Meniere's Disease: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="noeditbox">Welcome to [[Pathophysiology of Complex Patient Problems|PT 635 Pathophysiology of Complex Patient Problems]] This is a wiki created by and for the students in the School of Physical Therapy at Bellarmine University in Louisville KY. Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!</div><div class="editorbox"> | ||
'''Original Editors '''- [[Pathophysiology of Complex Patient Problems|Mary Glorighian & Mercedes Nelson from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | '''Original Editors '''- [[Pathophysiology of Complex Patient Problems|Mary Glorighian & Mercedes Nelson from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
| Line 305: | Line 305: | ||
#Rehabilitate patients after destructive treatments that result in static unilateral or bilateral vestibular loss. | #Rehabilitate patients after destructive treatments that result in static unilateral or bilateral vestibular loss. | ||
#Treat the “spin-offs” of Meniere’s disease ([http://www.dizziness-and-balance.com/treatment/rehab/menieresPT.html see the notes by Timothy Hain MD]): | #Treat the “spin-offs” of Meniere’s disease ([http://www.dizziness-and-balance.com/treatment/rehab/menieresPT.html see the notes by Timothy Hain MD]): | ||
##Visual dependence for balance | ##Visual dependence for balance | ||
##Neck stiffness caused by a common balance coping strategy | ##Neck stiffness caused by a common balance coping strategy | ||
##Depression and anxiety<br> | ##Depression and anxiety<br> | ||
| Line 381: | Line 381: | ||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed])<br> == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed])<br> == | ||
<div class="researchbox"><rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1b9VCa6FcviVo_Dc47KkOT1460XlsI0RFlc7fJJBRtuc0lxMzT|charset=UTF-8|short|max=10</rss></div> | <div class="researchbox"><rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1b9VCa6FcviVo_Dc47KkOT1460XlsI0RFlc7fJJBRtuc0lxMzT|charset=UTF-8|short|max=10</rss></div> | ||
== References == | == References == | ||
Revision as of 15:52, 12 February 2017
Original Editors - Mary Glorighian & Mercedes Nelson from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Mercedes Nelson, Mary Glorighian, Deborah Bruckman, Lucinda hampton, Tony Lowe, Kim Jackson, Elaine Lonnemann, Admin, Vidya Acharya, Wendy Walker, Hayley Lawler, 127.0.0.1, Mande Jooste, Aminat Abolade, Laura Ritchie, Scott Buxton, Naomi O'Reilly, Magdalena Hytros, WikiSysop and Uchechukwu Chukwuemeka
Definition/Description[edit | edit source]
Also known as endolymphatic hydrops, Ménière's disease is a disorder that affects the semicircular canals and cochlea (collectively known as the labyrinth) of the inner ear. These canals help to interpret the bodies position in space and help to maintain balance. [1] [2]
Prevalence[edit | edit source]
- There are 200 cases/100,000 persons in the United States (or about 0.2 % of the population). [1]
- The National Institute on Deafness and Other Communication Disorders (NIDCD) estimates that approximately 615,000 individuals in the United States are currently diagnosed with Ménière’s disease and that 45,500 cases are newly diagnosed each year. [4]
- Ménière’s disease can develop at any age, but it is more likely to happen to adults between 40 and 60 years of age. [4]
- The prevalence of Ménière disease varies between ethnicites internationally. [1]
In a study performed in Framingham, MA, 1.48 % of the population claimed to have a history of Ménière’s disease. This large prevalence figure likely derives from a tendency of many physicians to lump all cases of recurrent vertigo into the category of Ménière’s disease. Mayo Clinic reported prevalence in 1980 in the Rochester, MN population of 218.2 cases/100,000 people, and an incidence rate of new cases of 15.3/100,000 per year. They also reported a diagnosis rate basically proportional to age up to the age of 60, with a decline thereafter. Ménière’s disease in the ears bilaterally was found in 34% of their group.[1]
Etiology/Causes [edit | edit source]
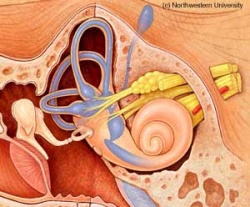
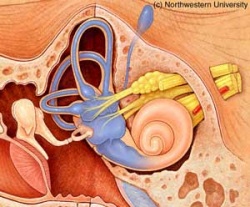
This disorder has an unknown cause but is thought to be due to increased fluid pressure in the inner ear. The pressure stretches the membranes that divide the inner ear. This stretching causes tinnitus and a decrease in ability to hear. The rupture of these membranes and the mixture of fluids with different concentrations is thought to lead to vertigo. This repeated process of rupturing and healing is what is thought to cause the eventual loss of ability to hear low frequencies.[5]
 [1]
[1]
Normal Labyrinth Dilated Labyrinth- such as in Ménière's
It may be related to:[2]
- Head Injury
- Middle or Inner Ear Infection
Risk Factors Include:[2]
- Allergies
- Alcohol Use
- Family History
- Fatigue
- Recent Viral Illness
- Respiratory Infection
- Smoking
- Stress
- Use of Certain Medications
Characteristics/Clinical Presentation[edit | edit source]
Fullness in the Ear [6]
Fullness in one ear is typically the first symptom experienced preceding an acute attack. This feeling is similar to what is felt when changing altitudes (such as in an airplane) but cannot be relieved by swallowing.
Vertigo[6]
This is the main symptom of Ménière's disease and is commonly the most debilitating part of an attack. This feeling of dizziness can last anywhere from 20 minutes to a few days, with the average attack being two to four hours. During an attack of vertigo, the room seems to be spinning and the person feels imbalanced. This sensation may produce nystagmus(beating of the eyes from side to side), nausea, vomiting or sweating. An attack of vertigo, unlike common feeling of spinning can persist with a constant intensity or may gradually increase in intensity.
Recurrent vertigo often affects patients' daily activities even during periods of remission. The episodes often force a person to lie down for several hours and lose time from work or leisure activities, if they have to climb ladders or operate machinery. Vertigo can increase risk of falls, accidents while driving a car or operating heavy machinery.[7]
Tinnitus[6]
Tinnitus is a sustained, loud ringing or buzzing in the ears. The intensity of this may vary, but the symptom is continual in people diagnosed with Ménière's.
Fluctuations in hearing[6]
This hearing loss usually affects one ear. The person will have a decline in ability to hear during an attack but will regain hearing when current episode has ended. When a person has had Ménière's for a prolonged period, this hearing loss may not resolve as it did previously. Low frequency tones are most frequently lost, but all tones may be affected as the disease process progresses.
Other Symptoms[2]
- Diarrhea
- Headaches
- Pain/discomfort in the abdomen
- Uncontrollable Eye Movements
Associated Co-morbidities[edit | edit source]
It has been suggested that there may be a link between Ménière’s disease and joint disease of the jaw (temporomandibular joint), the cervical spine, Eustachian tube dysfunction, and autonomic nervous system dysfunction.[8]
An increased prevalence of migraine in patients with Menière’s disease (MD) is well documented. Migraine was twice as high in a group of 78 patients with unilateral or bilateral MD (based on the American Academy of Otolaryngology criteria), than in an age- and sex-matched control group (56% vs. 25%, p<0.001). Migraine leads to a greater susceptibility of developing MD, as suggested by a study in which MD patients had an earlier onset of symptoms and a greater frequency of bilateral hearing loss when they also had migraine. [9]
Vertigo can also cause emotional stress in patients with Menière's disease. These patients often avoid a wide range of situations and activities for fear of provoking or experiencing a sudden attack. Due to MD's unpredictability, patients with Menière's disease also have depression or anxiety in dealing with the disease. Experts are not sure whether stress/anxiety cause symptoms or whether they are caused by the disease. However, some studies indicate that good stress and anxiety management may help lessen the intensity of symptoms. Professional psychotherapy and some medications have been known to help many patients with Ménière’s disease.[10]
Systemic Involvement[edit | edit source]
Immunologic function of the endolymphatic sac has been analyzed and it is found that immune disease may contribute to a substantial percentage of Ménière’s disease. Reports of Ménière’s disease associated with thyroid autoimmune disease, allergies and elevated levels of immune complexes and activated lymphocytes may be due to an abnormal immune response. Others have reported that there is an association of viral infection with the development of Ménière’s, but results have been conflicting. Individuals with certain auto immune disorders such as lupus and severe rheumatoid arthritis, or who suffer from thyroid disorders such as Grave's disease and Hashimoto's thyroiditis may be at higher risk for developing Ménière’s disease.[8]
Diagnostic Tests/Lab Tests/Lab Values
[edit | edit source]
Ménière’s disease is most often diagnosed and treated by an otolaryngologist (commonly called an ear, nose, and throat doctor, or ENT). However, there is no definitive test or single symptom that a doctor can use to make the diagnosis. [4]
Diagnosis is based upon medical history and the presence of:[7]
• Two or more spontaneous episodes of vertigo lasting at least 20 minutes each
• Tinnitus or aural fullness
• Temporary hearing loss verified by a hearing test on at least one occasion
• Exclusion of other known causes of these sensory problems
The physician may ask questions about:[7]
• Patient's history of infectious diseases or allergies
• The severity, duration and frequency of the sensory problems
• Medication use
• Past ear problems
• Patient's general health
• History of inner ear problems in patient's family
Initial evaluation is based on a very careful history given to the otolaryngologist, as well as an examination of the ears under the operating microscope to rule out obvious infections or visible growths. A physical examination of the ears, head and neck, and the part of the nervous system related to balance is performed. A brain and nervous system (neurological) examination may show problems with hearing, balance, or eye movement. Comprehensive hearing and balance tests are performed.[5]
Hearing tests may include:[7][11]
• Audiogram (basic hearing test) assesses how well sounds are detected at different pitches and volumes and how well similar-sounding words are distinguished. The test not only reveals the quality of hearing but also may help determine if the source of hearing problems is in the inner ear or the nerve that connects the inner ear to the brain. A low frequency up sloping hearing loss of the neural type noted on the hearing test is typical of Ménière’s.
• Electrocochleography (ECOG), similar to the Brainstem Evoked Response Audiometry, measures the response of the inner ear to sound stimuli introduced to the external auditory canal or middle ear. ECOG measures the excess fluid accumulation in the inner ear. In Ménière’s, this test will also confirm increased pressure due to excess fluids in the inner ear.
• Dehydration tests administering glycerol are used to reduce fluid in the ear and any resultant changes in eharing are measured by an audiogram.
The visual and vestibular systems interact with each other to maintain visual clarity of objects during head movement. Head movement or other stimulation of the inner ear sends signals to the muscles of the eyes via the nervous system, which is called the vestibulo-ocular reflex (VOR). The VOR normally generates eye movements that maintain clear vision with head movement. Balance tests are used to determine which ear is affected, assess the level of balance lost, and assess the brain’s compensation for the damage in the ear.[12]
Balance tests include:[7] [1] [5] [12]
• Electronystagmography (ENG) is a group of eye-movement tests that look for signs of vestibular dysfunction or neurological problems by measuring nystagmus (a type of involuntary eye movements). During ENG, eye movements are recorded and analyzed via small electrodes placed on the skin around the eyes. The electrodes attach to the skin with an adhesive, much like a small bandage. One ENG test evaluates the movement of the eyes as they follow a moving target. Another observes eye movements as the head is positioned in different directions. Finally, caloric testing analyzes eye reflexes. It involves stimulating the horizontal semicircular canal in the inner ear by introducing warm or cold water (or air) into the outer ear canal and recording the resulting eye movements. Abnormal results can be a sign of Ménière’s disease.
• Videonystagmography (VNG) is similar to ENG, except that eye movements may be recorded by an infrared video camera mounted inside the goggles that the patient wears instead of sticky-patch electrodes.
• Harmonic acceleration tests (rotary-chair testing), like an ENG, measures inner ear function based on eye movement. Stimulus to the inner ear is provided by movement of a special rotating chair precisely controlled by a computer, with the lights turned off, and checking to see if the inner ear is detecting the rotation.
• Vestibular evoked myogenic potentials (VEMP) testing measures the function of sensors in the vestibule of the inner ear that help detect acceleration movement. These sensors also have a slight sensitivity to sound. When these sensors react to sound, tiny measurable variations in neck muscle contractions occur. These contractions serve as an indirect measure of inner ear function.
• Posturography is a computerized test that provides information about motor control or balance function under varying environmental conditions. The patient wears a safety harness and tries to keep their balance on a platform under various conditions barefoot.
Additional testing to rule out other conditions:[7]
• Brainstem Evoked Response Audiometry (BSER) or Auditory Brainstem Response (ABR) is a computerized test of the hearing nerves and hearing centers of the brain. It can help detect the presence of a tumor disrupting the function of auditory nerves. It will usually be normal despite the hearing loss, unless a central disorder is present.
• Magnetic Resonance Imaging (MRI) with a contrast dye called Gadolinium can rule out an acoustic neuroma or other brain tumor as a possible source of symptoms. The MRI with Gadolinium specifically visualizes the eighth nerve (acoustic and balance nerve). Some older scanners can miss a small acoustic neuroma (tumor). Newer MRIs can actually visualize the structures of the inner ear including the cochlea and semicircular canals, which is most helpful. The eighth nerve can be clearly identified on MRI scan. A nerve that does not show enhancement (increase in brightness) when the dye is given, rules out an acoustic neuroma from the diagnosis.
• Computerized tomography (CT) to determine whether there are abnormal masses in the head and brain.
•Lab tests should include examination for inner ear immune related infections or conditions. Syphilis can involve the inner ear even twenty to thirty years after the original infection. Lyme disease can also produce Ménière’s-like symptoms, and symptoms can surface months after the original infection.
Once testing is completed, the otolaryngologist can evaluate the results, rule out extraneous conditions and confirm the diagnosis of Ménière’s disease. Even after this extensive testing, the test results may not be conclusive.[5]
Differential Diagnosis[edit | edit source]
Other conditions can produce the same symptoms as Ménière’s disease and must be ruled out in order to develop an accurate diagnosis. The differential diagnosis is broad and includes perilymph fistula, recurrent labyrinthitis, migraine, congenital ear malformations of many kinds, multiple sclerosis, posterior fossa arachnoid cysts, and other rare entities. Symptoms similar to Ménière’s (fluctuating hearing, tinnitus, vertigo) can also be caused by impending strokes in the distribution of the anterior inferior cerebellar artery. Hearing fluctuation bilaterally suggests a vascular cause such as migraine. Occasionally a "wrong way" nystagmus is seen in Ménière’s disease. This is a highly specific finding to Ménière’s disease, as few other conditions have an excitatory phase. [1]
Infections of the inner ear, such as syphilis and Lyme disease, may produce episodes of vertigo and hearing loss quite indistinguishable from Ménière’s, which usually occur in both ears. Tumors of the inner ear nerve (the eighth nerve), especially acoustic neuromas, can also produce similar symptoms. These tumors grow slowly and compress the nerve. However, the hearing loss doesn't have periods of improvement and the patient usually experiences imbalance rather than vertigo. Cholesteatomas (cystic growths) and other infections of the middle ear can also produce symptoms similar to Ménière’s. Ten to fifteen percent of cases resembling Ménière’s disease may be the result of an immune disorder of the body, the system producing antibodies which attack the inner ear.[5]
Medications[edit | edit source]
Medications prescribed for Ménière's disease are typically used to treat individual symptoms because no cure has been found.
Medications to control dizziness and vestibular disturbances are typically used during an acute attack to relieve the person of some discomfort.
Some commonly used medications are:
- Meclizine
- Diazepam
- Lorazepam
- Clonazepam
Anti-Nausea Medications[1]
Medications to control nausea or motion-sickness are commonly used to relieve these symptoms associated with vestibular upset.
Commonly Used Anti-Nausea:
- Phenergan
- Compazine
- Ondansetron
Diuretics[1]
The exact cause of effectiveness with diuretics in reducing vestibular complaints is uncertain. The mechanism is thought to be a reduction in the fluid volume within the ear. People taking diuretics may need to take potassium supplements due to potassium loss associated with increased fluid excretion.
- Dyazide is the most commonly prescribed in the United States.
Other Diuretics include:
- Moduretic
- Diamox
- Amiloride
- Ethacrynic Acid
- Spironolacetone
- Tiamterine
Middle Ear Injections[7]
- Gentamicin is an antibiotic that is toxic to the ear. It is injected to reduce the balance function in the affected ear therefore reducing severity of the vertigo attack. The unaffected ear assumes the responsibility for balance. There is a risk of further hearing loss with this treatment.
- Steroids such as dexamethasone can be used to control vertigo attacks. It may be less effective than Gentamicin but is less likely to result in hearing loss.
Calcium Channel Blockers[1]
The method of treatment with these drugs is not fully understood. It ha been shown that some people with Ménière's have elevated calcium levels.
Commonly Used for Ménières:
- Verapamil
- Nimodipine
- Flunarizine (Not available in USA)
Immunosupressants[1]
If there is a significant improvement with the use of steroids, the symptoms of Ménières may be caused by autoimmune disorder, so a bout of immunosupressants may be tried.
Common Immunosupressants:
- Methotrexate
- Steroids
- Enbrel
- Humira
Medical Management (current best evidence)[edit | edit source]
- Salt restriction helps to reduce excess fluid in ears over time. This helps to limit attacks.
- Caffiene stimulates nerves and can affect ménière's, so a reduction in caffiene can be helpful.
- Smoking constricts the blood vessels and restricts blood flow to the nerve endings.
- Keeping stress and anxiety levels low can also help to prevent attacks. Fear of an attack could be an added stress that the person will want to learn to control.
Medication
See medication section
Hearing Aid[2]
Hearing aids can be useful in patients with ménière's that have progressive hearing loss. Hearing aids can help the person hear to the best of their ability for as long as possible.
Meniett Device[13]
The Meniett® Low-Pressure Pulse Generator device is a safe, simple, and effective treatment for the vertigo symptoms of Ménière's disease. The Meniett device delivers a computer-controlled, complex algorithm of micropressure pulses that are transmitted to the middle ear space and act on the oval and round windows. It is believed that the energy of the Meniett's micropressure pulses causes a displacement of the perilymphatic fluid, which stimulates the flow of endolymphatic fluid and reduces it, thus relieving the symptoms of Ménière's disease. The Meniett device is based on nearly 30 years of clinical research in the US and abroad. Short- and long-term results have been studied in patients with Ménière's disease, including placebo-controlled trials.
Advantages of Meniett Therapy
- May help reduce the frequency and intensity of vertigo attacks
- Helps some patients avoid serious surgical or destructive procedures
- Safe and minimally invasive Ménière’s disease treatment
- Developed and tested over nearly 30 years of clinical research
- Easy for patients to do and puts them in control of their Ménière's disease
- Portable and convenient therapy just takes a few minutes each day
- Other Ménière's disease treatments may still be employed, if necessary
- Full refund within 6 weeks if patient’s Ménière's disease doesn’t respond to Meniett therapy
Disadvantages of Meniett Therapy for Ménière's Disease
- Slight risk of infection from tympanostomy tube
- Not reimbursed by all insurance providers
- Ménière's disease is not responsive to Meniett therapy in a small portion of the population
A study discussed the possibility of low pressure Meniett therapy allowing avoidance of the surgical procedure, vestibular neurectomy, in thirty six patients with Ménière’s disease (MD) that have recurring episodes of vertigo. Twenty-five patients (69.4%) were treated satisfactorily by using Meniett treatment and therefore avoided vestibular neurectomy. In half of them only one cycle of treatment was necessary. Better results are shown when pressure treatment is performed on patients with MD of short duration.[14]
Surgeries[5]
- Endolymphatic sac procedures- This procedure is performed by making an incision behind the ear. The endolymphatic sac is exposed and a valve is inserted for future drainage. This surgery should allow the inner ear to re-equilibrate and take pressure off of the nerve endings. Vertigo symptoms subside in about 70% of patients after surgery but recur with this same severity within three years in a significant number of individuals.
- Vestibular neurectomy- If the patient still has substantial hearing this may be the preferred surgery. The vestibular nerve is sectioned near its origin at the brain, therefore preserving the hearing portion. This surgery cures vertigo 90-95% of the time.
- Labyrinthectomy- In a labyrinthectomy, an incision is made behind the ear as in the enolymphatic sac draining procedure but the labyrinth is exposed in this procedure. The semicircular canals are carefully drilled away and the nerve inside is removed. Patients experience vertigo for one to two days after the surgery then slowly beginto regain their balance as the other ear takes over balance functioning. This surgery does not preserve hearing and the other ear may begin to have problems later in the persons lifetime.
Physical Therapy Management (current best evidence)[edit | edit source]
Despite the fact that physical therapy cannot address the underlying cause of Ménière’s disease physiotherapy management can assist patients in several ways[15]
- Improve baseline balance
- Educate patients how to avoid injury due to imbalance or vertigo
- Rehabilitate patients after destructive treatments that result in static unilateral or bilateral vestibular loss.
- Treat the “spin-offs” of Meniere’s disease (see the notes by Timothy Hain MD):
- Visual dependence for balance
- Neck stiffness caused by a common balance coping strategy
- Depression and anxiety
For patients experiencing problems with balance between episodes of vertigo, they may benefit from vestibular rehabilitation therapy. This therapy may include exercises and activities that the patients perform during therapy sessions and at home. Vestibular rehabilitation helps their body and brain regain the ability to process balance information correctly. [7]
One study discussed the evaluation and treatment plan for a 68 year old female diagnosed with Ménière’s disease. The plan consisted of vestibular rehabilitation including adaptation, substitution, and habituation exercises. Neuromuscular education was performed involving static and dynamic balance exercises and the treadmill was used to normalize gait. The treatment plan for this female usually lasted 50 to 60 minutes, but was shorter sometimes if she was experiencing symptoms early on in the treatment process. Adaptation and substitution exercises were performed as a home exercise program with business or index cards used as targets. Adaptation exercise treatment progression involved the use of complex of backgrounds. Habituation exercises included forward bending to decrease vertigo. Static balance exercises involved eyes open or eyes closed, changes in base of support, vertical or horizontal head movements in Romberg, sharpened Romberg, or single leg stance. Uneven surfaces were utilized also. Dynamic balance exercises included walking with vertical or horizontal head movements, modified or tandem ambulation forward and backward, walking with ball passes, tosses, or kicking. [16]
Home Modification Ideas[16]
Patients recovering from balance disorders require a safe environment at home, as In the clinic. To help safeguard against dangerous falls, suggest the following household improvements:
- Add grab bars to the shower or tub, both horizontal and vertical ones
- Add a shower or tub seat
- Add anti-slip strips in showers or tubs
- Consider an elevated toilet seat
- Add ramps and reduce threshold heights in doorways tor anyone on wheels (rolling walkers, wheelchairs, scooters, etc)
- Add handrails or secure hand holds at steps or stairs
- Place risers or blocks under the legs ot couches or chairs
- Remove throw rugs throughout the house
- Clear out clutter. Set a goal to clear a pathway 36 inches wide, which leaves enough room to easily handle a walker or wheelchair
- Add light sensor night-lights in hallways and bathrooms
- Add motion-sensor alarms that alert care providers when loved ones start to get out ot bed
- Carry small loads, as heavy ones throw ott your balance
- Keep items you use often in easy-to-reach places
Case Reports/ Case Studies[edit | edit source]
Case report: a case of intractable Meniere's disease treated with autogenic training
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2265298/
The Role of Vestibular Rehabilitation in treating Ménière's Disease
http://www.ptproductsonline.com/issues/articles/2011-08_04.asp
A 69-Year-Old Man with Chronic Dizziness
http://jama.ama-assn.org/content/280/24/2111.extract
A 69-Year-Old Man with Chronic Dizziness, 1 Year Later
http://jama.ama-assn.org/content/282/4/378.extract
Resources
[edit | edit source]
Directory of Organizations
http://www.nidcd.nih.gov/directory/keyword.asp?keyword49=49
Information on vestibular disorders for patients and health professionals, support group, and book: Ménière’s Disease : What you need to know by P.J. Haybach, Jerry Underwood.
Information on Ménière’s disease
http://www.american-hearing.org/disorders/menieres-disease/
Ménière’s disease information and doctor who treats patients with Ménière’s disease: Indianapolis, Indiana: Midwest Ear Institute. George W. Hicks, M.D. (Dispenses the Meniett device.)
http://www.menieresinfo.com/doctors.html
American Academy of Otolaryngology — Head and Neck Surgery website to help patients find an ENT
Coping information and support group for patients
http://www.menieresresources.org/
Support group and forum for patients with Ménière’s disease
Recent Related Research (from Pubmed)
[edit | edit source]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Hain T. Dizziness-and-balance.com. Ménière’s disease [internet]; 2011 Nov 11 [updated 2011 Nov 30; cited 2012 Mar 15]. Available from: http://www.dizziness-and-balance.com
- ↑ 2.0 2.1 2.2 2.3 2.4 PubMed Health. Ménière’s Disease [internet]. Bethesda, MD: A.D.A.M. Inc., National Center for Biotechnology Information, U.S. National Library of Medicine; 2012 [updated 2011 Aug 31; cited 2012 Mar 15]. Available from: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001721/
- ↑ Gibson B. YouTube. menieresresearch; 2010 [updated 2010 Apr 27; cited 2012 Apr 4]. Available from: http://www.youtube.com/watch?v=TFksAtUpTfg
- ↑ 4.0 4.1 4.2 National Institute on Deafness and Other Communication Disorders. Ménière’s disease [internet]; [updated 2010 July; cited 2012 Mar 15]. Available from: http://www.nidcd.nih.gov/health/balance/pages/meniere.aspx/ Cite error: Invalid
<ref>tag; name "NIDCD" defined multiple times with different content - ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Levenson M. Ménière’s Disease [internet]. Saratoga Springs, NY: The Ear Surgery Information Center; 2011 [cited 2012 Mar 15]. Available from http://www.earsurgery.org/site/pages/conditions/menieres-syndrome.php
- ↑ 6.0 6.1 6.2 6.3 Salt AN. The Department of Otolaryngology [Internet];St. Louis:Washington University School of Medicine; 2005 [updated 2005 November; cited 2012 Apr 4]. Available from: http://oto2.wustl.edu/men/
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 7.9 Mayo Clinic. Ménière’s Disease [internet]. Mayo Foundation for Medical Education and Research (MFMER); 2012 Aug 11 [updated 2011 Aug 2; cited 2012 Mar 15]. Available from: http://www.mayoclinic.com/health/menieres-disease/DS00535
- ↑ 8.0 8.1 Hain T. American Hearing Research Foundation. Ménière’s disease [internet]; [updated 2008 Oct; cited 2012 Mar 15]. Available from: http://www.american-hearing.org/disorders/menieres-disease/
- ↑ Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and vestibular migraine. Journal of Neurology. 2009; 256 (3):333-338.
- ↑ Medical News Today. What Is Ménière’s Disease? What Causes Ménière’s Disease? [internet]; 2009 Sept 15 [cited 2012 Mar 15]. Available from http://www.medicalnewstoday.com/articles/163888.php
- ↑ Ménière’s Australia. Diagnosis of Ménière’s Disease [internet]. Frankston, VIC: Ménière’s Australia; 2004 – 2012 [updated 2012 Mar; cited 2012 Mar 15]. Available from: http://www.menieres.org.au/diagnosis.php
- ↑ 12.0 12.1 Vestibular Disorders Association. Ménière’s Disease [internet]. Portland, OR; [updated 2011 Mar 11; cited 2012 Mar 15]. Available from: http://www.vestibular.org/
- ↑ Medtronic. Menniett Device for Ménière’s Disease [internet]. Medtronic Inc.; 2012 [updated 2012 Jan 24; cited 2012 Mar 15]. Available from: http://www.medtronic.com/
- ↑ Barbara M, Monin S, Chiappini I, Filipo R. Meniett therapy may avoid vestibular neurectomy in disabling meniere's disease. Acta Oto-Laryngologica. 2007; 127: 1136-1141.
- ↑ Hain, T. C., 2008 Physical Therapy for Meniere's Disease, accessed 13/03/2015
- ↑ 16.0 16.1 Babb R, Hafner W. Balancing act - the role of vestibular rehabilitation in treating meniere's disease. PTProductsOnline.com. 2011; 20-23.






