Opioid Use Disorder: Difference between revisions
mNo edit summary |
Sonal Joshi (talk | contribs) (Added link to references) |
||
| (17 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editors '''- [[Pathophysiology of Complex Patient Problems|Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> | |||
'''Original Editors '''- [[Pathophysiology of Complex Patient Problems|Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
== Definition/Description == | == Definition/Description == | ||
[[Image:CDC prescription opioids.png|right|250x250px]] | [[Image:CDC prescription opioids.png|right|250x250px]] | ||
Opioid use disorder is | Opioid use disorder is the chronic use of opioids that causes clinically significant distress or impairment. Opioid use disorders affect over 16 million people worldwide and there are over 120,000 deaths worldwide annually attributed to opioids.<ref name=":1">Dydyk AM, Jain NK, Gupta M. [https://www.ncbi.nlm.nih.gov/books/NBK553166/ Opioid use disorder.] InStatPearls [Internet] 2021 Jul 12. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK553166/ (accessed 9.4.2022)</ref> The opioid crisis was declared a nationwide Public Health Emergency in USA on Oct. 27, 2017<ref name=":0">APA Opioid use disorder Available: https://www.psychiatry.org/patients-families/addiction/opioid-use-disorder<nowiki/>(accessed 9.4.20220</ref>. | ||
Opioid use disorder consists of an overpowering desire to use opioids, increased opioid tolerance, and withdrawal syndrome when discontinued. | |||
While opioid use disorder is similar to other substance use disorders in many respects, it has several unique features. Opioids can lead to physical dependence within a short time, as little as 4-8 weeks. In chronic users, the abruptly stopping use of opioids leads to severe symptoms, including generalized pain, chills, cramps, diarrhea, dilated pupils, restlessness, anxiety, nausea, vomiting, insomnia, and very intense cravings. Because these symptoms are severe it creates significant motivation to continue using opioids to prevent withdrawal.<ref name=":1" /> <div> | |||
== Opioids == | |||
[[Image:Drowsiness_opioids.jpg|350x300px|alt=|thumb|Drowsy]][[Opioids]] are natural or synthetic (made in laboratories to mimic the properties of natural opioids) chemicals that interact with opioid receptors on the nerve cells in the body and brain and reduce feelings of [[Pain Behaviours|pain.]] They are a class of drugs that include prescription [[Pain Medications|pain relievers]], synthetic opioids and heroin. Prescription opioids are meant to be used to treat acute pain (such as recovering from injury or post-surgery), [[Chronic Pain and the Brain|chronic pain]], active-phase [[Cancer pain|cancer]] treatment, [[Palliative Care Competence Framework for Physiotherapists|palliative care]] and end-of-life care. The main intended use is to reduce pain perception, but is associated with causing euphoria, drowsiness, mental confusion, nausea, constipation, and depress respiration (high doses) <ref name=":0" /><ref name="p2">Substance Use Disorders. Substance Abuse and Mental Health Services Administration. 2015. Available at: http://www.samhsa.gov/disorders/substance-use. Accessed April 8, 2016.</ref>.<div> | |||
Commonly used opioids identified in the healthcare setting include: | |||
*Codeine | |||
*Fentanyl (patch) | |||
*Hydrocodone (Hysingla ER, Zohydro ER) | |||
*Hydrocodone/Acetaminophen (Lorcet, Lortabe, Norco, Vicodin) | |||
*Hydromorphone (Dilaudid) | |||
*Methadone (Dolophine) | |||
*Morphine (Avinza, Kadian) | |||
*Oxycodone (OxyContin, Roxicodone) | |||
*Oxycodone | |||
*Naloxone <ref name="p1">American Psychiatric Association. Opioid Use Disorder Diagnostic Criteria. http://pcssmat.org/wp-content/uploads/2014/02/5B-DSM-5-Opioid-Use-Disorder-Diagnostic-Criteria.pdf Accessed 07 April 2016.</ref> | |||
== Epidemiology == | |||
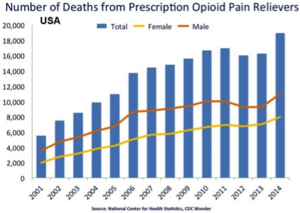
[[File:NID Opioid Deaths.png|thumb|Opioid Deaths]]Over 16 million people worldwide are opioid-dependent and would meet the criteria for opioid use disorder, three million in the USA. Opioid use disorder results in over 120000 and 47000 deaths per year worldwide and in the U.S., respectively<ref name=":1" />. | |||
== Etiology == | |||
There is not one single cause that will lead someone to develop an opioid use disorder. Although, there are several factors that can increase the risk for developing an addiction including both individual and environmental <ref name="p1" />. [[Genetic Conditions and Inheritance|Genetic]] factors have been found to play an important role for predisposition tendencies that can respond to the environment <ref name="p1" />. | |||
< | Opioids are known to activate the [[Limbic System|mesolimbic]] reward system which signals the release of dopamine causing feelings of pleasure. Our [[Brain Anatomy|brain]]<nowiki/>s ability to establish this conditioned association is responsible for the desire to repeatedly use the drug <ref name="p9">Goodman, CC, Snyder, TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. 5th ed. St. Louis, MO: Saunders/Elsevier; 2013. (Pg 49-51)</ref>. However, the body is highly specialized to make adaptations to the presence of the drug and will transition from compulsion of seeking pleasure to depending on the drug existence entirely. Therefore, the increased compulsion is related to an individual tolerance and dependence of the drug <ref name="p9" />. | ||
[[ | == Clinical Presentation == | ||
[[File:Opioid addict.jpeg|thumb|Giving up or reducing activities because of opioid use]]Opioids produce high levels of positive reinforcement, increasing the odds that people will continue using them despite negative resulting consequences. Opioid use disorder is a chronic lifelong disorder, with serious potential consequences including disability, relapses, and death. The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition describes opioid use disorder as a problematic pattern of opioid use leading to problems or distress, with at least two of the following occurring within a 12-month period: | |||
# Taking larger amounts or taking drugs over a longer period than intended. | |||
# Persistent desire or unsuccessful efforts to cut down or control opioid use. | |||
# Spending a great deal of time obtaining or using the opioid or recovering from its effects. | |||
# Craving, or a strong desire or urge to use opioids | |||
# Problems fulfilling obligations at work, school or home. | |||
# Continued opioid use despite having recurring social or interpersonal problems. | |||
# Giving up or reducing activities because of opioid use. | |||
# Using opioids in physically hazardous situations. | |||
# Continued opioid use despite ongoing physical or psychological problem likely to have been caused or worsened by opioids. | |||
# Tolerance (i.e., need for increased amounts or diminished effect with continued use of the same amount) | |||
# Experiencing withdrawal (opioid withdrawal syndrome) or taking opioids (or a closely related substance) to relieve or avoid withdrawal symptoms<ref name=":0" /> | |||
</div></div> | |||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
As research has shown, there is a high correlation between drug abuse and mental disorders. | [[Image:Depression_opioid.JPG|350x300px|alt=|thumb|Depression]]As research has shown, there is a high correlation between drug abuse and [[Mental Health Challenges of Health Professionals in Times of COVID-19|mental disorders]]. <ref name="p0">National Institute on Drug Abuse. Comorbidity: Addiction and Other Mental Illnesses. https://www.drugabuse.gov/sites/default/files/rrcomorbidity.pdf (accessed 06 April 2016).</ref> The most common comorbidities associated with opioid use are anxiety and [[depression]] <ref name="p1" />.<br>Another frequent comorbidity associated with opioid use disorder is [[Chronic Pain|chronic pain]] <ref name="p2" />. The importance of screening an individual with chronic pain for substance use disorder is crucial; this way it can prevent any relapses with previously abused drugs like opioids or set up a strict plan for the individual using the drug <ref name="p2" />. | ||
== Treatment == | |||
Effective treatments are available, however, only about one in four people with opioid use disorder receive specialty treatment. Medication-assisted treatment is an effective treatment for individuals with an opioid use disorder. It involves use of medication along with counseling and behavioral therapies. Brain chemistry may contribute to an individual's mental illness as well as to their treatment. For this reason medications might be prescribed to help modify one's brain chemistry. Medications are also used to relieve cravings, relieve withdrawal symptoms and block the euphoric effects of opioids.<ref name=":0" /> | |||
# The disease is treated with opioid replacement therapy using buprenorphine or methadone, which reduces the risk of morbidity and mortality. | |||
# Naltrexone may be useful to prevent relapse. Naloxone is used to treat opioid overdose. Nonpharmacologic behavioral therapy is also beneficial. | |||
# Patients with opioid use disorder often benefit from twelve-step programs, peer support, and mental health professionals, individual and group therapy<ref name=":1" /> | |||
== | == Physical Therapy Management == | ||
Physical therapists are not qualified to manage opioid use disorders. Physical therapists should be able to recognize signs and symptoms of this disorder, but need to refer patients out for treatment. Physical therapists need to advocate for their patients to get them the treatment and help they deserve <ref name="p1" />. A recent review suggests physical therapy may promote use of nonpharmacological treatment model for musculoskeletal pain management thus indirectly helping reduce cases of opioid use disorders.<ref>George SZ, Goode AP. Physical therapy and opioid use for musculoskeletal pain management: competitors or companions?. Pain reports. 2020 Sep;5(5).https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7808685/ (Accessed on 18th October 2022)</ref>A retrospective study recommends early physical therapy for patients of low back pain, who are at risk of long term opioid use or misuse with avoidance of opioid prescription<ref>Fritz JM, King JB, McAdams-Marx C. Associations between early care decisions and the risk for long-term opioid use for patients with low back pain with a new physician consultation and initiation of opioid therapy. The Clinical journal of pain. 2018 Jun 1;34(6):552-8.https://pubmed.ncbi.nlm.nih.gov/29135698/<nowiki/>(Last accessed on 18th October 2022)</ref>. The attitude of physical therapists in managing patients with prescription opioid medication misuse (POMM) is related to how often they are engaged in treating them.<ref>Magel J, Cochran G, West N, Fritz JM, Bishop MD, Gordon AJ. Physical therapists’ attitudes are associated with their confidence in and the frequency with which they engage in prescription opioid medication misuse management practices with their patients. A cross–sectional study. Substance Abuse. 2022 Dec 1;43(1):433-41.https://pubmed.ncbi.nlm.nih.gov/34283690/<nowiki/>(Accessed on 18th October 2022)</ref> This will help not only to treat musculoskeletal issues like low back pain in such individuals but assist in early detection of opioid use disorder in many cases. Physical therapy interventions focusing on aerobic exercise in Opioid maintenance therapy (OMT) patients were found to be both feasible and beneficial<ref>ake-Schoffman DE, Berry MS, Donahue ML, Christou DD, Dallery J, Rung JM. Aerobic exercise interventions for patients in opioid maintenance treatment: a systematic review. Substance abuse: research and treatment. 2020 May;14:1178221820918885.https://pubmed.ncbi.nlm.nih.gov/35153484/<nowiki/>(Accessed on 18th October 2022)</ref>.<br>On March 15, 2016 the CDC released “Guideline for Prescribing Opioids for Chronic Pain” <ref name="p2" />. In these guidelines it promotes “nonpharmacological therapy and non opioid therapy as preferred treatment for chronic pain” <ref name="p2" />. The CDC found that physical therapy and exercise therapy had a high-quality of evidence to reduce pain and improve function <ref name="p2" />. In recent times the scope of physical therapy as a profession has grown for this disorder. Physical therapy now is included in the multidisciplinary team for prevention & management of opioid use disorder at community level<ref>Davenport TE, DeVoght AC, Sisneros H, Bezruchka S. Navigating the intersection between persistent pain and the opioid crisis: population health perspectives for physical therapy. Physical Therapy. 2020 Jun 23;100(6):995-1007.https://pubmed.ncbi.nlm.nih.gov/32115638/<nowiki/>(Accessed on 18th October 2022)</ref>. | |||
<br> | |||
== Case Reports == | |||
#Sullivan M, Edlund M, Fan M, DeVries A, Braden J, Martin B. Risks for Possible and Probable Opioid Misuse Among Recipients of Chronic Opioid Therapy in Commercial and Medicaid Insurance Plans: the TROUP Study. Pain. 2010 Aug; 150(2): 332–339. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2897915/ www.ncbi.nlm.nih.gov/pmc/articles/PMC2897915/] | |||
<br> | |||
== Case Reports | |||
#Sullivan M, Edlund M, Fan M, DeVries A, Braden J, Martin B. Risks for Possible and Probable Opioid Misuse Among Recipients of Chronic Opioid Therapy in Commercial and Medicaid Insurance Plans: the TROUP Study. Pain. 2010 Aug; 150(2): 332–339. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2897915/ www.ncbi.nlm.nih.gov/pmc/articles/PMC2897915/] | |||
#Niesters M, Overdyk F, Smith T, Aarts L, Dahan A. Opiod-induced respiratory depression in paediatrics: a review of case reports. Br. J. Anaesth. (2013) 110 (2): 175-182. [http://bja.oxfordjournals.org/content/110/2/175.short bja.oxfordjournals.org/content/110/2/175.short] | #Niesters M, Overdyk F, Smith T, Aarts L, Dahan A. Opiod-induced respiratory depression in paediatrics: a review of case reports. Br. J. Anaesth. (2013) 110 (2): 175-182. [http://bja.oxfordjournals.org/content/110/2/175.short bja.oxfordjournals.org/content/110/2/175.short] | ||
# | #Maloney E, Degenhardt L, Darke S, Mattick R, Nelson E. Suicidal behaviour and associated risk factors among opioid-dependent individuals: a case–control study. Addiction. December (2007) 102 (12) 1933–1941. [Http://onlinelibrary.wiley.com/doi/10.1111/j.1360-0443.2007.01971.x/full onlinelibrary.wiley.com/doi/10.1111/j.1360-0443.2007.01971.x/full] | ||
<div class="researchbox"> </div> | |||
<div class="researchbox"> | |||
</div> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
[[Category:Pharmacology]] | |||
[[Category:Pain]] | |||
[[Category:Older People/Geriatrics]] | |||
[[Category:Pharmacology for Older People]] | |||
Latest revision as of 08:00, 19 October 2022
Definition/Description[edit | edit source]
Opioid use disorder is the chronic use of opioids that causes clinically significant distress or impairment. Opioid use disorders affect over 16 million people worldwide and there are over 120,000 deaths worldwide annually attributed to opioids.[1] The opioid crisis was declared a nationwide Public Health Emergency in USA on Oct. 27, 2017[2].
Opioid use disorder consists of an overpowering desire to use opioids, increased opioid tolerance, and withdrawal syndrome when discontinued.
While opioid use disorder is similar to other substance use disorders in many respects, it has several unique features. Opioids can lead to physical dependence within a short time, as little as 4-8 weeks. In chronic users, the abruptly stopping use of opioids leads to severe symptoms, including generalized pain, chills, cramps, diarrhea, dilated pupils, restlessness, anxiety, nausea, vomiting, insomnia, and very intense cravings. Because these symptoms are severe it creates significant motivation to continue using opioids to prevent withdrawal.[1]
Opioids[edit | edit source]
Opioids are natural or synthetic (made in laboratories to mimic the properties of natural opioids) chemicals that interact with opioid receptors on the nerve cells in the body and brain and reduce feelings of pain. They are a class of drugs that include prescription pain relievers, synthetic opioids and heroin. Prescription opioids are meant to be used to treat acute pain (such as recovering from injury or post-surgery), chronic pain, active-phase cancer treatment, palliative care and end-of-life care. The main intended use is to reduce pain perception, but is associated with causing euphoria, drowsiness, mental confusion, nausea, constipation, and depress respiration (high doses) [2][3].Commonly used opioids identified in the healthcare setting include:
- Codeine
- Fentanyl (patch)
- Hydrocodone (Hysingla ER, Zohydro ER)
- Hydrocodone/Acetaminophen (Lorcet, Lortabe, Norco, Vicodin)
- Hydromorphone (Dilaudid)
- Methadone (Dolophine)
- Morphine (Avinza, Kadian)
- Oxycodone (OxyContin, Roxicodone)
- Oxycodone
- Naloxone [4]
Epidemiology[edit | edit source]
Over 16 million people worldwide are opioid-dependent and would meet the criteria for opioid use disorder, three million in the USA. Opioid use disorder results in over 120000 and 47000 deaths per year worldwide and in the U.S., respectively[1].Etiology[edit | edit source]
There is not one single cause that will lead someone to develop an opioid use disorder. Although, there are several factors that can increase the risk for developing an addiction including both individual and environmental [4]. Genetic factors have been found to play an important role for predisposition tendencies that can respond to the environment [4].
Opioids are known to activate the mesolimbic reward system which signals the release of dopamine causing feelings of pleasure. Our brains ability to establish this conditioned association is responsible for the desire to repeatedly use the drug [5]. However, the body is highly specialized to make adaptations to the presence of the drug and will transition from compulsion of seeking pleasure to depending on the drug existence entirely. Therefore, the increased compulsion is related to an individual tolerance and dependence of the drug [5].
Clinical Presentation[edit | edit source]
Opioids produce high levels of positive reinforcement, increasing the odds that people will continue using them despite negative resulting consequences. Opioid use disorder is a chronic lifelong disorder, with serious potential consequences including disability, relapses, and death. The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition describes opioid use disorder as a problematic pattern of opioid use leading to problems or distress, with at least two of the following occurring within a 12-month period:- Taking larger amounts or taking drugs over a longer period than intended.
- Persistent desire or unsuccessful efforts to cut down or control opioid use.
- Spending a great deal of time obtaining or using the opioid or recovering from its effects.
- Craving, or a strong desire or urge to use opioids
- Problems fulfilling obligations at work, school or home.
- Continued opioid use despite having recurring social or interpersonal problems.
- Giving up or reducing activities because of opioid use.
- Using opioids in physically hazardous situations.
- Continued opioid use despite ongoing physical or psychological problem likely to have been caused or worsened by opioids.
- Tolerance (i.e., need for increased amounts or diminished effect with continued use of the same amount)
- Experiencing withdrawal (opioid withdrawal syndrome) or taking opioids (or a closely related substance) to relieve or avoid withdrawal symptoms[2]
Associated Co-morbidities[edit | edit source]
As research has shown, there is a high correlation between drug abuse and mental disorders. [6] The most common comorbidities associated with opioid use are anxiety and depression [4].
Another frequent comorbidity associated with opioid use disorder is chronic pain [3]. The importance of screening an individual with chronic pain for substance use disorder is crucial; this way it can prevent any relapses with previously abused drugs like opioids or set up a strict plan for the individual using the drug [3].
Treatment[edit | edit source]
Effective treatments are available, however, only about one in four people with opioid use disorder receive specialty treatment. Medication-assisted treatment is an effective treatment for individuals with an opioid use disorder. It involves use of medication along with counseling and behavioral therapies. Brain chemistry may contribute to an individual's mental illness as well as to their treatment. For this reason medications might be prescribed to help modify one's brain chemistry. Medications are also used to relieve cravings, relieve withdrawal symptoms and block the euphoric effects of opioids.[2]
- The disease is treated with opioid replacement therapy using buprenorphine or methadone, which reduces the risk of morbidity and mortality.
- Naltrexone may be useful to prevent relapse. Naloxone is used to treat opioid overdose. Nonpharmacologic behavioral therapy is also beneficial.
- Patients with opioid use disorder often benefit from twelve-step programs, peer support, and mental health professionals, individual and group therapy[1]
Physical Therapy Management[edit | edit source]
Physical therapists are not qualified to manage opioid use disorders. Physical therapists should be able to recognize signs and symptoms of this disorder, but need to refer patients out for treatment. Physical therapists need to advocate for their patients to get them the treatment and help they deserve [4]. A recent review suggests physical therapy may promote use of nonpharmacological treatment model for musculoskeletal pain management thus indirectly helping reduce cases of opioid use disorders.[7]A retrospective study recommends early physical therapy for patients of low back pain, who are at risk of long term opioid use or misuse with avoidance of opioid prescription[8]. The attitude of physical therapists in managing patients with prescription opioid medication misuse (POMM) is related to how often they are engaged in treating them.[9] This will help not only to treat musculoskeletal issues like low back pain in such individuals but assist in early detection of opioid use disorder in many cases. Physical therapy interventions focusing on aerobic exercise in Opioid maintenance therapy (OMT) patients were found to be both feasible and beneficial[10].
On March 15, 2016 the CDC released “Guideline for Prescribing Opioids for Chronic Pain” [3]. In these guidelines it promotes “nonpharmacological therapy and non opioid therapy as preferred treatment for chronic pain” [3]. The CDC found that physical therapy and exercise therapy had a high-quality of evidence to reduce pain and improve function [3]. In recent times the scope of physical therapy as a profession has grown for this disorder. Physical therapy now is included in the multidisciplinary team for prevention & management of opioid use disorder at community level[11].
Case Reports[edit | edit source]
- Sullivan M, Edlund M, Fan M, DeVries A, Braden J, Martin B. Risks for Possible and Probable Opioid Misuse Among Recipients of Chronic Opioid Therapy in Commercial and Medicaid Insurance Plans: the TROUP Study. Pain. 2010 Aug; 150(2): 332–339. www.ncbi.nlm.nih.gov/pmc/articles/PMC2897915/
- Niesters M, Overdyk F, Smith T, Aarts L, Dahan A. Opiod-induced respiratory depression in paediatrics: a review of case reports. Br. J. Anaesth. (2013) 110 (2): 175-182. bja.oxfordjournals.org/content/110/2/175.short
- Maloney E, Degenhardt L, Darke S, Mattick R, Nelson E. Suicidal behaviour and associated risk factors among opioid-dependent individuals: a case–control study. Addiction. December (2007) 102 (12) 1933–1941. onlinelibrary.wiley.com/doi/10.1111/j.1360-0443.2007.01971.x/full
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Dydyk AM, Jain NK, Gupta M. Opioid use disorder. InStatPearls [Internet] 2021 Jul 12. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK553166/ (accessed 9.4.2022)
- ↑ 2.0 2.1 2.2 2.3 APA Opioid use disorder Available: https://www.psychiatry.org/patients-families/addiction/opioid-use-disorder(accessed 9.4.20220
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Substance Use Disorders. Substance Abuse and Mental Health Services Administration. 2015. Available at: http://www.samhsa.gov/disorders/substance-use. Accessed April 8, 2016.
- ↑ 4.0 4.1 4.2 4.3 4.4 American Psychiatric Association. Opioid Use Disorder Diagnostic Criteria. http://pcssmat.org/wp-content/uploads/2014/02/5B-DSM-5-Opioid-Use-Disorder-Diagnostic-Criteria.pdf Accessed 07 April 2016.
- ↑ 5.0 5.1 Goodman, CC, Snyder, TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. 5th ed. St. Louis, MO: Saunders/Elsevier; 2013. (Pg 49-51)
- ↑ National Institute on Drug Abuse. Comorbidity: Addiction and Other Mental Illnesses. https://www.drugabuse.gov/sites/default/files/rrcomorbidity.pdf (accessed 06 April 2016).
- ↑ George SZ, Goode AP. Physical therapy and opioid use for musculoskeletal pain management: competitors or companions?. Pain reports. 2020 Sep;5(5).https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7808685/ (Accessed on 18th October 2022)
- ↑ Fritz JM, King JB, McAdams-Marx C. Associations between early care decisions and the risk for long-term opioid use for patients with low back pain with a new physician consultation and initiation of opioid therapy. The Clinical journal of pain. 2018 Jun 1;34(6):552-8.https://pubmed.ncbi.nlm.nih.gov/29135698/(Last accessed on 18th October 2022)
- ↑ Magel J, Cochran G, West N, Fritz JM, Bishop MD, Gordon AJ. Physical therapists’ attitudes are associated with their confidence in and the frequency with which they engage in prescription opioid medication misuse management practices with their patients. A cross–sectional study. Substance Abuse. 2022 Dec 1;43(1):433-41.https://pubmed.ncbi.nlm.nih.gov/34283690/(Accessed on 18th October 2022)
- ↑ ake-Schoffman DE, Berry MS, Donahue ML, Christou DD, Dallery J, Rung JM. Aerobic exercise interventions for patients in opioid maintenance treatment: a systematic review. Substance abuse: research and treatment. 2020 May;14:1178221820918885.https://pubmed.ncbi.nlm.nih.gov/35153484/(Accessed on 18th October 2022)
- ↑ Davenport TE, DeVoght AC, Sisneros H, Bezruchka S. Navigating the intersection between persistent pain and the opioid crisis: population health perspectives for physical therapy. Physical Therapy. 2020 Jun 23;100(6):995-1007.https://pubmed.ncbi.nlm.nih.gov/32115638/(Accessed on 18th October 2022)