113-140°/9-30°)[10] adduction/abduction: 25°/50° (28-31°/39-48)[10] internal/external rotation: Hip IR/ER can be dependent upon the angle of hip flexion at which it is measured (0 vs 90 degrees of hip flexion):[11] 45°/50° (32-47°/33-60°)[10] |
Full extension of the hip, some internal rotation and abduction | Flexion, abduction, and external rotation.
In the hip joint, the open-pack position, rather than the closed-packed position, is the position of optimal articular contact. Flexion and external rotation tend to uncoil the ligaments and make them slack. |
Hip Bursae[edit | edit source]
There are a number of bursae located near the hip joint. Two major bursae are the greater trochanteric bursa, which covers the greater trochanter, and the iliopectineal (iliopsoas) bursa, which is located beneath the musculotendinous portion of the iliopsoas muscle.
In addition, the following bursae can be found in or near the hip joint:
- subgluteus medius bursa: between the tendon of gluteus medius and the lateral facet
- subgluteus minimus bursa: between the gluteus minimus tendon and the anterior facet of the femur
- gluteofemoral bursa: at the lateral aspect of the hip, below the iliotibial band
- obturator externus bursa: at the posteroinferior aspect of the hip joint
- obturator internus bursa: between the obturator internus tendon and the posterior surface of the ischium
- ischiogluteal bursa: at the inferior portion of the gluteus maximus muscle, posteroinferior to the ischial tuberosity
You can learn about lateral hip pain associated with trochanteric bursitis here.
Hip Joint Capsule[edit | edit source]
The hip joint capsule significantly contributes to joint stability.[12] The capsule is thinner posteroinferiorly and thicker anterosuperiorly where the predominant weight-bearing stresses occur.
Ligaments of the Hip[edit | edit source]
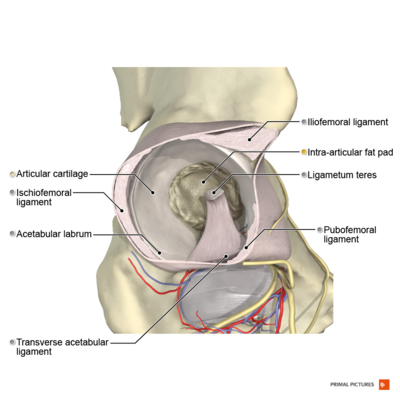
The ligaments that reinforce the hip include intracapsular ligaments, which are located within the joint capsule, and capsular ligaments, which blend with the joint capsule.
Intracapsular Ligaments[edit | edit source]
| Key Ligaments | Origin | Insertion | Action/Role | Key Palpation |
|---|---|---|---|---|
| Ligamentum teres femoris (Femoral head ligament) | Peripheral inferior acetabular notch | The fovea of the femoral head | Carrying small vessels and nerves to the femoral head.
Provides proprioception and structural stability to the hip joint by limiting abduction and external rotation when flexing the hip. |
The acetabulum of the hip bone, and the head and neck of the femur are NOT palpable |
| Transverse acetabular ligament (Tunstall’s ligament) | Wide attachment at the bony region of the posterior horn | Joins the two ends of the acetabular labrum
Forms a complete ring |
Transforms the acetabular notch into a foramen.
Prevents inferior displacement of the head of the femur. Channels nerves and vessels into the joint.[13] |
Capsular Ligaments[edit | edit source]
| Key Ligaments | Origin | Insertion | Action/Role | Key Palpation |
|---|---|---|---|---|
| Pubofemoral ligament | Superior pubic ramus | Intertrochanteric line | Limits excessive abduction and extension | To palpate the superior pubic ramus, position the patient in supine and locate start the anterior superior iliac crest (ASIS). Follow your hands down along the inguinal ligament, which connects to the pubic bone at the pubic tubercle. The superior pubic ramus is located below the inguinal ligament. |
| Iliofemoral ligament | Inferior portion of the anterior inferior iliac spine | Intertrochanteric line of the femur | Prevents hyperextension | To palpate the anterior inferior iliac spine, position the patient in supine and locate the ASIS. Follow your hands from the top of the iliac crest all the way to the front. To confirm that you are palpating the ASIS, ask the patient to lift their leg off the table to activate the sartorius muscle. From the ASIS, move your fingers two finger pads down to locate the anterior inferior iliac spine (AIIS) |
| Ischiofemoral ligament | Posterior acetabular rim | Anterior aspect of the femur | Limits extension and internal rotation |
Passive Range of Motion of the Hip[edit | edit source]
Passive range of motion describes how far a joint can be moved by an external force (e.g. another person) when the surrounding muscles are relaxed.
Passive range of hip flexion
- The patient is in supine lying.
- With one hand, the therapist palpates the anterior superior iliac spine on the tested side and monitors the movement of the pelvis during hip flexion. The clinician must stop the hip movement once the patient's pelvis moves.
- The therapist holds the distal femur with their other hand while the patient's lower leg rests on their forearm.
- The therapist moves the patient's leg into flexion.
Passive range of hip extension
- The patient is in prone lying.
- With one hand, the therapist stabilises the pelvis and watches for pelvis compensatory movements during passive hip extension.
- With their other hand, the clinician holds onto the distal femur and moves the patient's leg into extension.
Passive range of hip abduction
- The patient is in supine lying.
- The therapist palpates the ipsilateral anterior superior iliac spine with one hand to monitor for movement of the pelvis.
- The clinician supports the patient’s leg on their other forearm and passively abducts the patient's hip.
Passive range of hip adduction
- The patient is in supine.
- The patient's non-tested leg is abducted.
- The therapist palpates the contralateral anterior superior iliac spine with one hand to monitor for movement of the pelvis.
- The clinician supports the patient’s leg on their other forearm and passively adducts the patient's hip.
Passive range of hip external rotation
- The patient is in supine.
- The patient’s leg is supported by the clinician's forearm. The clinicians holds the patient's leg in hip and knee flexion.
- The therapist cups the patient's knee with their hand to protect it against varus torque.
- The therapist performs passive hip external rotation.
Passive range of hip internal rotation
- The patient is in supine.
- The patient’s leg is supported by the clinician's forearm. The clinicians holds the patient's leg in hip and knee flexion.
- The therapist cups the patient's knee with their hand to protect it against valgus torque.
- The therapist performs passive hip internal rotation.
Muscles of the Hip[edit | edit source]
Muscles of the hip joint can be grouped based on their function relative to the movements of the hip or based on the fascial compartments they belong to.
- Grouped based on function: e.g. hip flexors, extensors, abductors, adductors, and external and internal rotators
- Grouped based on fascial compartments of the thigh: e.g. gluteal, anterior, medial, and posterior compartments
- gluteal compartment contains: gluteus maximus, medius, and gluteus minimus
- anterior compartment contains: pectineus, sartorius, and rectus femoris
- medial compartment contains: hip adductor muscles and gracilis
- posterior compartment contains: biceps femoris, semimembranosus and semitendinosus muscles
The following tables describe the muscles of the hip joint based on their function relative to movements of the hip.
Hip Flexors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Pectineus | Pectineal line of the pubic bone (superior pubic ramus) | Pectineal line of the femur
Linea aspera of femur |
Anterior part: Femoral nerve (L2, L3);
Posterior part: Accessory obturator nerve (L3, L4) |
Hip flexion and adduction.
An important stabiliser of the pelvis. |
| Iliopsoas:
Iliacus (I) Psoas major (PM) |
I: Iliac fossa
PM: Vertebral bodies of T12-L4, intervertebral discs between T12-L4, transverse processes of L1-L5 vertebrae |
I: Lesser trochanter of femur
PM: Lesser trochanter of femur |
I: Femoral nerve (L1-L3)
PM: Anterior rami of spinal nerves L1-L3 |
I: Main flexor of the hip joint.
Contributes to lateral flexion of the trunk. PM: Hip flexion, hip external rotation, lateral flexion of the trunk. |
| Rectus femoris | Anterior inferior iliac spine
Supraacetabular groove |
Tibial tuberosity (via the patellar ligament) | Femoral nerve (L2-L4) | Hip flexion - active during the swing phase of gait.[14] |
| Tensor fasciae latae (TFL) | Outer lip of anterior iliac crest
Anterior superior iliac spine (ASIS) |
Lateral condyle of tibia (via iliotibial tract) | Superior gluteal nerve (L4-S1) | Weak hip flexor, abductor and
internal rotator. Contributes to pelvic stability during stance and gait. |
| Sartorius | Anterior superior iliac spine (ASIS) | Proximal end of the tibia below the medial condyle (via pes anserinus) | Femoral nerve (L2-L3) | Hip flexion, hip abduction, hip external rotation. |
| Adductor magnus:
Adductor part (AP) Hamstrings part (HP) |
AP: Inferior pubic ramus, ischial ramus
HP: Ischial tuberosity |
AP: Gluteal tuberosity, the medial lip of linea aspera, medial supracondylar line
HP: Adductor tubercle of femur |
AP: Obturator nerve (L2-L4)
HP: Tibial division of sciatic nerve (L4) |
AP: Hip flexion, adduction, and external rotation.
Assists with stabilisation of the pelvis. HP: Hip extension and internal rotation. Assists with pelvis stabilisation. |
Hip Extensors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Adductor magnus:
Adductor part (AP) Hamstrings part (HP) |
AP: Inferior pubic ramus, ischial ramus
HP: Ischial tuberosity |
AP: Gluteal tuberosity, the medial lip of linea aspera, medial supracondylar line
HP: Adductor tubercle of femur |
AP: Obturator nerve (L2-L4)
HP: Tibial division of sciatic nerve (L4) |
AP: Hip adduction, flexion,and external rotation.
Assists with stabilisation of the pelvis. HP: Hip extension and internal rotation. Assists with pelvis stabilisation. |
| Biceps femoris (long head) | Ischial tuberosity Sacrotuberous ligament | Head of fibula (lateral border) | Tibial part of the sciatic nerve (L5-S2) | Hip extension, hip external rotation. |
| Semimembranosus | Ischial tuberosity, superior to the semitendinosus and biceps femoris | Medial tibial condyle | Tibial part of the sciatic nerve | Hip extension, hip and knee internal rotation. |
| Semitendinosus | Ischial tuberosity of the pelvis | Medial surface of the tibia, via pes anserinus | Tibial part of the sciatic nerve | Hip extension, hip and knee internal rotation. |
| Gluteus maximus | Lateroposterior surface of sacrum and coccyx
The gluteal surface of ilium Thoracolumbar fascia Sacrotuberous ligament |
Iliotibial tract
Femoral gluteal tuberosity |
Inferior gluteal nerve (L5, S1, S2) | Hip extension and external rotation.
The superior portion assists with hip abduction. The inferior portion assists with hip adduction. |
Hip Abductors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Gluteus minimus | Gluteal surface of the ilium (between anterior and inferior gluteal lines) | Anterior aspect of greater trochanter of femur | Superior gluteal nerve (L4-S1) | Hip internal rotation and abduction.
An important stabiliser of the pelvis during gait. |
| Gluteus medius | Gluteal surface of the ilium (between anterior and posterior gluteal lines) | Lateral aspect of greater trochanter of femur | Superior gluteal nerve (L4-S1) | Hip abduction and internal rotation (anterior part).
Stabilises the pelvis during standing or walking. |
| Tensor fasciae latae | Outer lip of anterior iliac crest
Anterior superior iliac spine (ASIS) |
Lateral condyle of tibia (via iliotibial tract) | Superior gluteal nerve (L4-S1) | Weak hip flexor, abductor and internal rotator.
Contributes to pelvic stability during stance and gait. |
Hip Adductors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Adductor Magnus: Adductor part (AP)
Hamstring part (HP) |
AP: Inferior pubic ramus, ischial ramus
HP: Ischial tuberosity |
AP: Gluteal tuberosity, the medial lip of linea aspera, medial supracondylar line
HP: Adductor tubercle of femur |
AP: Obturator nerve (L2-L4)
HP: Tibial division of sciatic nerve (L4) |
AP: Hip flexion, adduction, and external rotation.
Assists with stabilisation of the pelvis. HP: Hip extension and internal rotation. Assists with stabilisation of the pelvis. |
| Adductor brevis | Anterior body of pubis Inferior pubic ramus | Medial lip of linea aspera of femur | Obturator nerve (L2-L4) | Weak hip adductor.
Assists with hip flexion, internal and external rotation. Assists with stabilisation of the pelvis in standing or walking. |
| Pectineus | Pectineal line of the pubic bone (superior pubic ramus) | Pectineal line of the femur
Linea aspera of femur |
Anterior part: Femoral nerve (L2, L3)
Posterior part: Accessory obturator nerve (L3, L4) |
Hip flexion and adduction.
An important stabiliser of the pelvis. |
| Adductor longus | Body of pubis
(inferior to the pubic crest and lateral to the pubic symphysis) |
The medial lip of the middle third of the linea aspera of the femur | Obturator nerve (L2-L4) | Main hip adductor. |
| Gracilis | Anterior body of pubis
Inferior pubic ramus Ischial ramus |
Medial surface of the proximal tibia (via pes anserinus) | Obturator nerve (L2-L3) | The most superficial and the weakest hip adductor. |
Hip External Rotators[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Piriformis | The anterior surface of the sacrum
The gluteal surface of the ilium Sacrotuberous ligament |
Greater trochanter of the femur | Nerve to piriformis (S1-S2) | Hip external rotation.
Stabilises the hip joint. |
| Superior gemellus | Ischial spine | Medial surface of greater trochanter of femur | Nerve to obturator internus (L5-S1) | Stabilises the hip joint.
Externally rotates and abducts the hip. |
| Obturator internus | The posterior surface of the obturator membrane
Bony boundaries of the obturator foramen |
Medial surface of greater trochanter of femur | Nerve to obturator internus (L5 and S1) | Hip external rotation with hip joint in extension.
Hip abduction with hip joint in flexion. Stabilises the hip joint. |
| Inferior gemellus | Ischial tuberosity | Medial surface of greater trochanter of femur | Nerve to quadratus femoris (L4/5, S1) | Hip external rotation, hip abduction (when the hip is flexed).
Stabilises the head of the femur in the acetabulum. |
| Obturator externus | The anterior surface of obturator membrane
Bony boundaries of obturator foramen |
Trochanteric fossa of femur | Obturator nerve (L3, L4) | Hip external rotation (when the hip is neutral and flexed). |
| Quadratus femoris | Ischial tuberosity | Intertrochanteric crest of femur | Nerve to quadratus femoris (L4-S1) | Hip external rotation.
Stabilises the head of the femur in the acetabulum. |
| Gluteus maximus | Lateroposterior surface of sacrum and coccyx
The gluteal surface of ilium Thoracolumbar fascia Sacrotuberous ligament |
Iliotibial tract
Femoral gluteal tuberosity |
Inferior gluteal nerve (L5, S1, S2) | Hip extension and external rotation.
The superior portion assists with hip abduction. The inferior portion assists with hip adduction. |
| Adductor longus | Body of pubis
(inferior to the pubic crest and lateral to the pubic symphysis) |
The medial lip of the middle third of the linea aspera of the femur | Obturator nerve (L2-L4) | Main hip adductor.
Participates in hip external rotation and flexion of the thigh. |
| Adductor magnus:
Adductor part (AP) Hamstring part (HP) |
AP:Inferior pubic ramus, ischial ramusHP: Ischial tuberosity | AP:Gluteal tuberosity, the medial lip of linea aspera, medial supracondylar lineHP: Adductor tubercle of femur | AP: Obturator nerve (L2-L4)HP: Adductor tubercle of femur | AP: Hip flexion, adduction, and external rotation.
Assists with stabilisation of the pelvis. *The adductor magnus muscle is an external rotator by those fibres inserted into the medial edge of the linea aspera. The fibres attached to the adductor tubercle assist with internal rotation. [15] HP: Hip extension and internal rotation. Assists with stabilisation of the pelvis. |
Hip Internal Rotators[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Adductor magnus:
Adductor part (AP) Hamstring part (HP) |
AP: Inferior pubic ramus, ischial ramus
HP: Ischial tuberosity |
AP: Gluteal tuberosity, the medial lip of linea aspera, medial supracondylar line
HP: Adductor tubercle of femur |
AP: Obturator nerve (L2-L4)
HP: Tibial division of sciatic nerve (L4) |
AP: Hip flexion, adduction, and external rotation.
Assists with stabilisation of the pelvis. HP: Hip extension and internal rotation. Assists with stabilisation of the pelvis. *The adductor magnus muscle is an external rotator by those fibres inserted into the medial edge of the linea aspera. The fibres attached to the adductor tubercle (HP) assist with internal rotation. [15] |
| Adductor brevis | Anterior body of pubis
Inferior pubic ramus |
Medial lip of linea aspera of femur | Obturator nerve (L2-L4) | Weak hip adductor.
Assists with hip flexion and internal and external rotation. Assists with stabilisation of the pelvis in standing or walking. |
| Gluteus minimus | Gluteal surface of the ilium (between anterior and inferior gluteal lines) | Anterior aspect of greater trochanter of femur | Superior gluteal nerve (L4-S1) | Hip internal rotation and abduction.
An important stabiliser of the pelvis during gait. |
| Gluteus medius | Gluteal surface of the ilium (between anterior and posterior gluteal lines) | Lateral aspect of greater trochanter of femur | Superior gluteal nerve (L4-S1) | Hip abduction and internal rotation (anterior part).
Stabilises the pelvis during standing or walking. |
| Tensor fasciae latae | Outer lip of anterior iliac crest
Anterior superior iliac spine (ASIS) |
Lateral condyle of tibia (via iliotibial tract) | Superior gluteal nerve (L4-S1) | The weak hip flexor, abductor and
internal rotator. Contributes to pelvic stability during stance and gait. |
Innervation of the Hip[edit | edit source]
The hip joint receives innervation from the femoral nerve and the sciatic nerve. In addition, the femoral nerve, obturator nerve, and the nerve to the quadratus femoris provide innervation to the anterior and posterior capsule of the hip joint.[16]
| Nerve | Origin | Branches | Motor fibres | Sensory fibres |
|---|---|---|---|---|
| Femoral nerve | Lumbar plexus L2-L4 | The anterior (superficial) femoral nerve
The posterior (deep) femoral nerve, which becomes the saphenous nerve |
Pectineus, iliacus, sartorius, rectus femoris | The anteromedial thigh,
the medial side of the leg |
| Obturator nerve | Nerve roots L2-L4 | Anterior branch
Posterior branch |
Obturator externus, adductor longus, adductor brevis, adductor magnus (except its hamstring portion) and gracilis | The skin of the medial thigh |
| Sciatic nerve | Nerve roots L4-S3 | Tibial nerve
Common fibular nerve |
Biceps femoris, semimembranosus and semitendinosus, and the hamstring portion of the adductor magnus | No direct sensory functions, but indirect sensory functions include the skin of the lateral leg |
| Superior gluteal nerve | Sacral plexus L4–S1 | Superior branch
Inferior branch |
Gluteus medius muscle, gluteus minimus muscle, and tensor fasciae latae muscle | The skin over the gluteus maximus muscle |
Vascular Supply of the Hip[edit | edit source]
The vascular supply of the hip joint comes from the superior gluteal artery, obturator artery, and the medial and lateral circumflex femoral arteries.
| Artery | Origin | Branches | Supply |
|---|---|---|---|
| Superior gluteal artery | Internal iliac artery | Superficial branch
Deep branch |
Piriformis, obturator internus, ileum, gluteus maximus, gluteus medius, gluteus minimus, skin over sacrum, hip joint, tensor fasciae latae |
| Obturator artery | Internal iliac artery | Anterior branch
Posterior branch |
Femoral head, obturator externus muscle, hip adductors |
| Medial circumflex femoral artery | External iliac artery | Ascending branch
Descending branch Transverse branch Superficial branch Deep branch Acetabular branch |
Thigh adductors, gracilis muscle, obturator externus muscle, hamstring muscles, sciatic nerve, the neck and head of the femur |
| Lateral circumflex femoral artery | External iliac artery | Ascending branch
Descending branch Transverse branch |
Hip joint, femoral head, femoral neck and greater trochanter of femur, quadriceps femoris, tensor fasciae latae, and skin over the anterolateral thigh.
Contributes to the vascular supply of sartorius and gluteal region. |
Relevant Clinical Conditions[edit | edit source]
- Individuals with femoroacetabular impingement (FAI) syndrome present with hip adduction, flexion, and extension weakness, as well as reduced hip internal and external rotation range of motion.[17] You can learn more about FAI syndrome here.
- During total hip arthroplasty, surgeons may preserve the hip joint capsule to may help preserve "the defences of the native hip against hypermobility, impingement, subluxation, and edge-loading."[18]
- “Pseudo-sciatica” is caused by gluteal nerve entrapment between the piriformis and gluteus medius muscle.[19]
- Groin pain on palpation of the adductor tendons, swelling or a lump in the adductor muscle or muscles, stiffness in the groin area or an inability to contract or stretch the adductors may indicate adductor tendinopathy. You can read more about this condition here.
- Severe lateral hip pain with marked palpation tenderness over the greater trochanter may be a symptom of gluteal tendinopathy (or Greater Trochanter Pain Syndrome (GTPS), a condition that can limit a patient's ability to stand, walk, use stairs or run). You can learn more about diagnostic procedures and management strategies for gluteal tendinopathy here. In addition, this Tendinopathy Rehabilitation course discusses the fundamentals of rehabilitation and the four stages of tendinopathy rehabilitation.
Resources[edit | edit source]
- Wichman D, Rasio JP, Looney A, Nho SJ. Physical Examination of the Hip. Sports Health. 2021 Mar;13(2):149-153.
- Hip Examination
- Byrd JW. Evaluation of the hip: history and physical examination. N Am J Sports Phys Ther. 2007 Nov;2(4):231-40.
References[edit | edit source]
- ↑ Shetty A, Hacking C. Trabecular pattern of the proximal femur [Internet]. Radiopaedia.org. 2020. Available from: https://radiopaedia.org/articles/trabecular-pattern-of-proximal-femur [last access 5.05.2023]
- ↑ 2.0 2.1 2.2 2.3 Bannai M, Rock P. Acetabulum. Reference article. Radiopaedia.org. Available at https://radiopaedia.org/articles/acetabulum (last access 9.05.2023).
- ↑ Krebs V, Incavo SJ, Shields WH. The anatomy of the acetabulum: what is normal? Clin Orthop Relat Res. 2009 Apr;467(4):868-75. doi: 10.1007/s11999-008-0317-1. Epub 2008 Jul 22.
- ↑ Gao G, Fu Q, Wu R, Liu R, Ao Y, Xu Y. The correlation between the labrum size and the labral tear in asymptomatic volunteers and symptomatic patients. Journal of Orthopaedic Surgery and Research. 2021 Dec;16(1):1-6.
- ↑ Groh MM, Herrera J. A comprehensive review of hip labral tears. Current reviews in musculoskeletal medicine 2009;2(2):105-17.
- ↑ Ellenbecker TS, Ellenbecker GA, Roetert EP, Silva RT, Keuter G, Sperling F. Descriptive profile of hip rotation range of motion in elite tennis players and professional baseball pitchers. Am J Sports Med. 2007 Aug;35(8):1371-6.
- ↑ Roach KE, Miles TP. Normal hip and knee active range of motion: the relationship to age. Phys Ther. 1991 Sep;71(9):656-65.
- ↑ Simoneau GG, Hoenig KJ, Lepley JE, Papanek PE. Influence of hip position and gender on active hip internal and external rotation. J Orthop Sports Phys Ther. 1998 Sep;28(3):158-64.
- ↑ Huffaker SJ, T-Y Tsai, Rubash HE, Li G, Kwon Y-M. Kinematics of the Hip. Available from https://musculoskeletalkey.com/kinematics-of-the-hip/ [last access 11.05.2023]
- ↑ 10.0 10.1 10.2 Svenningsen S, Terjesen T, Auflem M, Berg V. Hip motion related to age and sex. Acta Orthop Scand. 1989 Feb;60(1):97-100.
- ↑ Cannon A, Finn K, Yan Z. COMPARISON OF HIP INTERNAL AND EXTERNAL ROTATION BETWEEN INTERCOLLEGIATE DISTANCE RUNNERS AND NON-RUNNING COLLEGE STUDENTS. Int J Sports Phys Ther. 2018 Dec;13(6):956-962.
- ↑ Levangie P, Norkin C. Joint structure and function: A comprehensive analysis. 4th ed. Philadelphia: The F.A. Davis Company; 2005.
- ↑ Ng KCG, Jeffers JRT, Beaulé PE. Hip Joint Capsular Anatomy, Mechanics, and Surgical Management. J Bone Joint Surg Am. 2019 Dec 4;101(23):2141-2151.
- ↑ Frigo CA, Wyss C, Brunner R. The Effects of the Rectus Femoris Muscle on Knee and Foot Kinematics during the Swing Phase of Normal Walking. Applied Sciences. 2020; 10(21):7881.
- ↑ 15.0 15.1 Reimann R, Sodia F, Klug F. Die umstrittene Rotationswirkung ausgewählter Muskeln im Hüftgelenk [Controversial rotation function of certain muscles in the hip joint]. Ann Anat. 1996 Aug;178(4):353-9. German.
- ↑ Laumonerie P, Dalmas Y, Tibbo ME, Robert S, Durant T, Caste T, Vialla T, Tiercelin J, Gracia G, Chaynes P. Sensory Innervation of the Hip Joint and Referred Pain: A Systematic Review of the Literature. Pain Med. 2021 May 21;22(5):1149-1157.
- ↑ Frasson VB, Vaz MA, Morales AB, Torresan A, Telöken MA, Gusmão PDF, Crestani MV, Baroni BM. Hip muscle weakness and reduced joint range of motion in patients with femoroacetabular impingement syndrome: a case-control study. Braz J Phys Ther. 2020 Jan-Feb;24(1):39-45.
- ↑ Tamaki Y, Goto T, Wada K, Hamada D, Tsuruo Y, Sairyo K. Anatomic evaluation of the insertional footprints of the iliofemoral and ischiofemoral ligaments: a cadaveric study. BMC Musculoskelet Disord. 2020 Dec 9;21(1):828.
- ↑ Koh E. Imaging of peripheral nerve causes of chronic buttock pain and sciatica. Clin Radiol. 2021 Aug;76(8):626.e1-626.e11.