Ischial Bursitis
Original Editors - Andrea Nees as part of the Vrije Universiteit Brussel's Evidence-based Practice project
Top Contributors - Kim Jackson, Habibu Salisu Badamasi, Admin, David Olukayode, WikiSysop, Uchechukwu Chukwuemeka and Aminat Abolade
Definition/Description[edit | edit source]
Ischial bursitis, also known as Ischiogluteal bursitis , Weaver’s bottom or Tailor's bottom[1][2] [3] is a rare and infrequently recognized bursitis of the buttock region.[4] It’s one of the four types of hip bursitis. The bursitis is mainly due to chronic and continuous irritation of the bursa and occurs most often in individuals who have a sedentary life.[2][5] The irritation commonly results from prolonged pressure on the ischium, Bursitis always develops in response to another pathology. Therefore, the diagnosis of bursitis must be considered as a secondary happening, the primary condition being another pathology. Ischial bursitis can result from sitting for long periods on a hard surface, from direct trauma to the area, or from injury to the hamstring muscle or tendon through activities such as running or bicycling.
Clinically Relevant Anatomy[edit | edit source]
The Ischial bursa is a deep located bursa over the bony prominence of the Ischium[6] and lies between the Gluteus Maximus and the Ischial tuberosity.[7][5]
Specifically, the bursa located deep:
- On the sagittal section - between the inferior part of the M. Gluteus maximus and posteroinferiorly part of the Ischial tuberosity.
- On the transverse and coronal sections - the superior end of the bursa abutted to the inferomedial surface of the Ischial tuberosity and it lies medial to the common tendon of the hamstrings muscles that has his insertion from the inferolateral surface of the Ischial tuberosity.[5]
- When the bursa is larger, it is possible that it is located in the subcutaneous fat at the ischiorectal fossa, beyond the imaginary line that can be drawn between the medial ends of the gluteus maximus and adductor magnum muscles on the transverse sections.[5]
Etiology[edit | edit source]
The origin of ischial bursitis is apparent in the original name of the condition, "weaver's bottom."[8] The earliest people with this illness were employees who sat for extended amounts of time on hard surfaces. Another vernacular moniker for this ailment is "tailor's bottom."[9] Other common causes of bursitis include:
- Trauma (hemorrhagic bursitis)
- Inflammation (rheumatoid arthritis and spondyloarthropathies),
- Infection (rarely septicemia and septic arthritis ) [3]
- Crystal deposition. There are three basic crystal-induced arthropathies: monosodium urate crystal deposition disease(gout); calcium pyrophosphate dihydrate (CPPD) crystal deposition disease (pseudogout and other clinical presentation); and calcium hydroxy-apatite (HA) crystal deposition disease.
- Cycling, because it involves a lot of gluteus maximus muscle repetition.[9]
Epidemiology[edit | edit source]
Ischial bursitis is a clinical disease that is not very prevalent. Patients of all ages may present with the diagnosis, despite the fact that it is frequently overlooked. Less than 1% of all visits to primary care centers are for bursitis. The term "weaver's bottom" is a colloquial term for this condition since it most frequently affects those with sedentary occupations who spend a lot of time sitting on hard surfaces.[9] People have been affected by this condition for as long as weaving has been a vocation, which dates to around 6000 BCE.[10]
Pathophysiology[edit | edit source]
There are several different types of bursa, including synovial, subcutaneous, submuscular, and adventitious. The ischial bursa is synovial, which means it is made up of a capsule of fatty connective tissue and synovial fluid. The cells of the synovia multiply in response to infection or irritation, increasing the amount of synovial fluid produced. This process is mediated by inflammatory mediators like cytokines, cyclooxygenase, and metalloproteases. The end outcome is a thick cavity filled with fluid and abundant fibrin, resulting in the creation of granulation tissue.[11]This granulation tissue will end up altering the normal activities of other surrounding tissues, like the muscles, tendon, or bone.[9]
Characteristics/Clinical Presentation[edit | edit source]
- Pain in the region of the ischial tuberosity which may also be referred to the lower leg[1] [12]
- Pain is aggravated by prolonged sitting[13]
- Pain with passive hip flexion.[9]
- Pain with stretching, which also causes an inability to extend the hip.[9]
- Tenderness may occur over the ischial tuberosity.[14]
- Inability to sleep on the affected hip.
- Regional muscle dysfunction.[12]
- Swelling and limited mobility.[15]
- Overlying erythema. If erythema forms the major part of the presentation, etiologies such as cellulitis or septic joint are suspected.[9]
Differential Diagnosis[edit | edit source]
Ischial Bursitis can be confused with myoxoid tumors. These are a group of rare tumors showing myoxoid change, including neurofibroma, schwannoma and myoxoma. Therefore it may be necessary to do an incisional or excisional biopsy.[13] By using this technique the doctors take cells out of the injured place and they can histologically differentiate cells from a myoxoid tumor or from Ischial Bursitis. An X-ray also rules out the possibility of a stress fracture or roughening of the cartilage in the hip joint.[7] The pain from ischial bursitis can be differentiated from pain from muscle-related conditions by performing physical examination.[9]
Diagnostic Procedures[edit | edit source]
- MRI: T1 weighted scans show an injury with intermediate intensity[4] [13]. T2 weighted scans show a higher intensity of this lesion, suggesting a space filled with fluid.
- X-Ray[16]
Examination[edit | edit source]
- Pain with straight leg raise test is often present.[14][7][13]
- Active resisted extension of the affected hip reproduces the pain.[14]
- Plain radiographs may reveal calcification of the bursa and associated structures which is consistent with chronic inflammation.[14]
- Examination of patients with ischial bursitis reveals a soft tissue mass in the gluteal region of the affected hip. This soft tissue mass is described as well defined, non-mobile and slightly tender.[4][13]
Medical Management[edit | edit source]
A combination of nonsteroidal anti-inflammatory drugs (NSAIDs) or cyclooxygenase-2 inhibitors and physical therapy. Steroid injections are reserved for patients who do not respond to analgesics. [14]
Physical Therapy Management[edit | edit source]
- Rest: The treatment begins with rest. Rest in the meaning of keep on doing your daily activities and sporting but at a lower intensity. The recommendation is to stay within your pain threshold.
- Cold therapy: Cold therapy contains ice application with cold packs usually for about 20-30 minutes.[19]. This application of cold leads to lowering of the temperature of the skin, subcutaneous tissues and to a lesser degree, deeper tissues like muscle, bone and joint. Cold water, cold gel packs and ethyl chloride or other sprays can be used, depending on the clinical situation.[20]
- Ultrasound therapy ,transcutaneous electrical stimulation and laser can be used for improving the healing process and reducing pain [21][22][23]
- Heat treatment is also possible, with hot packs. It increases blood flow and oxygen tension. The treatment is used twice a day for 30 minutes. Target temperatures range from approximately 38°C to 50°C.[24]
- Frictional massage: It is recommended to use friction massage additional to the therapy on chronic bursitis because it affects the adhesions in chronic bursal problems.[25] It breaks down scar tissue, increases extensibility and mobility of the structure, promotes normal orientation of collagen fibers, increases blood flow, reduces stress levels, and allows healing to take place. Friction massage is beneficial to the underlying structures. [26]By using the Graston technique of friction massage the patient should be forewarned because it may initially aggravate a chronic subacute inflammation that is present. It is postulated that deep friction, especially with the Graston technique instruments, may initiate a new inflammatory cascade, which is necessary to reach the remodelling stage of the inflammatory process and result in healing of the area.[27]
- Therapeutic exercises: should contain stretching exercises to increase the flexibility of tight hamstrings muscle and reducing pressure on the bursa and achieving painless motion and strengthening exercises, to correct muscle imbalances, ease symptoms.[1][28][29] Static stretching is believed to be the safest method because it would have the lowest injury risk. It is most effective when you stretch once a day, 30 seconds for each stretch. [30][31] The benefits of static stretching includes preventing the tissue from absorbing great amounts of energy per unit time, doesn't elicit a forceful reflex contraction and it is good against muscle soreness. [30]
Examples of static stretching exercises: [1]
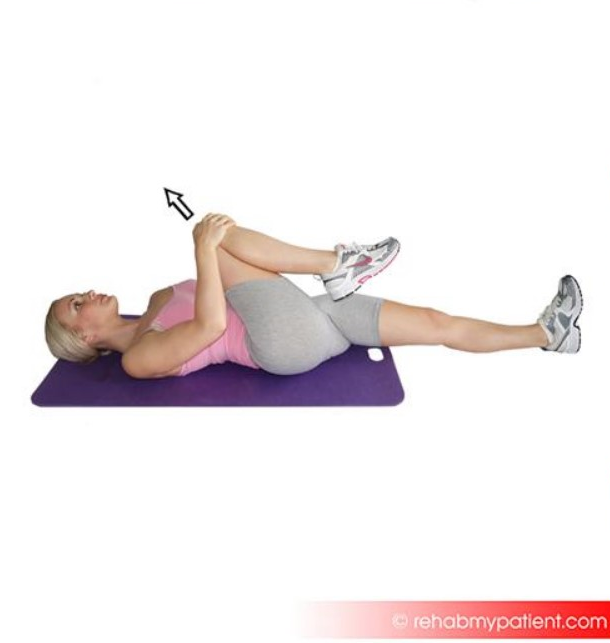
- Gluteus stretch:
Lie on your back and bend your affected knee upward. Grab the back of your knee with both hands and slowly pull the knee toward your chest. Hold this position for 5 to 10 seconds and repeat 6 to 10 times.
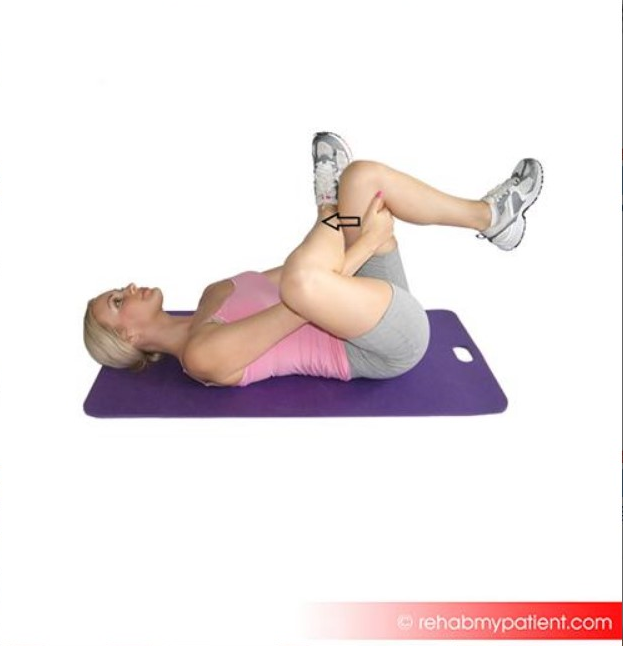
- Piriformis stretch:
While lying on the floor, bend your affected knee and cross the leg over the other leg, placing your foot alongside the knee. Use your hands to pull the good leg in towards you, lifting the leg off the floor. You should feel a stretch in the affected buttock and in your outer thigh. Hold this position for 10-30 seconds.
- Strengthening of the hip rotators is a frequently used rehabilitation program.[12]
- Another program contains strengthening of the hamstrings and gluteal muscles by climbing stairs and reverse curls.[32]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Johnson DB, Varacallo M. Ischial Bursitis. InStatPearls [Internet] 2019 Mar 19. StatPearls Publishing.
- ↑ 2.0 2.1 Kim S, Shin M, Kim K, Ahn J, Cho K, Chang J, Lee S, Chhem R. Imaging features of ischial bursitis with an emphasis on ultrasonography. Skeletal radiology. 2002 Nov 1;31(11):631-6.
- ↑ 3.0 3.1 Johnson DB, Varacallo M. Ischial Bursitis. InStatPearls [Internet] 2020 Mar 15. StatPearls Publishing.
- ↑ 4.0 4.1 4.2 Van Mieghem IM, Boets A, Sciot R, Van Breuseghem I. Ischiogluteal bursitis: an uncommon type of bursitis. Skeletal radiology. 2004 Jul;33(7):413-6.
- ↑ 5.0 5.1 5.2 5.3 Cho KH, Lee SM, Lee YH, Suh KJ, Kim SM, Shin MJ, Jang HW. Non-infectious ischiogluteal bursitis: MRI findings. Korean Journal of Radiology. 2004 Dec 1;5(4):280-6.
- ↑ Zimmermann III B, Mikolich DJ, Ho Jr G. Septic bursitis. InSeminars in arthritis and rheumatism 1995 Jun 1 (Vol. 24, No. 6, pp. 391-410). WB Saunders.
- ↑ 7.0 7.1 7.2 Weiss, L., & al, et al. (2007). Ischial Bursa. In Easy Injections (pp. 92-94). Philadelphia: Elsevier.
- ↑ Chen B, Rispoli L, Stitik T, Leong M. Successful Treatment of Gluteal Pain from Obturator Internus Tendinitis and Bursitis with Ultrasound-Guided Injection. Am J Phys Med Rehabil. 2017 Oct;96(10):e181-e184.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 Johnson DB, Varacallo M. Ischial bursitis. InStatPearls [Internet]. 2023 Jan. StatPearls Publishing.
- ↑ Ekiz T, Biçici V, Hatioglu C, Yalçın S, Cingöz K. Ischial Pain and Sitting Disability Due to Ischiogluteal Bursitis: Visual Vignette. Pain Physician. 2015 Jul-Aug;18(4):E657-8.
- ↑ Navarro-Zarza JE, Villaseñor-Ovies P, Vargas A, Canoso JJ, Chiapas-Gasca K, Hernández-Díaz C, Saavedra MÁ, Kalish RA. Clinical anatomy of the pelvis and hip. Reumatol Clin. 2012 Dec-2013 Jan;8 Suppl 2:33-8.
- ↑ 12.0 12.1 12.2 Paluska SA. An overview of hip injuries in running. Sports medicine. 2005 Nov 1;35(11):991-1014.
- ↑ 13.0 13.1 13.2 13.3 13.4 Hitora, T., & al, et al. (2008). Ischiogluteal bursitis: a report of three cases with MR findings. Rheumatol Int , 455-458.
- ↑ 14.0 14.1 14.2 14.3 14.4 Waldman, S. D. (2012). Ischial Bursitis. In Atlas Of Common Pain Syndromes (pp. 288-290). Philadephia: Elsevier Saunders.
- ↑ Pécina, M. M., & Bojanic, I. (2004). Bursitis. In Overuse injuries of the musculoskeletal system (pp. 305-313). Florida: CRC Press.
- ↑ Ryan, A. J. (1962). Bursitis. In Medical care of the athlete (p. 132). McGraw hill.
- ↑ https://youtu.be/j0_-jkRbZEs
- ↑ Osteo and Physio. Our full 5 minute guided routine for ISCHIAL BURSITIS!. Available from: https://www.youtube.com/watch?v=e8LnMFVsJqM [last accessed 13/6/2021]
- ↑ Cuccurullo, S. (2004). Physical Medicine and Rehabilitation Board Review. New York.
- ↑ Ernst, E., & Fialka, V. (1994, January 1). Ice Freezes pain? A review of the clinical effectiveness of analgesic cold therapy. Journal of Pain and Symptom Management , pp. 56-59.
- ↑ Swam Downing, D., & Weinstein, A. (1986, February). Ultrasound Therapy of Subacromial Bursitis. Physical Therapy. Journal of the American Physical Therapy Association , pp. 194-199.
- ↑ Luck J., L. (n.d.). Musculoskeletal Ultrasound Intervention: Principles and Advances. p. 515-533.
- ↑ Timur Ekiz MD, Vedat Biçici MD, Cem Hatioglu MD, Süha Yalçın MD, Kagan Cingöz MD. Ischial pain and sitting disability due to ischiogluteal bursitis: visual vignette. Pain physician. 2015 Jul;18:E657-9.
- ↑ Badgwell Doherty, C. (2009). Thermotherapy in dermatologic infections. Continuing medical education , 909-927.
- ↑ Hammer, W. (1993). The use of transverse friction massage in the management of chronic bursitis of the hip and shoulder. Journal of Manipulative & physiological therapeutics
- ↑ Premkumar, K. (2004). The massage connection: anatomy and physiology.
- ↑ Hammer, W. I. (2007). Hip Bursitis. In Functional Soft-Tissue Examination and Treatment by Manual Methods (P. 281). Jones and Bartlett Publishers Inc.
- ↑ Thacker, S. B., et al. (2004). The impact of stretching on sports injury risk: a systematic review of the literature. Official journal of the American College of sports medicine , 371-378.
- ↑ Pécina, M. M., & Bojanic, I. (2004). Bursitis. In Overuse injuries of the musculoskeletal system (pp. 305-313). Florida: CRC Press.
- ↑ 30.0 30.1 Brady, W. D., et al. (1998). The effect of static stretch and dynamic range of motion training on the flexibility of the hamstrings muscles. Journal of Orthopaedic & Sporrts Physical Therapy , 295-300.
- ↑ Bandy, W. D. (1997). The effect of time and frequency of static stretching on flexibility of the hamstrings muscles. Physical therapy , 1090-1096.
- ↑ Subotnic, S. (1991). In Conventional, Homeopathic & alternative treatments. Sport & Exercise injuries. (p. 279). California: North Atlantic Books.