Liver Function Tests
Introduction[edit | edit source]
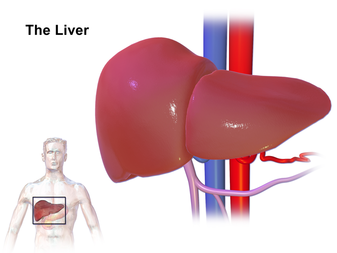
Liver Function Tests (LFTs) are used to screen for, detect, evaluate and monitor acute and chronic liver inflammation (hepatitis), infection, liver disease and/or damage. The liver is one of the largest organs in the body and is located in the upper right-hand part of the abdomen and behind the lower ribs.
The liver has several functions including eg: primary detoxification of various metabolites; synthesizing proteins; producing digestive enzymes; a role in metabolism; regulation of red blood cells; glucose synthesis and storage; vitamin and mineral storage.[1] [2].
- The liver function tests are one of the most commonly ordered laboratory tests. Mild isolated elevations in LFTs can be seen as normal fluctuations and should not trigger expensive and extensive workup.
- The term “liver function tests“ is a misnomer as many of the tests do not comment on the function of the liver but rather pinpoint the source of the damage.
- Physicians need be aware of various conditions that can lead to an elevation in LFTs.[1]
What LFTs Reveal[edit | edit source]
A variety of diseases and infections can cause acute or chronic damage to the liver, causing inflammation, scarring, bile duct obstructions, clotting abnormalities, and liver dysfunction. Alcohol, drugs, some herbal supplements, and toxins can also pose a threat. A significant amount of liver damage may be present before symptoms such as jaundice, dark urine, light-coloured stools, pruritus, nausea, fatigue, diarrhoea, and unexplained weight loss or gain emerge. Early detection is essential in order to minimize damage and preserve liver function.
LFTs measure enzymes, proteins, and substances that are produced or excreted by the liver and are affected by liver injury. Some are released by damaged liver cells and some reflect a decrease in the liver's ability to perform one or more of its functions. When performed together, these tests give the doctor a snapshot of the health of the liver, an indication of the potential severity of any liver injury, change in liver status over time, and a starting place for further diagnostic testing[2]
Etiology and Epidemiology[edit | edit source]
Elevated LFTs are found in approximately 8% of the general population. These elevations may be transient in patients without symptoms with up to 30% elevations resolving after 3 weeks. ie care should be taken when interpreting these results to avoid unnecessary testing[1]
Significance[edit | edit source]
The levels of LFTs can point to the differentials. Many disease processes have very distinct abnormalities in the liver enzymes.
Differentials include:
- Several medications are known to cause liver damage. eg.Many of these are commonly used in daily practice including but not limited to NSAIDs, antibiotics, statins, anti-seizure drugs, antifungals such as ketoconazole, antibiotics such as tetracyclines and drugs for tuberculosis treatment.
- Alcoholism eg Liver fibrosis can also be seen as secondary to chronic alcohol intake
- Fatty liver disease can cause chronic hepatic disease as well as hepatocellular carcinoma. The typical patient with this disease is overweight, has type II diabetes, or has dyslipidemia and no evidence of clinically significant alcohol use
- Viral Hepatitis: Viral illnesses are a common cause of hepatitis and elevation in LFTs. Viral hepatitis B, C, and D can cause chronic hepatitis; hepatitis A and E cause acute viral hepatitis. Several other viruses including HIV, Epstein-Barr (EBV) and Cytomegalovirus (CMV) can also cause hepatitis.
- Hemochromatosis is the abnormal accumulation of iron in parenchymal organs, leading to organ toxicity. It is the most common autosomal recessive genetic disorder and the most common cause of severe iron overload.
- Autoimmune hepatitis is a chronic disease that is characterized by continuing hepatocellular inflammation and necrosis and a tendency to progress to cirrhosis.
- Wilson disease, a rare autosomal-recessive inherited disorder of copper metabolism, is characterized by excess copper deposition in the liver, brain, and other tissues. It is fatal if not recognized and treated early.
- Alpha-1 antitrypsin deficiency (AATD) is a relatively common yet often undiagnosed genetic condition. Those with AATD are also predisposed to obstructive pulmonary disease and liver disease
Components of Liver Function Tests[edit | edit source]
- Alanine aminotransferase (ALT) – an enzyme mainly found in the liver; the best test for detecting hepatitis
- Alkaline phosphatase (ALP) – an enzyme related to the bile ducts; often increased when they are blocked
- Aspartate aminotransferase (AST) – an enzyme found in the liver and a few other places, particularly the heart and other muscles in the body
- Total bilirubin – measures all the yellow bilirubin pigment in the blood. Another test, direct bilirubin, measures a form combined with another compound in the liver and is often requested with total bilirubin in infants with jaundice.
- Albumin – measures the main protein made by the liver and tells whether or not the liver is making an adequate amount of this protein
- Gamma-glutamyl transferase (GGT) - an enzyme found mainly in the liver and is a useful marker for detecting bile duct problems
- Total protein - measures albumin and all other proteins in blood, including antibodies made to help fight off infections
| Alanine Transaminase (ALT); Normal value: 0-45 IU/L
Aspartate Transaminase (AST); Normal value: 0-35 IU/L[3] |
|---|
Causes of raised transaminases:
|
| Alkaline phosphatase (ALP); Normal value: 30–120 IU/l[3] |
|---|
Causes of raised ALP:
|
| Gammaglutamyl transferase (GGT); Normal value: 0 to 30 IU/L[3] |
|---|
Causes of raised GGT:
|
| Bilirubin; Normal value: 2 to 17 micromoles/L[3] |
|---|
Causes of isolated hyperbilirubinemia:
|
| Prothrombin time; Normal value: 10.9 to 12.5 seconds[3] |
|---|
Causes of prolonged prothrombin time:
|
| Albumin; Normal value: 40 to 60 g/L[3] |
|---|
| With progressive liver disease serum albumin levels fall, reflecting decreased synthesis. Albumin levels are dependant on a number of other factors such as the nutritional status, catabolism, hormonal factors, and urinary and gastrointestinal losses.[4] |
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Lala V, Goyal A, Bansal P, Minter DA. Liver function tests. StatPearls [Internet]. 2020 Jul 4.Available from: https://www.ncbi.nlm.nih.gov/books/NBK482489/(accessed 27.3.2021)
- ↑ 2.0 2.1 Lab tests inline LFTs Available from: https://www.labtestsonline.org.au/learning/test-index/liver-function(accessed 27.3.2021)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Lala V, Goyal A, Bansal P, Minter D. Liver function tests. StatPearls. 2020 Apr 28.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Limdi JK, Hyde GM. Evaluation of abnormal liver function tests. Postgraduate medical journal. 2003 Jun 1;79(932):307-12.
- ↑ MedCram - Medical Lectures Explained CLEARLY. Liver Function Tests (LFTs) Explained Clearly by MedCram.com. Available from: https://www.youtube.com/watch?v=bFdTgty0T0I [Last accessed 29 November, 2020]