Trigeminal Neuralgia
Original Editor - Wendy Walker
Top Contributors - Kirenga Bamurange Liliane, Wendy Walker, Abbey Wright, Admin, Kim Jackson, Scott Buxton, Evan Thomas, Joao Costa, Claire Knott, Laura Ritchie, Naomi O'Reilly, Vanessa Rhule, WikiSysop and Uchechukwu Chukwuemeka
Introduction[edit | edit source]
Trigeminal Neuralgia (TN) is a facial pain syndrome.
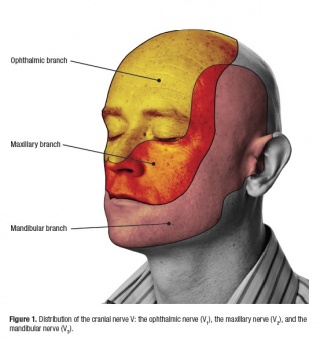
It is typically characterised by short term, unilateral facial pain following the sensory distribution of cranial nerve V, the Trigeminal Nerve. Most commonly the pain radiates to the mandibular or maxillary regions. In some cases, it is accompanied by a brief facial spasm or tic.[1]
Clinically Relevant Anatomy[edit | edit source]
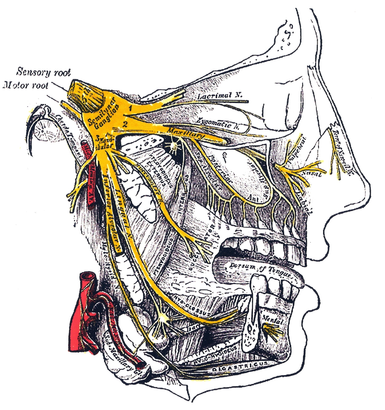
The Trigeminal nerve, the fifth cranial nerve, is the nerve responsible for sensation in the face, and control of motor functions such as biting and chewing.
"Trigeminal" = tri, and "-geminus" or twin, or thrice twinned derives from the fact that it has three major branches:
- Ophthalmic nerve (V1) 1st branch - sensory
- Maxillary nerve (V2) 2nd branch - sensory
- Mandibular nerve (V3) 3rd branch - sensory and motor. Controlling the muscles of mastication: Temporalis and Masseter.
Mechanism of Injury / Pathological Process[edit | edit source]
Symptoms of pain is usually caused by compression of the Trigeminal nerve route in 80-90% of cases.[1] Which is located within the Central Nervous System.
Common causes of compression can be tumours or their associated blood vessels however in many cases the cause can be unknown.[1]
TN can also be a complication of Multiple Sclerosis and other neurological conditions, due to the demyelination of the root entry of the Trigeminal nerve in the pons[1][2].
Epidemiology[edit | edit source]
Recent estimates suggest the prevalence is approximately 4.5 cases per 100,000 population, with an incidence of approximately 15,000 cases per year.[3]
Age[edit | edit source]
In 90% of patients, the disease begins after age 40 years, most often between 60-70 years.[4]
Gender[edit | edit source]
Woman are affected more than men 3:2[4].
Multiple Sclerosis[edit | edit source]
Approximately 1-2% of patients with MS develop TN[5][6]
Clinical Presentation[edit | edit source]
TN presents as a sharp, stabbing unilateral facial pain that is normally episodic in nature. [7]
Area of pain[edit | edit source]
60% of patients with TN present with lancinating pain shooting from the corner of the mouth to the angle of the jaw
30% experience jolts of pain from the upper lip or canine teeth to the eye and eyebrow, sparing the orbit itself—this distribution falls between the division of the first and second portions of the nerve.
According to Patten[8], fewer than 5% of patients experience ophthalmic branch involvement.
Characteristic Descriptors of pain[edit | edit source]
The pain quality is severe, paroxysmal, and lancinating.
It usually starts with a sensation of electrical shocks, then quickly increases in less than 20 seconds to an excruciating pain felt deep in the face, often contorting the patient's expression. The pain then begins to fade within seconds, only to give way to a burning ache lasting seconds to minutes. During attacks, patients may grimace, wince, or make an aversive head movement, as if trying to escape the pain, thus producing an obvious movement, or tic; hence the term "tic douloureux."
Frequency of pain[edit | edit source]
The number of attacks may vary from less than 1 per day, to hundreds per day.
Outbursts fully abate between attacks, even when they are severe and frequent.
Pain Triggers[edit | edit source]
A common feature of TN is that the pain is triggered by touching the painful area of the face, as well as activities such as shaving, rubbing, brushing teeth, moving face to talk, cold wind on the face, etc.
Studies suggest that trigger zones, or areas of increased sensitivity, are present in one half of patients and often lie near the nose or mouth[9].
Diagnosis and Classification[edit | edit source]
The International Headache Society (IHS) have published strict criteria[10] for TN:
A - Paroxysmal attacks of pain lasting from a fraction of a second to 2 minutes, affecting 1 or more divisions of the trigeminal nerve and fulfilling criteria B and C
B - Pain has at least 1 of the following characteristics: (1) intense, sharp, superficial or stabbing; or (2) precipitated from trigger areas or by trigger factors
C - Attacks stereotyped in the individual patient
D - No clinically evident neurologic deficit
E - Not attributed to another disorder
No laboratory, electrophysiologic, or radiologic testing is routinely indicated for the diagnosis of trigeminal neuralgia (TN), as patients with characteristic history and normal neurologic examination may be treated without further investigation.
The diagnosis of TN is almost entirely based on the patient's history and in most cases no specific laboratory tests are needed.
MRI scanning is often indicated simply to exclude other causes of the pain, such as pressure on the trigeminal nerve from Acoustic Neuroma.
Outcome Measures[edit | edit source]
- Visual Analog Scale (VAS)
- McGill Pain Questionnaire (MPQ)
- Brief Pain Inventory (BPI)
- Brief Pain Inventory - Facial (BPI-F)
Management / Interventions[edit | edit source]
Medical Management[edit | edit source]
A range of anti-epileptic drugs have proved to be useful in management of TN, with carbamazepine in particular having a large number of studies demonstrating efficacy[11].
Non anti-epileptic drugs can also be prescribed, often in conjunction with carbamazepine[12].[13]
Surgical Management[edit | edit source]
Studies suggest that approximately 25% of TN patients go on to require surgery as their condition worsens over years, and the drug management becomes less effective[14]. Microvascular decompression and radiofrequency thermorhizotomy are the most common surgical procedures employed in these cases.
Differential Diagnosis[edit | edit source]
The main differential diagnoses for TN are:
- Atypical facial pain - this common facial pain is less intense than TN, described as a dull or throbbing ache which lasts for minutes to hours
- Migraine can cause severe unilateral facial pain
- As can Cluster headaches
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Love S, Coakham HB. Trigeminal neuralgia: pathology and pathogenesis. Brain. 2001;124(12):2347-60.
- ↑ Burchiel KJ. Abnormal impulse generation in focally demyelinated trigeminal roots. Journal of neurosurgery. 1980;53(5):674-83.
- ↑ Katusic S, Williams DB, Beard M, Bergstralh EJ, Kurland LT. Epidemiology and clinical features of idiopathic trigeminal neuralgia and glossopharyngeal neuralgia: similarities and differences, Rochester, Minnesota, 1945-1984. Neuroepidemiology. 1991;10(5-6):276-81.
- ↑ 4.0 4.1 Manzoni GC, Torelli P. Epidemiology of typical and atypical craniofacial neuralgias. Neurological Sciences. 2005 May 1;26(2):s65-7.
- ↑ Rushton JG, Olafson RA. Trigeminal neuralgia associated with multiple sclerosis: report of 35 cases. Archives of neurology. 1965;13(4):383-6.
- ↑ Jensen TS, Rasmussen P, Reske‐Nielsen E. Association of trigeminal neuralgia with multiple sclerosis: clinical and pathological features. Acta Neurologica Scandinavica. 1982;65(3):182-9.
- ↑ Eller JL, Raslan AM, Burchiel KJ. Trigeminal neuralgia: definition and classification. Neurosurgical focus. 2005 May 1;18(5):1-3.
- ↑ Patten J. Trigeminal neuralgia. In: Neurological Differential Diagnosis. 2nd ed. London: Springer;1996:373-5.
- ↑ Sands GH. Pain in the face. Headaches in Adults, Annual Course, American Academy of Neurology Annual Meeting. 1994;3:146:130-2
- ↑ The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24 Suppl 1:9-160
- ↑ Rockliff BW, Davis EH. Controlled sequential trials of carbamazepine in trigeminal neuralgia. Arch Neurol.1966;15(2):129-36
- ↑ He L, Wu B, Zhou M. Non-antiepileptic drugs for trigeminal neuralgia. Cochrane Database Syst Rev. 2006;3:CD004029
- ↑ Cruccu G, Gronseth G, Alksne J, Argoff C, Brainin M, Burchiel K, et al. AAN‐EFNS guidelines on trigeminal neuralgia management. European journal of neurology. 2008;15(10):1013-28.
- ↑ Dalessio DJ. Trigeminal neuralgia. A practical approach to treatment. Drugs.1982;24(3):248-55