Proximal Hamstring Tendinopathy
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (31 May 2024)
Description[edit | edit source]
Proximal hamstring tendinopathy (PHT) is commonly seen in long distance runners and athletes taking part in sprinting or hurdles. It is also common among athletes taking part in sports such as football and hockey, which involves change of direction activities.(Frederichson et al) Proximal hamstring tendinopathy is also referred to as hamstring origin tendinopathy or high hamstring tendinopathy. It can also affect people who do not participate in sport (de Jesus et al; Lempainen et al). It is characterised by deep, localised pain in the region of the ischial tuberosity.(Goom et al) Pain is usually worse during or after activities such as running, lunging, squatting and sitting.(Goom et al)This condition can include tendon degeneration, partial tearing and peritendinous inflammatory reactions.[1] Proximal Hamstring Tendinopathy-related Sciatic Nerve Entrapment (PHTrSNE) is a neuropathy caused by fibrosis interposed between the semimembranosus tendon and the sciatic nerve, at the level of the ischial tuberosity.
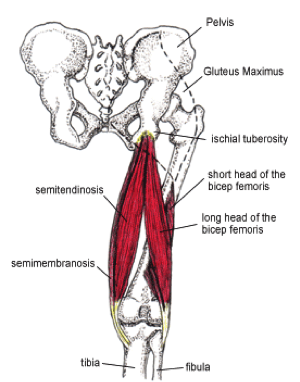
Clinically Relevant Anatomy[edit | edit source]
One of the most important muscle groups in running is the hamstrings muscle group. The hamstrings are active at various stages in the gait cycle, particularly in knee flexion and hip extension. The hamstrings muscles share a common origin on the lateral aspect of the ischial tuberosity. Semitendinosus and the long head of biceps femoris share a conjoined tendon originating from the lateral facet. (Goom et al). The origin of Semimembranosus is deeper (Phillippon et al, 2014). Various locations of hamstring tendon pathology have been reported. The semimembranosus is one of the most commonly affected parts of the hamstring muscles in proximal hamstring tendinopathy (Lempainen et al (50)) Other studies found a variety of locations such as the common hamstring tendon, biceps femoris, semimembranosus and semitendinosus (Benazzo et al)
The junction between the tendons of the hamstrings and the ischial tuberosity is the area affected by high hamstring tendinopathy. The tendon’s thickness, fibrousness and poor blood supply are the causes of difficult healing.[2]. The muscles contain a higher proportion of type 2 muscle fibers than the other muscles of the lower extremity; suggesting high intrinsic force generation.
During running, the hamstrings have three main functions. First, they decelerate knee extension at the end of the forward swing phase of the gait cycle. Through an eccentric contraction, the hamstrings decelerate the forward momentum (ie, leg swing) at approximately 30° short of full knee extension. This action helps provide dynamic stabilization to the weight bearing knee. Second, at foot strike, the hamstrings elongate to facilitate hip extension through an eccentric contraction, thus further stabilizing the leg for weight bearing. Third, the hamstrings assist the gastrocnemius in paradoxically extending the knee during the takeoff phase of the running cycle.[3]
Proximal hamstring tendinopathy is regarded as an insertional tendinopathy(Goom et al). Compression of the tendon at its attachment during hip flexion/adduction is hypothesized to be an important etiological factor (Cook and Purdham), but the evidence is limited. Other contributing factors may be the presence of a shearing force between the hamstring attachment and the ischial tuberosity (Hamming et al) and the increased displacement of the proximal hamstring tendon with an increased hip flexion angle (Harvey et al)
(For extra information about pathology mechanisms see Tendinopathy)
Functional Anatomy[edit | edit source]
Proximal hamstring tendinopathy (PHT) rehabilitation requires a good understanding of hamstring muscle function (Goom et al). In athletes, upright running may be an aggravating factor. During upright running, the function of the hamstrings is to eccentrically decelerate the knee in terminal swing phase. Peak forces are reported in the late swing phase, and a second peak is reported in the early stance phase (Goom, 19, 36) Another contributing factor to proximal hamstring overuse injuries is the storage of energy in the late swing to early stance stretch-shortening cycle. Eccentric to concentric transition is linked to higher hamstring loads (Goom, 81) The storage of elastic energy in tendons and aponeuroses have been shown to increase the efficiency of locomotion. (Goom et al 3) With greater hip and trunk flexion, as in running with the trunk leaning forward, or with over-striding as well as uphill running, the proximal hamstring is subjected to higher energy storage loads.(Goom t al). Considering these functional requirements, certain suggestions have been made to to improve muscle hypertrophy, strength and length-tension differences as well as facilitate the return to sport. These suggestions include eccentric type of rehabilitation exercises as well as strech-shorten exercises.(56, 8, 90)
Epidemiology / Etiology[edit | edit source]
With tendinopathy there is a a multitude of factors that can contribute to the etiology. These factors are usually load related. Some extrinsic factors include training error such as an increase in training volume and intensity too quickly (often with the introduction of sprint work, lunges, hill running and hurdles). These type of training errors have been reported in the research as training errors preceding PHT. (43, 97) With these type of activities, the hamstring needs to contract or lengthen when the hip is in flexion. This can lead to a higher tensile and compressive load at the tendon insertion (30,88). Another cause of symptoms may be excessive static stretching, ie in yoga or Pilates. These type of exercises involve sustained end range hip flexion postures (Goom et al) Long periods of sitting can also be a cause in some patients (49)
Risk Factors:[edit | edit source]
Intrinsic factors:
- Malalignments
- Leg length discrepancy
- Imbalance
- Decreased flexibility
- Joint laxity
- Female gender
- Age - Reduction in muscle fiber size and number are associated with advancing in age, this leads to losses of mass and strength.[4]
- Overweight
- Proprioceptive deficiency[5]
- Ischial tuberosity tenderness
- Core weakness[6]
- Pelvic dysfunction[6]
- Previous injury - the strength is reduced by previous hamstrings, knee or groin injuries.[4]
- Neuromyofascial involvement- increased neural tension and posterior thigh pain due to myofascial trigger points; often associated with decreased flexibility.[4]
- Hip stiffness
- Tightness/Weakness of the hamstrings and quadriceps
- Poor lumbopelvic/core stability.[7]
- History of another lower extremity injury - previous injury to the other lower limb, or injuries to other muscles or tendons in the same lower limb.[8]
- Sciatic nerve irritation.
Extrinsic factors:
- Excessive, repetitive overloads and over training.
- Poor training
- Environmental conditions
- Poor equipment
- Insufficient warm up - A warm-up with isometric contractions increases strength and length of the muscle.[4] A study found an association between hamstrings injuries and lack of stretch prior to sports participation.[4]
- Fatigue - causes decline in muscle energy, decreased concentration and coordination and poor technique.[4]
Intrinsic and Extrinsic factors contribute to the formation of injury.[2]
The tendinopathy usually starts with micro-damage without a remarkable trauma. Normally the tendon is capable to intrinsic repair itself, meaning that the consequences of this injury are little. Sometimes, an imbalance can cause further damage and failed healing. All of this leads to the formation of tendinopathy.
Clinical Picture[edit | edit source]
- Subjectively typical tendon pain behaviour (localised ischial tuberosity pain that becomes less symptomatic after a few minutes of activity, but is worse afterwards (Goome et al)
- Deep buttock pain and pain in the posterior thigh.
- The pain is often felt on the lower gluteal region, radiating along the hamstings[6].
- Provocative activities include activities requiring deeper hip flexion i.e. squats, lunging. long periods of sitting (especially on harder surfaces) (Goome et al)
- The pain increases with repetitive activities (such as long-distance running).In some cases pain flares with sitting or driving.
- Rarely painful with activities such as slow walking on level surface, standing and lying as these type of activities do not involve energy storage or compression (Goome et al)
- Occasional stiffness in the morning may be present or when starting to move after period of prolonged rest (Goome et al)
- The onset is mostly gradual, not with acute trauma.[9].
- Continued exercises and stretching can cause even more pain[3].
Pain down the back of the thigh can be caused by irritation of the sciatic nerve. This nerve passes very close to the ischial tuberosity.[2] Due to its degenerative nature, this injury is classified as a tendinopathy rather than a tendonitis, an inflammatory pathology.[1]
Differential Diagnosis[edit | edit source]
- First of all, it’s essential to determine if the pain is local or referred. Referred pain is characterized by complaints of pain in various locations. Pain in the buttock combined with pain in the lower back may refer to the lumbar spine. This may be caused by muscles, ligaments or discs dysfunctions.
- Localized constant pain in the buttock, around the ischial tuberosity could be triggered by hamstring origin tendinopathy or ischiogluteal bursitis.
- If the patient complains of pain higher up (upper gluteal region) there might be a problem with the piriformis muscle.
- Pain over the sacrum or near the sacroiliac joint refers to a pelvic stress fracture or inflammation or malalignment of the sacroiliac joint.
- There are also some uncommon cases where buttock and posterior thigh pain refer to chronic compartment syndrome of the posterior thigh. Due to the resemblance of some symptoms of this injury with other hip injuries, it’s important to get a proper diagnosis; this will likely entail a physical examination and an MRI.[3]
- Sciatic nerve irritation at piriformis muscle or near the ischial tuberosity (Goom et al)
- Ischiofemoral impingement
- Unfused ischial growth plate in a post-adolescent athlete
- Apophysitis or avulsion fracture among adolescents
- Deep gluteal muscle tear
- Posterior pubic or ischial ramus stress fracture
- Partial or complete rupture of the proximal hamstring tendon
Diagnostic Procedures[edit | edit source]
Imaging[edit | edit source]
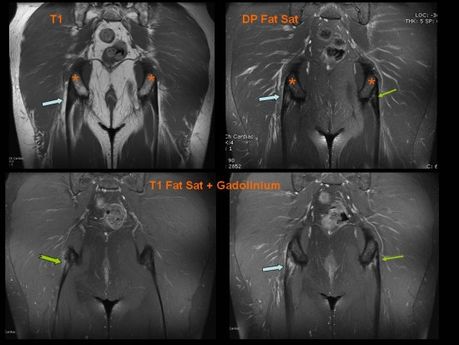
MRI is required to confirm the diagnosis and to take a look at the severity of the injury. MRI can detect tendon thickening, tearing, inflammation and swelling at the ischial tuberosity.
Ultrasound is also used, but this technique isn’t able to give a precise visualization of bone marrow edema.[10] Normally a high hamstring injury may be combined with stress reaction or bone edema in the ischial tuberosity and findings of the tendon. In case of a tendinopathy, an increased signal is noticeable on T1-weighted images with no abnormalities on fat-suppressed T2-weighted images.[3][1]
A series of provocation tests have been developed in order to help for the diagnosis of this injury.
Passive Stretch Tests[edit | edit source]
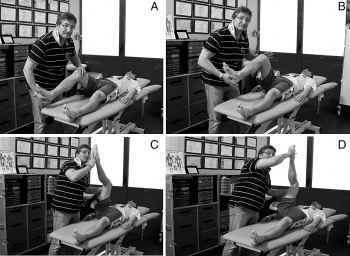
The bent-knee stretch, the modified bent-knee stretch and the Puraven-Orava test are used as passive stretch tests in the diagnosis of PHT. These tests have moderate to high validity and high sensitivity and specificity for the diagnosis of PHT (Goom et al , 15).
Bent-knee stretch test:[edit | edit source]
The test is performed while the patient is lying on his back. The hip and knee are maximally flexed. Slowly the therapist will straighten the knee till its maximally extended; the hip must remain in a 90° flexion. The test is also doable without the assistance of a therapist. The patient can use a rope or a belt to straighten his knee like depicted on the picture.
Modified bent-knee stretch test[edit | edit source]
The test is performed while the patient is lying on his back, the hip and knee are in extension. The therapist takes the heel in one hand and holds the knee with the other hand. He brings the hip and knee in maximal flexion and then rapidly straightens the knee.
These tests are used to identify a hamstrings origin tendinopathy, but do not replace an MRI.[2]
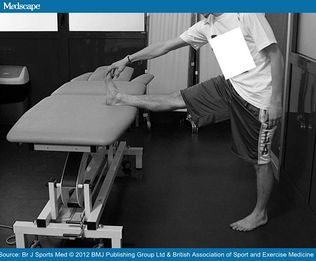
The Puranen-Orava test[edit | edit source]
The Puranen-Orava test is a standing test that actively stretches the hamstring when the hip is flexed to 90 degrees and the knee is extended fully and the foot is on a support 90 degrees to the standing body
Goom et al reports that in their clinical experience, these tests may be negative in less symptomatic cases, It is also important to consider other clinical conditions that may be present and responsible for the symptoms. The use of MRI in diagnosis of PHT is recommended. (Goom et al 15).
Furthermore, the pain response to palpation vary and may have low specificity in the diagnosis of tendinopathies (Goom, 24)
Palpation of the ischial tuberosity[edit | edit source]
Higher quality research studies are needed to investigate the use of special tests in the diagnosis of hamstring injuries(Goom 74). The lack of high quality evidence reiterates the importance of combining various tests results with a comprehensive and detailed history to determine tendon pain behaviour in diagnosing proximal hamstring tendinopathy (Goom et al).
Loading Tests[edit | edit source]
The reproduction of pain with various loading tests can aid in the diagnosis of proximal hamstring tendinopathy (PHT), but the accuracy of these tests still needs to be investigated more extensively. The principle is to reproduce pain by loading the proximal hamstring tendons. This is done by progressively increasing the compressive and tensile load, by increasing the angle of hip flexion.(Goom et al, 26)
An example of a load test assessment for patients with proximal hamstring tendinopathy may consist of progression from the single leg bent knee bridge (low load clinical test) to the long lever bridge (moderate load) and arabesque movements to single leg deadlift (high-load clinical test) (Goom, 26). The movements are initiated slowly at first, and only adding speed if patient is asymptomatic. The pain score should increase with the load across all these tests. (Goom)
Higher quality research are needed to investigate the clinical use of special tests in the diagnosis of hamstring injuries(Goom, 74). It remains essential to combine test results with a comprehensive and detailed history to determine tendon behaviour in diagnosing proximal hamstring tendinopathy (Goom).
Prevention
- Good flexibility of the hamstring and quadriceps muscles must be maintained for the prevention of this injury.
- Some preventative techniques related to sport techniques are to avoid block drills in the beginning of the season or on two consecutive days.[10]
Physical Therapy Management[edit | edit source]
During rehabilitation, patients may experience pain. Pain provocation after energy storage activities is acceptable, provided that the pain does not last longer than 24 hours (Goom, 45, 85). Pain provocation lasting longer than 24 hours can be classified as "irritable". Pain that settles within 24 hours of energy storage loading can be classified as "stable" (54). After the initial warm-up (pain becoming less after a few minutes of activity), stable tendon pain may return towards or afterwards the activity.(Goom)
Load modification as part of Symptom Management[edit | edit source]
Training load management or modification is essential in the management of tendon related pain, even more so in patients with irritable symptoms. It is advisable to limit pain producing compressive and energy storage load activities (i.e. increased hip flexion) until the pain irritability settles to stable pain. Stable pain is mild (VAS 0 to 3 out of 10) and usually settles with 24 hours of moderate to high tendon load interventions (e.g. repeated lunging). Determine subjectively what activities increase the patients' symptoms and the time frame (for how long?). This will help the clinician determine the irritability level as well as what type of load management strategy will be effective. Often the patient will be able to continue with certain activities such as steady state running within the pain/aggrevation guidelines. More compressive and energy storage activities such as hill running, quick starts and hurdles should be avoided initially and only implemented at later stages. (Goom)
In tendinopathy rehabilitation research there are varying outcomes in the different tendons. In Achilles tendinopathy rehabilitation it has been reported that continuing sport activities did not lead to worse outcomes compared to stopping sport activities in the first 6 weeks of rehabilitation.(84) This is in contrast to patellar tendinopathy though. (95) Patients or runners with PHT may often report certain distances that they are able to run without any symptoms or report activities where symptoms is only present during certain types of training(e.g. squats). If symptoms persists for longer than 24 hours after activity, despite partial load management, it is advisable to stop with the aggravating activities. If symptoms are really reactive and irritable, it is best to stop with all painful compression and energy storage activities until the symptoms settle and become stable.(Goom)
Aggravating sporting activities may be replaced with cross-training to maintain cardiovascular fitness, or these activities can be adapted to reduce the load. Examples of such activities are:
- Cycling may be better tolerated if patient is performing it standing
- Swimming and water running are good options
- Posture modification may reduce symptoms (e.g. reduce hamstring origin compression by reducing anterior pelvic tilt and hip flexion in standing)
- When sitting is symptomatic, shaped cushions are useful to reduce the compression. It allows for more weight bearing on the posterior thigh rather than the ischium
- Avoid repeated stretching of the hamstrings in the early, reactive phase
- Avoid hip flexion dominant movements such as trunk flexion and repeated lifting in the early, reactive stages
Rehabilitation[edit | edit source]
Load management is the key to tendinopathy management. Progressive loading, performed within a pain-monitoring framework, is essential to reduce pain and ultimately restore function. (Goom)Rehabilitation should incorporate the whole kinetic chain. (23)
Exercise prescription[edit | edit source]
Goom et al recommends the following rehabilitation stages in proximal hamstring tendinopathy, based on the current evidence available.
In general the following should apply:
- Resistance training principles should be applied to ensure optimal loading, contraction speed and time under tension (Goom, 1)
- Monitor pain at the same time on a daily basis with a load test during rehabilitation (Goom)
- Some pain is allowed during and after exercise (Stable pain - VAS 0 to 3 out of 10) (45)
- Symptoms should settle within 24 hours
- Symptoms should not progressively worsen over the course of the loading program (84)
- Treat every patient individually and focus on particular phases of rehabilitation or kinetic chain factors specific to the individual (Goom)
- Progression through the exercise stages should be based on the symptoms and the response when progressing the exercise load and not on specific time frames
- The 4 stage program may take 3 -6 months to complete, but variation will most likely be present.
Stage 1 Isometric hamstring load[edit | edit source]
Isometric exercises in positions without tendon compression is proposed as an effective method of loading the muscle tendon unit as well as reduce pain in proximal hamstring tendinopathy with irritable symptoms (26). It has been reported that isometric exercises have a pain inhibitory response (64)It is recommended that the isometric exercises should be repeated several times per day. (22). Symptom severity and irritability is used to determine the dosage. The dosage can be adjusted to shorter/less intense contractions or vice versa based on the symptoms.
In the early stages of proximal hamstring tendinopathy (PHT) the position of the hip should be near neutral hip flexion-extension or in minimal hip flexion (20°- 30° for straight leg pull downs). (Goom). A favorable sign for isometric hamstring loading is an immediate reduction in pain with hamstring loading tests after exercise. (Goom)
Appropriate exercises for stage I rehabilitation (Goom)
- Isometric leg curl
- Bridge holds - hip in neutral
- Isometric straight leg pull downs
- Trunk extensions
- Isometric long leg bridging on two, progressing to one leg holds
Stage 2 Isotonic hamstring load with minimal hip flexion (Goom)
Important aspects of proximal hamstring tendinopathy rehabilitation is
- to restore hamstring strength (83)
- to restore hamstring muscle bulk and capacity in a functional range of movement(83)
Isotonic hamstring loading may be started when there is minimal or no pain (VAS 0 -3 out of 10) during hamstring loading in early ranges of hip flexion. Although eccentric exercises are widely accepted as the treatment of choice for tendinopathies (12), there is not sufficient evidence for isolating the eccentric component (53). ThereforE, Heavy Slow Resistance training (HSR) is advocated. Heavy Slow Resistance training includes eccentric and concentric elements. It has also been shown to compare favourably with isolated eccentric loading in tendinopathy rehabilitation (12, 13, 45)
With HSR, the aim is to perform slow fatiguing resisted isotonic exercise. Commence with 15RM (the maximum load that can be lifted 15 times in a single set) and progress to 8 RM. Perform 3-4 sets every second/other day (1) Hold contractions for 3 seconds for each phase of the exercise (concentric and eccentric)(45).
Minimise loaded hip flexion
to in the early stages. This is advised to protect the enthesis against too much compression (25). It is important to concentrate on single leg work to address assymetrical strength loss. Continue with stage 1 isometric exercises on the "off" days. This will help with symptom (pain) management, especially if there are still symptoms present.
Appropriate exercises for stage 2
- Single leg bridge
- prone hip extension
- prone leg curl
- Nordic hamstring exercise
- Bridging progressions
- Supine leg curl
Stage 3 Isotonic exercises in increased hip flexion (70 - 90)
The aim of rehabilitation in this stage is
- to continue with hamstring muscle strengthening in greater hip flexion
- to continue with muscle hypertrophy in greater hip flexion
- to continue with functional training in greater hip flexion
Once there is minimal pain or no pain (VAS 0 - 3 out of 10) with higher loading hip flexion tests such as lunging and arebesques, the isotonic strengthening in increased hip flexion can be implemented. The dosage and frequency of exercises remain the same as in stage 2. Technique is important and exercises should be performed slow and controlled. The progression into greater hip flexion often cause pain and irritability and is important to monitor the 24 hour response post exercise with loading tests into hip flexion (hamstring bridge, deadlift, single leg arebesque) 26
Appropriate exercises for stage 3
- slow hip thrusts
- forward step-ups
- walking lunges
- deadlifts
- Romanian deadlifts
At the end of phase 3, patients with PHT should be able to load the proximal hamstring comfortably through sport-specific ranges with little aggravation of symptoms.(Goom)
Stage 4 Energy storage loading
This stage is only necessary for patients and athletes returning to sports that involves lower limb energy storage or impact loading. Introduction of power/elastic stimulus for the myotendinous unit can start when there is minimal pain during load tests (VAS 0-3 out of 10). It is also essential to have adequate bilateral strength in single leg exercises from stage 2 and 3. Good movement control is also needed. In the early phase of stage 4 it is advised to limit the amount of hip flexion, to protect the proximal hamstring tendon from compression. Note that this is the most provocative stage in the rehabilitation process and a conservative approach is needed for dosage and frequency of the exercises prescribed. Start with performing exercises only every third day. Follow with a stage 1 day, to settle the tendon. The following day will then include strengthening exercises from stage 2-3. This adds up to a 3 day high-low-medium tendon load cycle, twice a week, with a rest day between cycles (78).
Appropriate exercises for stage 4
- Sprinter leg curl
- A-skips
- Fast sled push or pull
- Alternate leg split squats
- Bounding
- Stair or hill bounding
- Kettle bell swings
- Lateral, rotational cutting movements
Return to sport
Return to sport can be gradually introduced when the athlete is able to cope with the loading requirements of the sport with minimal symptom aggravation (i.e. VAS 0 -3 of 10 with pain settling within 24 hours on load tests). The exercise progressions form stepping stones for return to sport, but it is important to not just add these exercises to the normal training volume on resumption, as this can lead to overloading and aggravation of symptoms (95). Be careful with the introduction of hill training as well as speed training sessions, as these can easily exacerbate symptoms. In team sports, there may be more complex loading requirements. This needs more detailed assessment and a graded return to sport will usually consist of a gradual exposure to activity prior to return to full competition.
Other Physical Therapy management considerations
- Limited evidence is available on the effectiveness of dry needling and soft tissue techniques in the treatment of PTH, but supporting evidence is available in published case series (43,60, 97)
- Massage and manual therapy can be useful in PHT when these are used to address tone and restriction in the kinetic chain (Goom)
- Take note that these passive interventions will not improve tissue load capacity, which is the key element of tendinopathy rehabilitation (Goom, 23)
Medical Management
- Anti-inflammatory drugs..[2]
- Corticosteroid injection -In more severe cases, when physical therapy does not help, a corticosteroid injection into the peritendinous soft tissues is recommended in combination with physical therapy. Injecting the substance in the tendon itself can be dangerous. Frederickson et al. found that patients whose MRIs showed more swelling around the tuberositas ischiadicum and less thickening of the tendon got more relief from a cortisone injection than patients with more pronounced tendon thickening. However, corticosteroid injections can also have a negative impact on the tendons inter alia the weakening of tendons, the rupture of tendons, particularly in load-bearing tendons (Kleinman M. et al, 1983)
- Platelet-rich plasma injection-A novel treatment is platelet-rich plasma injection at the origin of the muscle.[2] Platelet-rich plasma (PRP) seems to be a promising alternative to the corticosteroid injections. The alpha and dense granulates that are present in the platelets, release multiple growth factors and cytokines that promote wound healing (Alsousou J. et al, 2009 Mishra A. et al, 2009). An enhancement of the recruitment, proliferation and differentiation of the cells involved in soft-tissue regeneration has been reported by the authors of in vitro studies (Hall MP et al, 2009, De Mos M. et al, 2008)
- Shockwave therapy-The shockwave therapy has almost no influence on hamstrings origin tendinopathies.[1]
When conservative treatment fails, patient may need surgery to decrease the pressure on the nerve and to divide the fibrous and damaged tendon.[4]
- Patient should starts treatment as early as possible. The earlier the rehabilitation, the faster he/she will return to previous normal function.
- Therapy takes from weeks to months depending on the condition and the history of previous injuries.[7]
- Controlling the pain is one of the important therapy goals, this is possible through ice, electrical stimulation of the tendon and pulsed ultrasound.
- Correction of pelvis misalignment has to be taken into consideration, as it might increase the tension on the hamstring muscles,and affects muscle strength. Anterior pelvic tilt is the most common misalignment and it could be easily corrected by manual or chiropractic manipulation.
- Soft-tissue mobilization has to be included in the rehabilitation program. It’s very beneficial to break up the adhesions and scar tissues. A friction treatment with transverse frictions is commonly used. The therapist has to pay attention to not compress directly on the ischial tuberosity as it can irritate underlying edema. Techniques like ART (Active Release Technique) or Gastron can be included as well.
- At the same time the patient may start a gradual stretching program for the hamstrings. starting with double-leg non weight bearing isometric exercises followed by single-leg closed-chain isometric and isotonic open-chain exercises.
- Eccentric muscle strengthening program is a good treatment program for tendinopathies , as it can normalize the thickness and structure of the tendon. It can also prepare the hamstrings for the high-force load while running.
- Core strength is a considerable element for the rehabilitation of hamstring origin tendinopathy as it reduces the risk of recurrent hamstring strains..
- If the ROM of the muscle is normal and pain-free, pool running and stationary biking could be put into the rehabilitation program.[12][9][3][4][13][14]
- Stretching of both legs is crucial for balance. Even the antagonist hip flexor muscles should be stretched for an optimal function.
- ROM can be increased by the use of ultrasound or shockwave therapy before stretching. Frequent stretching may avoid a recurrence of the injury.
Running again:
- High hamstring tendinopathy is known as a disease that takes a long time to recover from. Fredericson et al. estimates a recovery of 8-12 weeks. It’s likely that cross training doesn’t stress the legs until the bent-knee stretch test can be done without pain.
When exercises becomes pain free, the following return-to-running program could be initiated:
Week 1: Walk 5min/jog 1min, build to sets on alternating days (ex. 2x5min/1min, off, 3x5min/1min, off, ect)
Week 2: If no pain, walk 5min/jog 5min, build to 5 sets on alternating days
Week 3: If no pain, advance to 20min jog, no more than 5 days per week
Week 4: If no pain, advance to 20min run at normal training pace, no more than 5 days per week
Week 5-8: If no pain, gradually increase running speed, volume, and acceleration as tolareted[2]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Maurice H. Zissen, et al. High Hamstring Tendinopathy: MRI and Ultrasound Imaging and Therapeutic Efficacy of Percutaneous Coorticosteroid Injection [Internet]. American Roentgen Ray Society 2010. Level of evidence 2B, grades of recommendation B
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 High hamstring tendinopathy injuries – Signs, symptoms and research-backed treatment solutions for a literal pain in the butt. Available from: http://runnersconnect.net/running-injury-prevention/high-hamstring-tendinopathy-injuries-a-pain-in-the-butt/
- ↑ 3.0 3.1 3.2 3.3 3.4 Michael Fredericson, et al. High Hamstring Tendinopathy in Runners. Meeting the Challenges of Diagnosis, Treatment, and Rehabilitation [Internet]. The Physician and Sportsmedicine 2005. Available from: http://www.agilept.com/downloads/high-hamstring-tendinopathy-in-runners.pdf - Level of evidence 2A, grades of recommendation B
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 P.BRUKNER & K. KAHN, clinical sports medicine, McGraw-Hill, Australia, 2005 (third edition), P388-390
- ↑ White, K. E., High hamstring tendinopathy in 3 female long distance runners. Journal of Chiropractic Medicine 2011, 10 (2), 93-99 Level of evidence 4. grades of recommendation C
- ↑ 6.0 6.1 6.2 Fredericson, M.; Moore, W.; Guillet, M.; Beaulieu, C., High hamstring tendinopathy in runners: Meeting the challanges of diagnosis, treatment, and rehabilitation. Physician and Sportsmedicine 2005, 33 (5), 32-43. Level of evidence 4, grades of recommendation C
- ↑ 7.0 7.1 Tele Demetrious and Brett Harrop. Hamstring Origin Tendonitis. PhysioAdvisor 2008. http://www.physioadvisor.com.au/9628550/hamstring-origin-tendonitis-hamstring-injury-p.htm Level of evidence 5, grades of recommendation D
- ↑ 15
- ↑ 9.0 9.1 Puranen J.; Orava S., The hamstring syndrome. A new diagnosis of gluteal sciatic pain, American Journal of Sports Medicine, 1988, 16(5): 517 – 521. Level of evidence 4, grades of recommendation C
- ↑ 10.0 10.1 McCormack R. J., The management of bilateral high hamstring tendinopathy with ASTYM treatment and eccentric exercise: a case report, The Journal of Manual and Manipulative Therapy, 2012, 20(3) 142 – 146. Level of evidence 4, grades of recommendation C
- ↑ Physiotutors. Bent Knee Stretch Test ⎟ Proximal Hamstring Tightness and Tendinopathy. Available from: https://www.youtube.com/watch?v=Xg0ghED6AS8
- ↑ Reid, D.C., 1992. Sports injury assessment and rehabilitation. USA: Churchill Livingstone Inc. Pp. 415, 417, 554-570. Level of evidence 2A, grades of recommendation B
- ↑ Daniel Lorenz and Michael Reiman. The Role and Implementation of Eccentric Training in Athletic Rehabilitation: Tendinopathy, Hamstring Strains, and ACL Reconstruction [Internet]. Sports Physical Therapy Section 2011. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3105370/?tool=pubmed Level of evidence 2A, grades of recommendation B
- ↑ Mike Walden. Hamstring Origin Tendinitis / Tendinopathy. Sportsinjuryclinic.net 2011 http://www.sportsinjuryclinic.net/cybertherapist/back/buttocks/hamstring_tendinitis.htm Level of evidence 5, grades of recommendation D